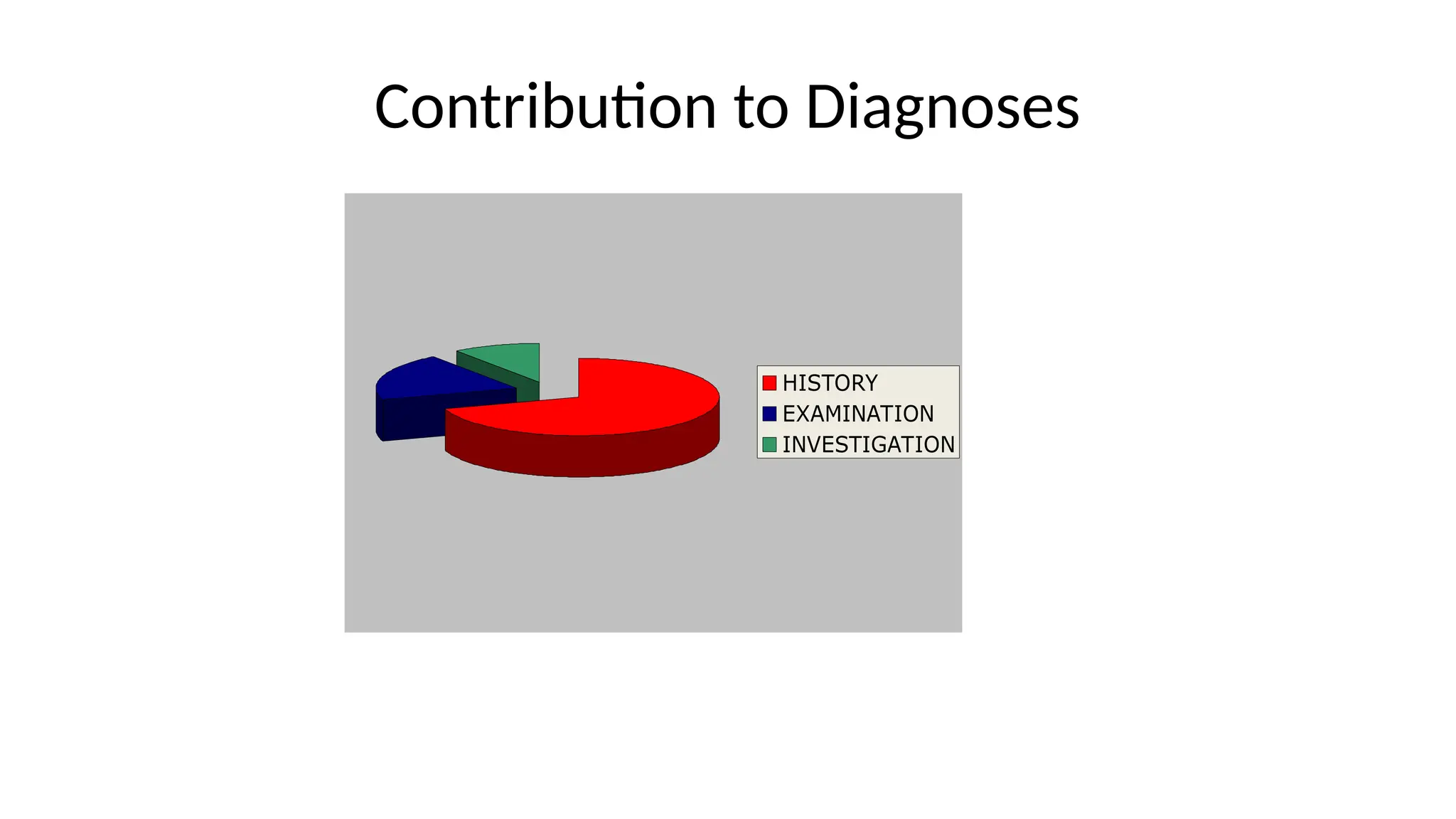
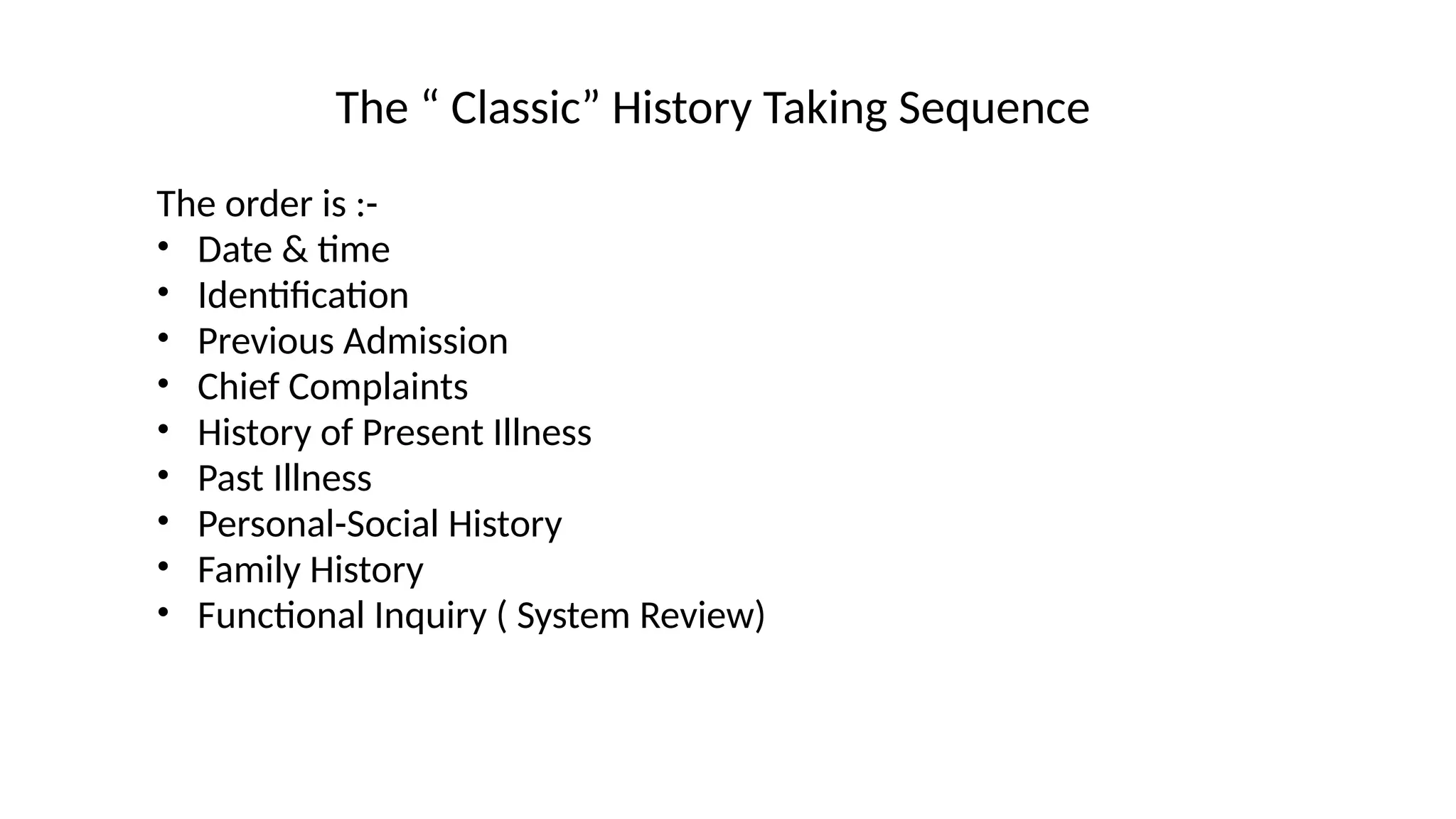
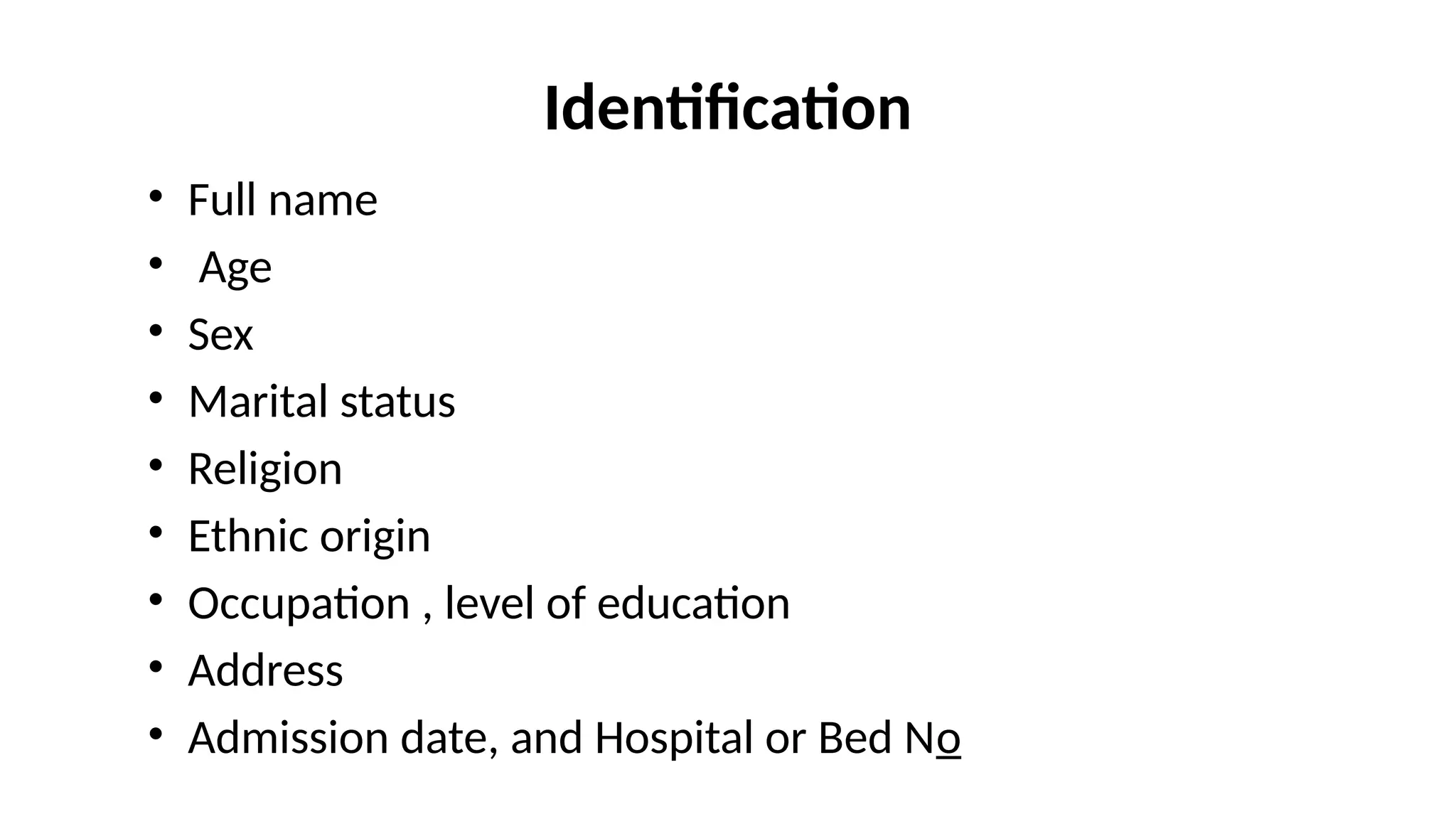
