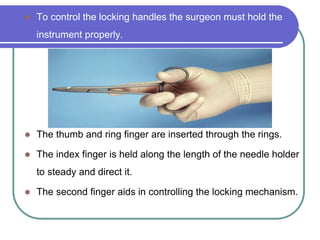
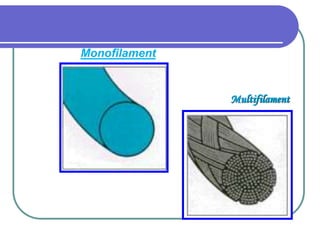
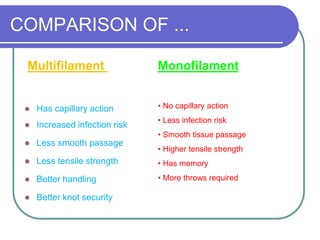
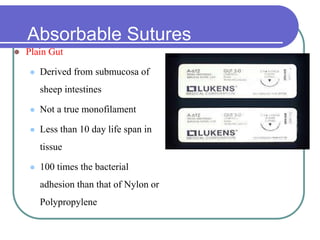
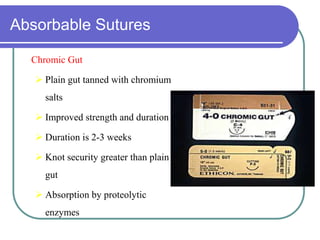
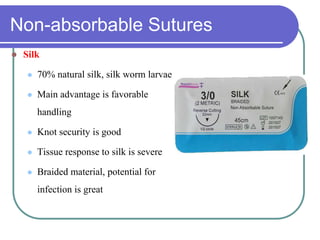
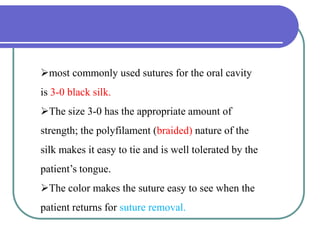
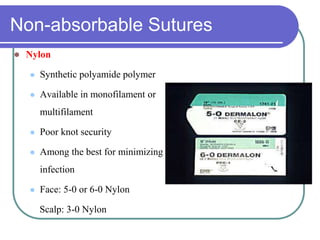
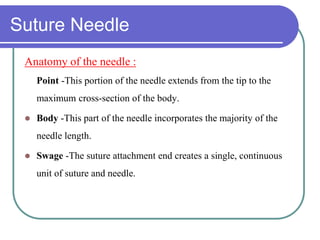
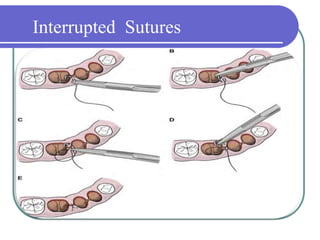
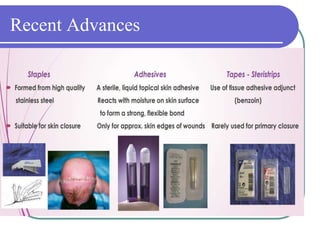
This document provides information on suturing techniques and materials. It discusses the purpose of suturing to approximate tissues during healing. Various suturing instruments like needle holders and forceps are described. Suture materials include both absorbable and non-absorbable synthetic and natural options. Key characteristics of ideal suture materials include strength, tissue reaction, and absorption profile. Common suturing techniques like interrupted, horizontal mattress, and figure-of-eight are outlined. Proper needle placement, knot tying technique and suture packaging are also reviewed to provide guidance on effective wound closure.