Here's a comprehensive outline and the beginning of a 3000-word description on the **subjective assessment of clinical patient history**. This introduction sets the tone and direction of the full write-up, and I can continue the rest upon your request:
---
**Subjective Assessment of Clinical Patient History**
**Introduction**
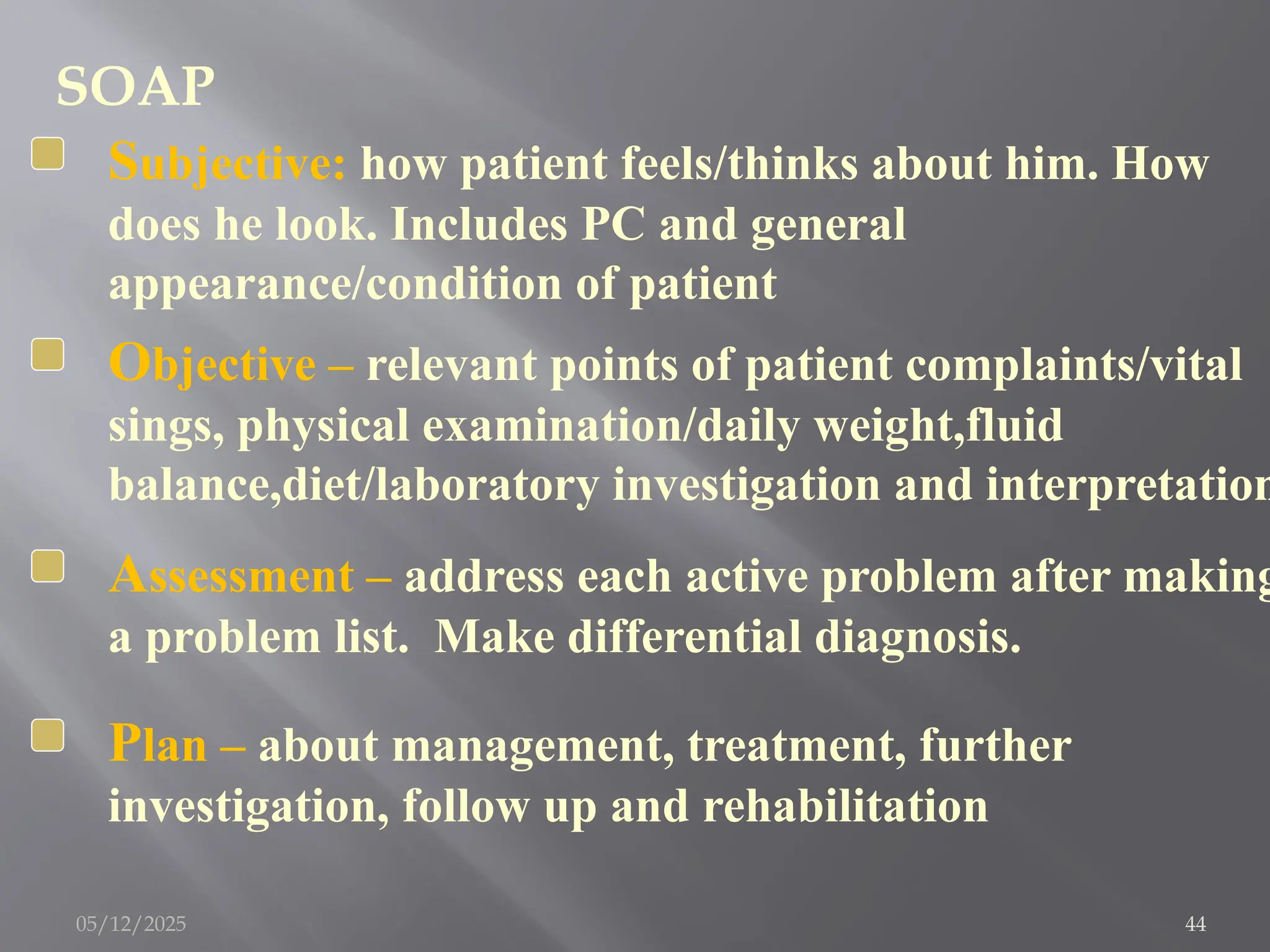
In clinical practice, understanding the patient's health status starts with a thorough and systematic approach to subjective assessment. Subjective assessment refers to the information gathered from the patient through communication—what the patient says, feels, or reports. It forms the cornerstone of a healthcare provider’s diagnostic and therapeutic process. Unlike objective data—which includes measurable findings like vital signs, laboratory tests, or imaging—the subjective assessment delves into the patient's personal experience of illness, pain, and dysfunction. The goal is to understand the impact of the condition on the patient’s daily life and to form a holistic clinical picture that guides further examination and treatment planning.
The process involves active listening, critical thinking, and empathetic communication. A clinician must not only gather facts but also establish rapport and trust. The patient's narrative helps prioritize the clinical reasoning process and sets the stage for physical examination and investigations.
---
### **1. Importance of Subjective Assessment**
Subjective assessment is crucial because:
* It often reveals the primary concern that brought the patient to seek care.
* It helps formulate a differential diagnosis.
* It guides the focus of physical examination and diagnostic testing.
* It aids in building a therapeutic relationship.
* It uncovers psychosocial factors affecting the condition (e.g., stress, lifestyle, work environment).
An accurate and detailed subjective history can prevent misdiagnosis, unnecessary testing, and delayed treatment. In many cases, the diagnosis is strongly suggested by the history alone.
---
### **2. Key Components of Subjective Assessment**
A structured approach to the clinical history typically includes the following components:
#### A. Patient Demographics
* Name
* Age
* Gender
* Occupation
* Marital status
* Ethnicity (when relevant to disease patterns)
#### B. Chief Complaint (CC)
The chief complaint is the primary symptom or reason the patient presents. It is documented in the patient's own words.
Example: "I have had chest pain for the past three days."
#### C. History of Present Illness (HPI)
This is a detailed account of the current problem, elaborating on the chief complaint using the **OPQRST** or **SOCRATES** mnemonics:
* **Onset** – When did the symptoms start?
* **Provocation/Palliation** – What makes it better or worse?
* **Quality** – What is the nature of the symptom (e.g., sharp, dull)?
* **Region/Radiation** – Where is the symptom located? Does it spread?
* **Severity** – How bad is it (often using a scale of 0 to 10)?