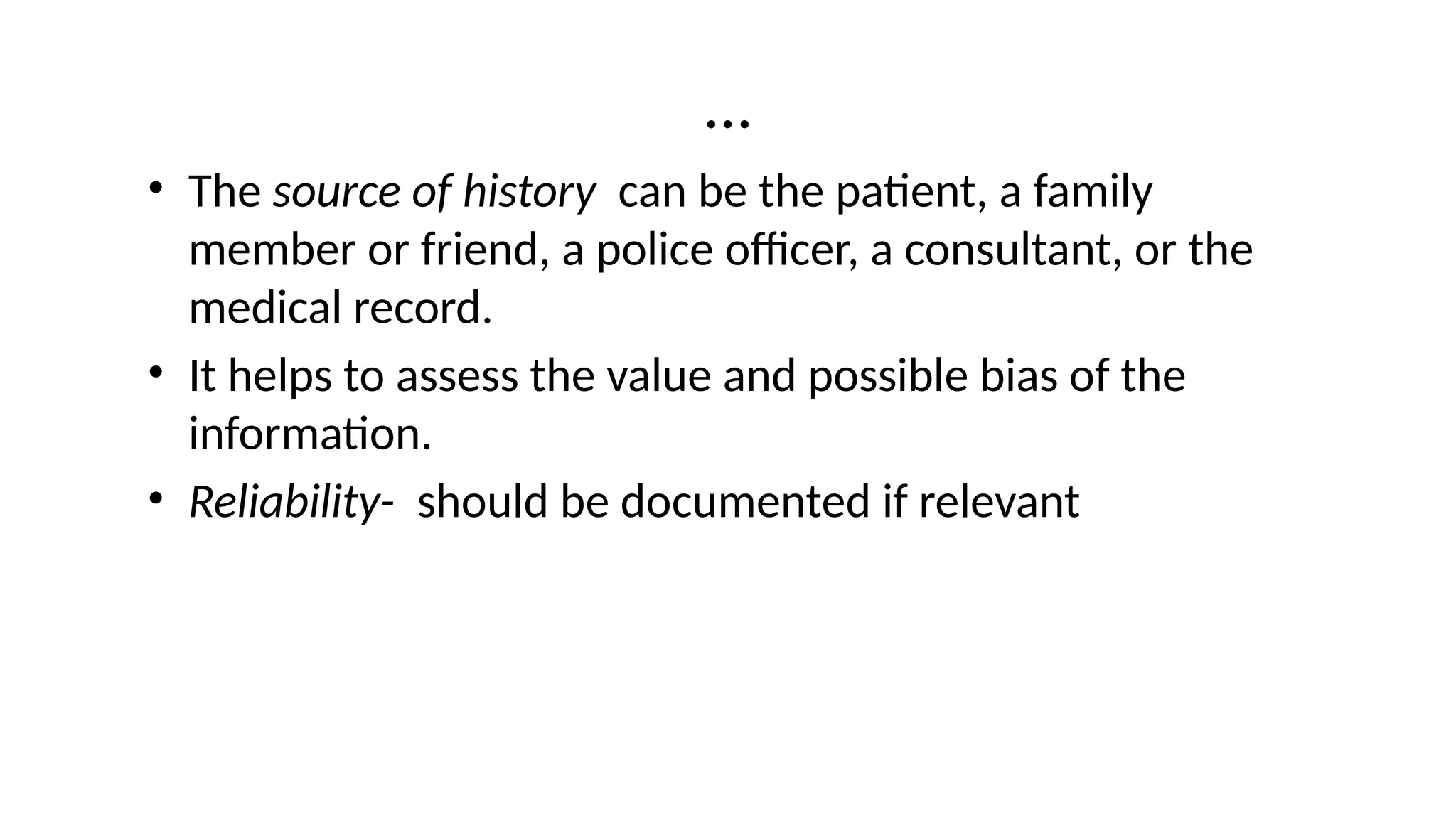
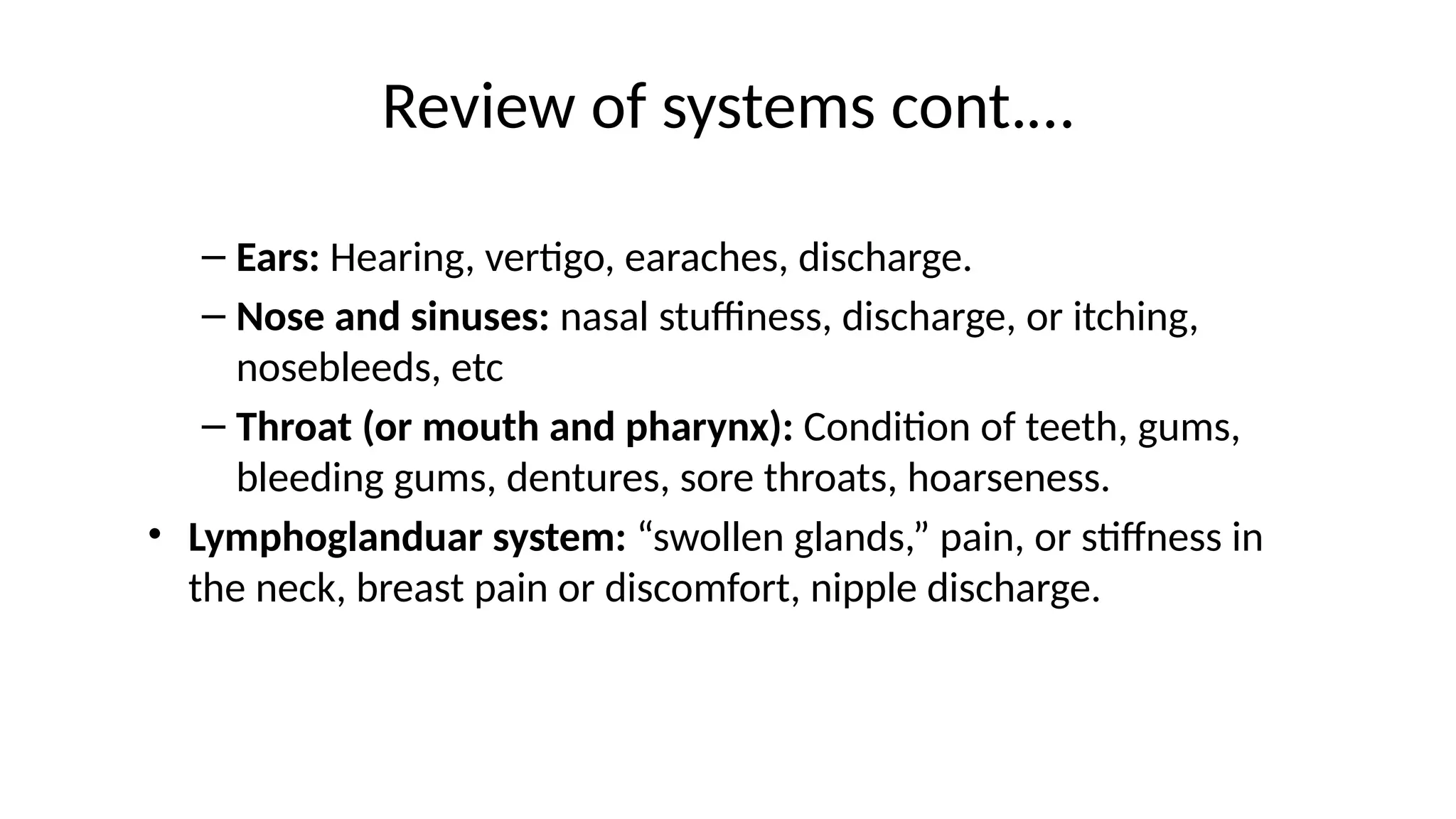
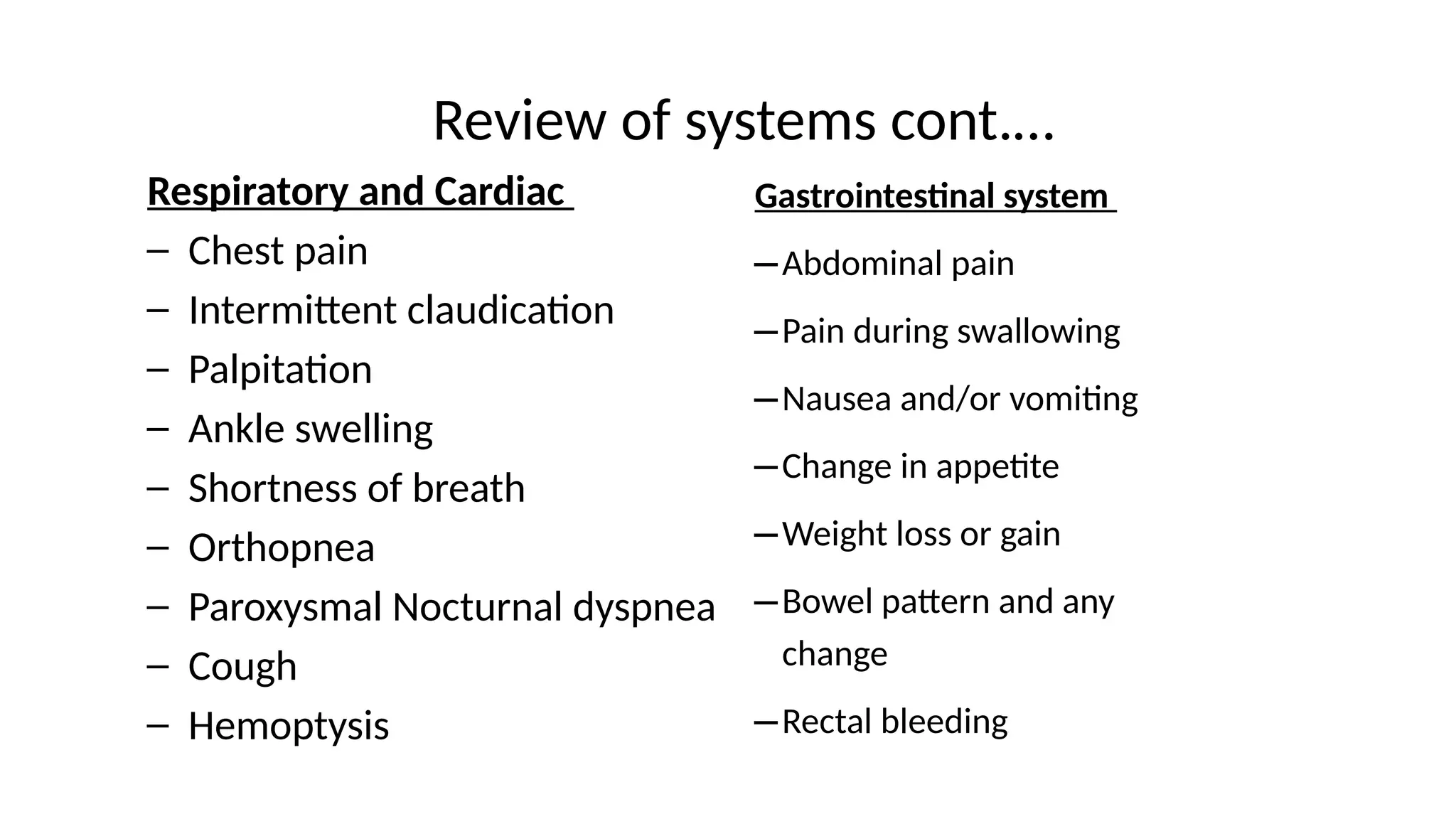
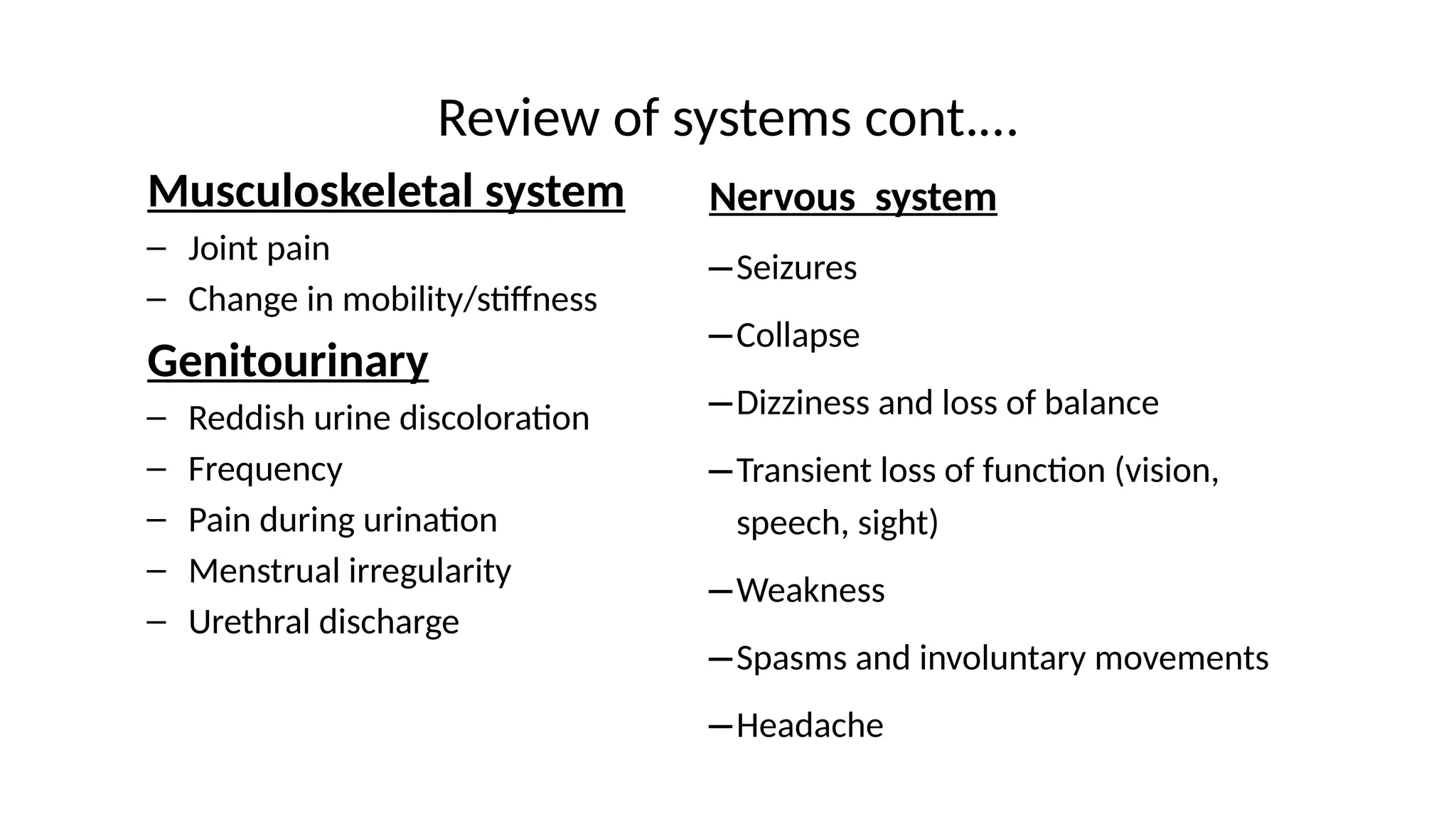
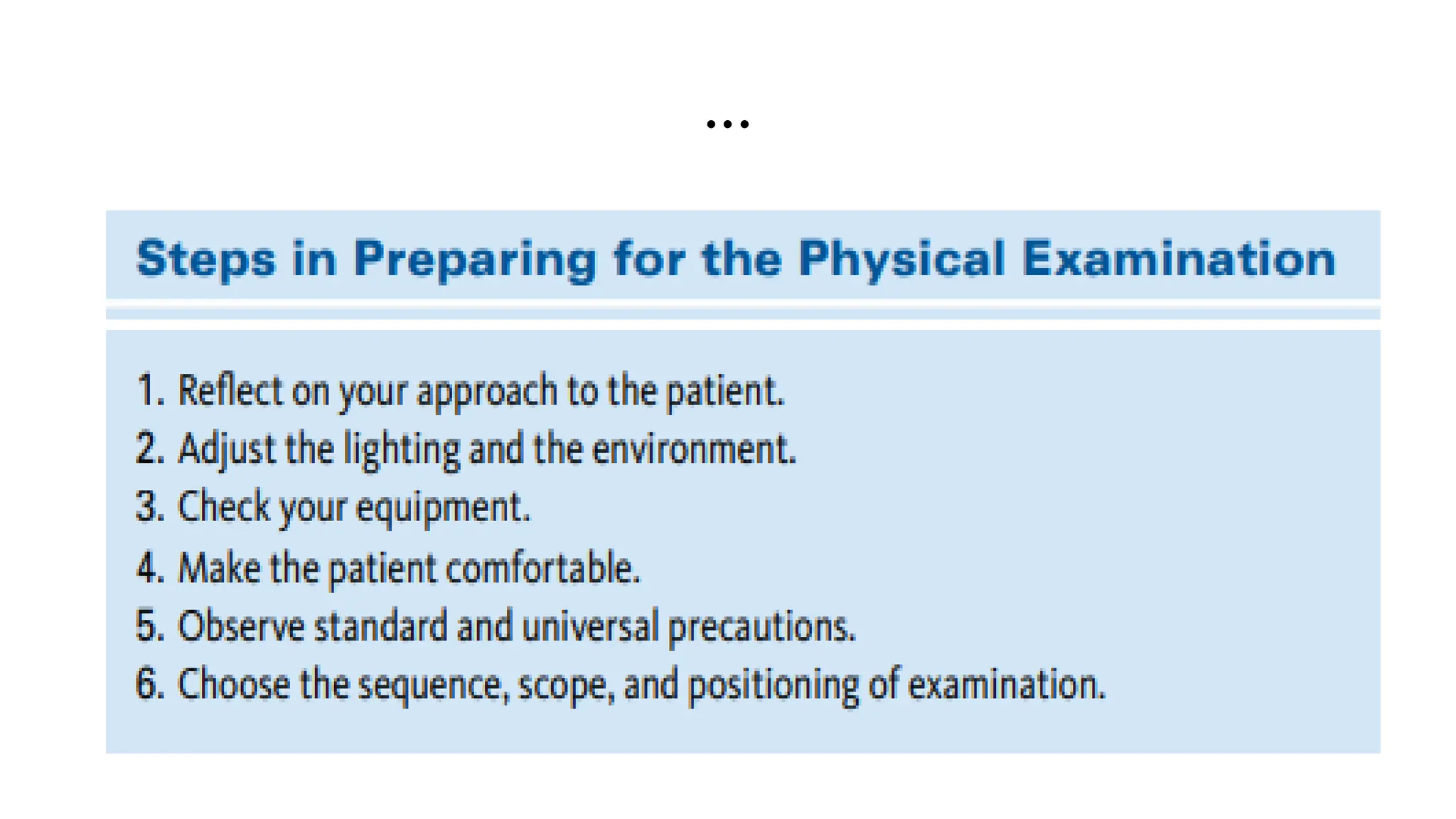
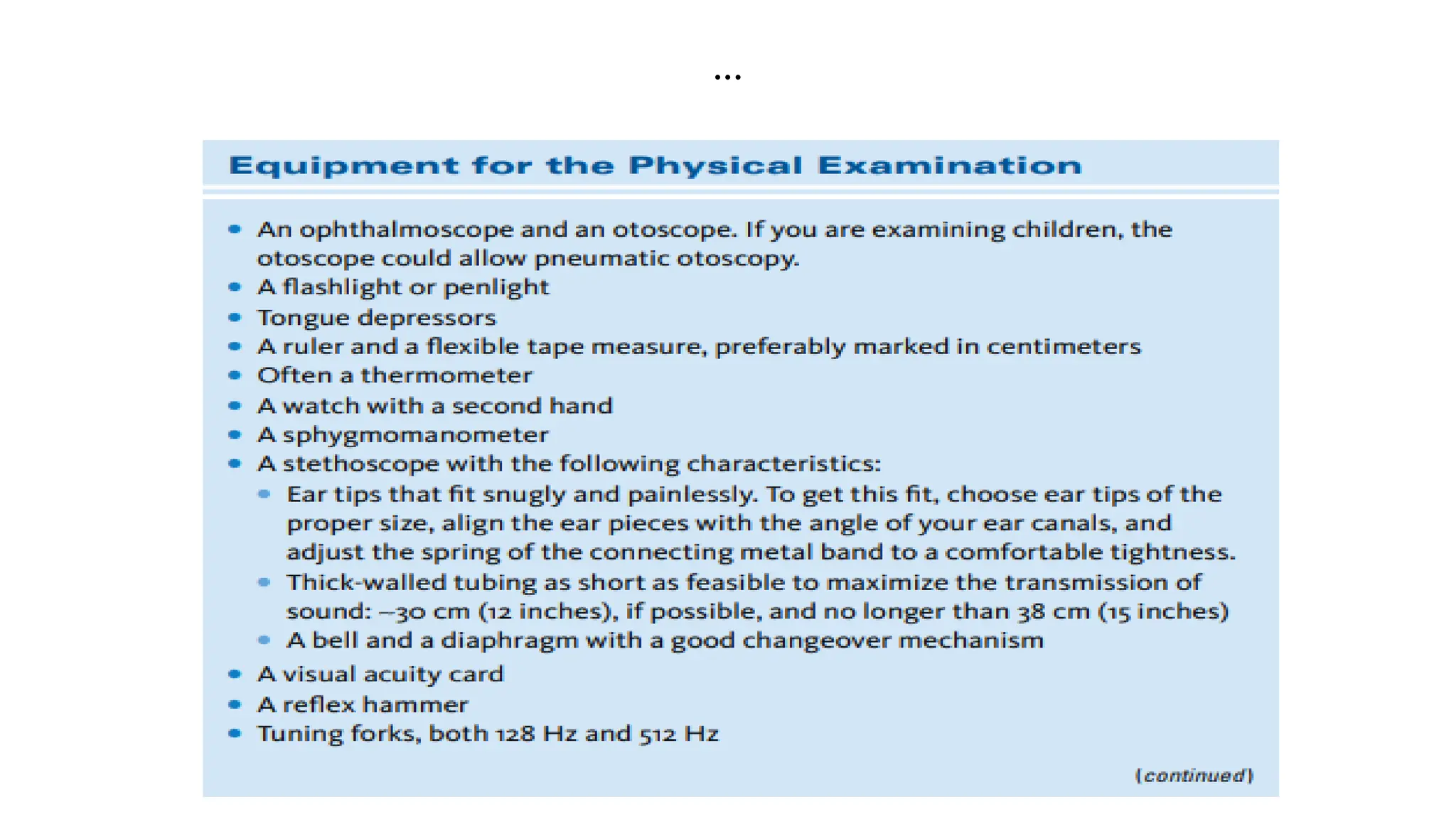
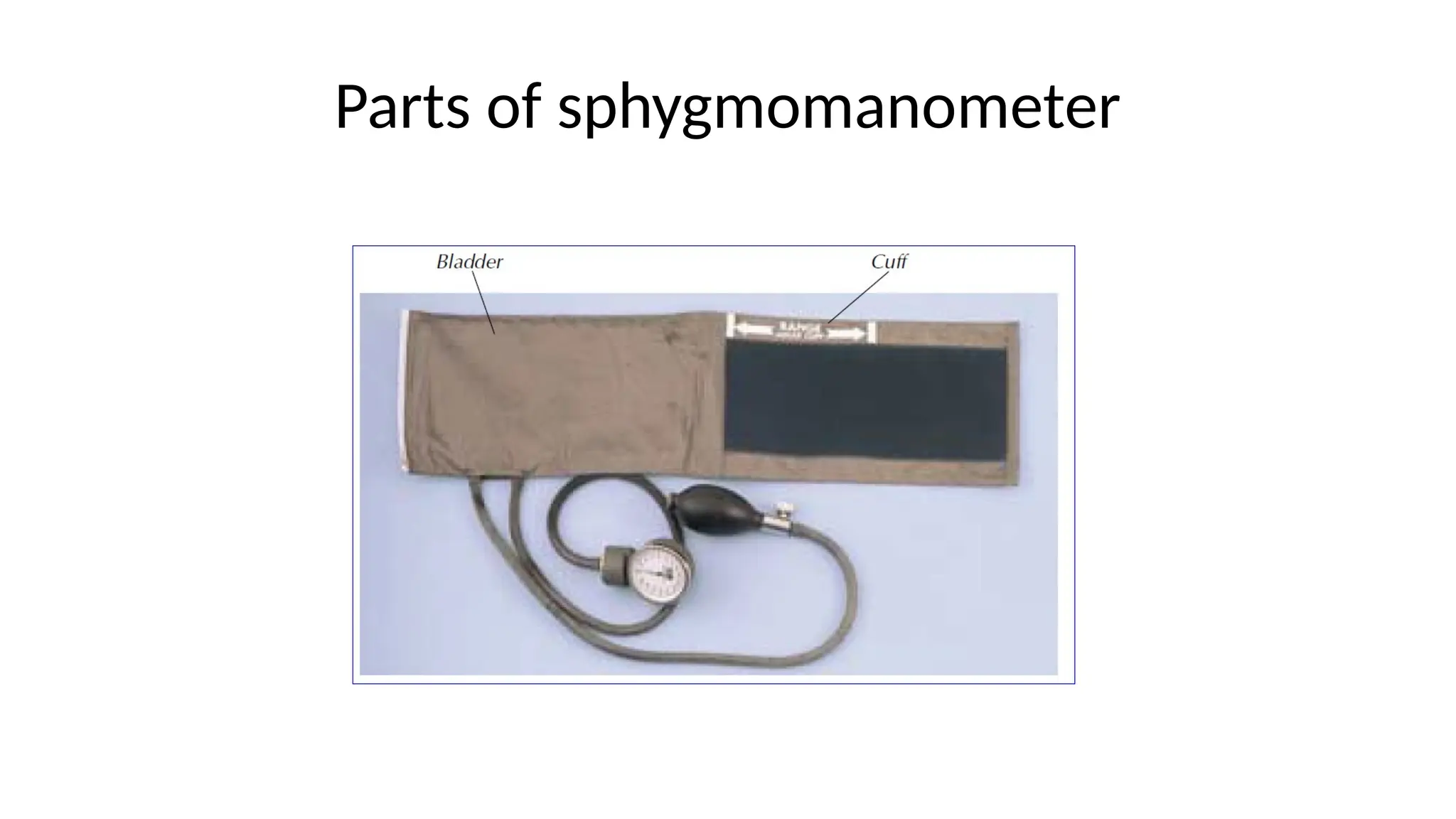
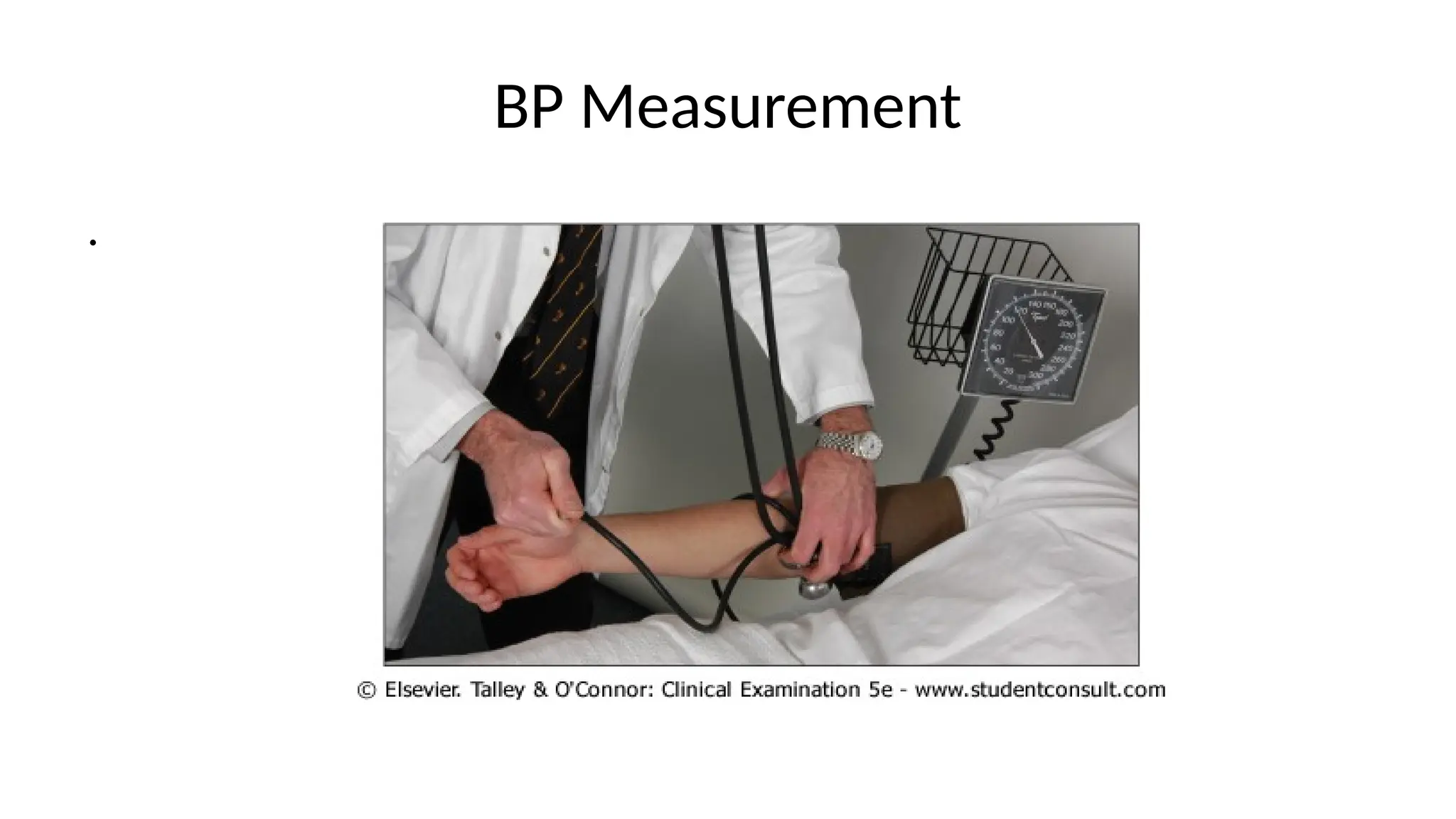
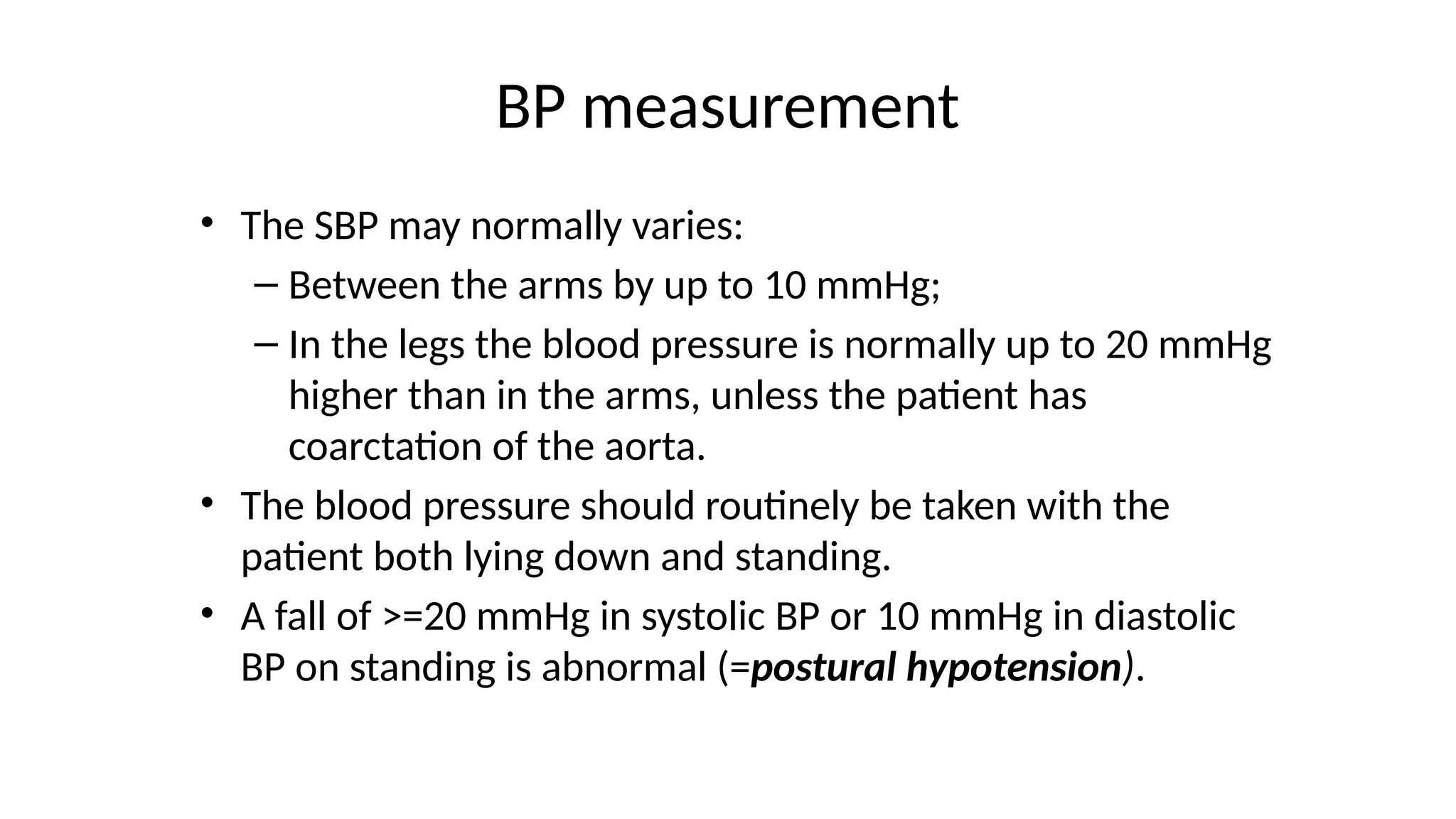
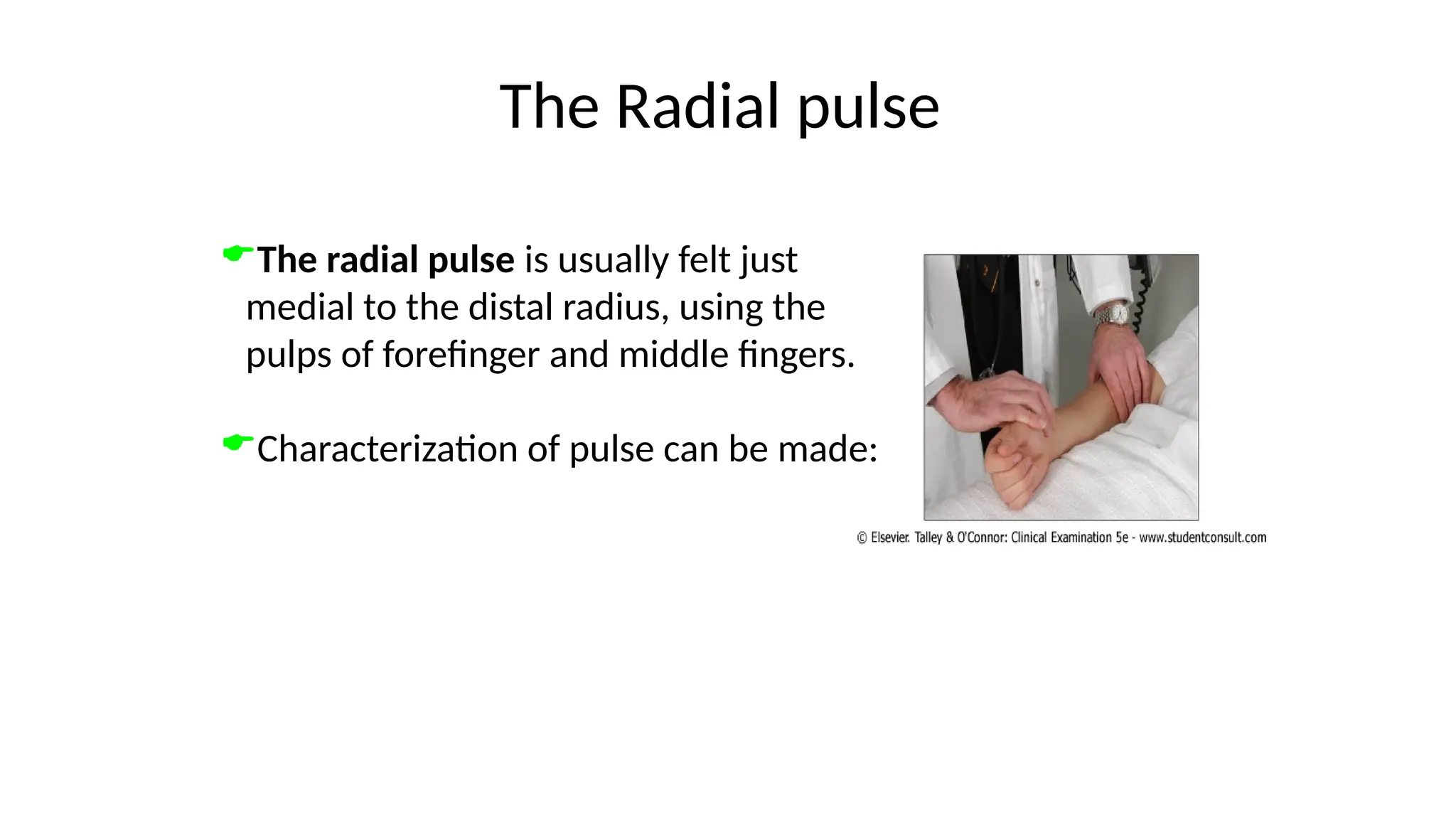
This document is a comprehensive guide on history taking and physical examination for public health students, outlining the essential skills involved in clinical evaluation. It details the steps in obtaining medical history, including the sequence of questions to ask, factors in establishing rapport, and comprehensive aspects of personal and family history. Additionally, it covers the physical examination methods and vital signs assessments, emphasizing the importance of systematic techniques and attention to patient details.