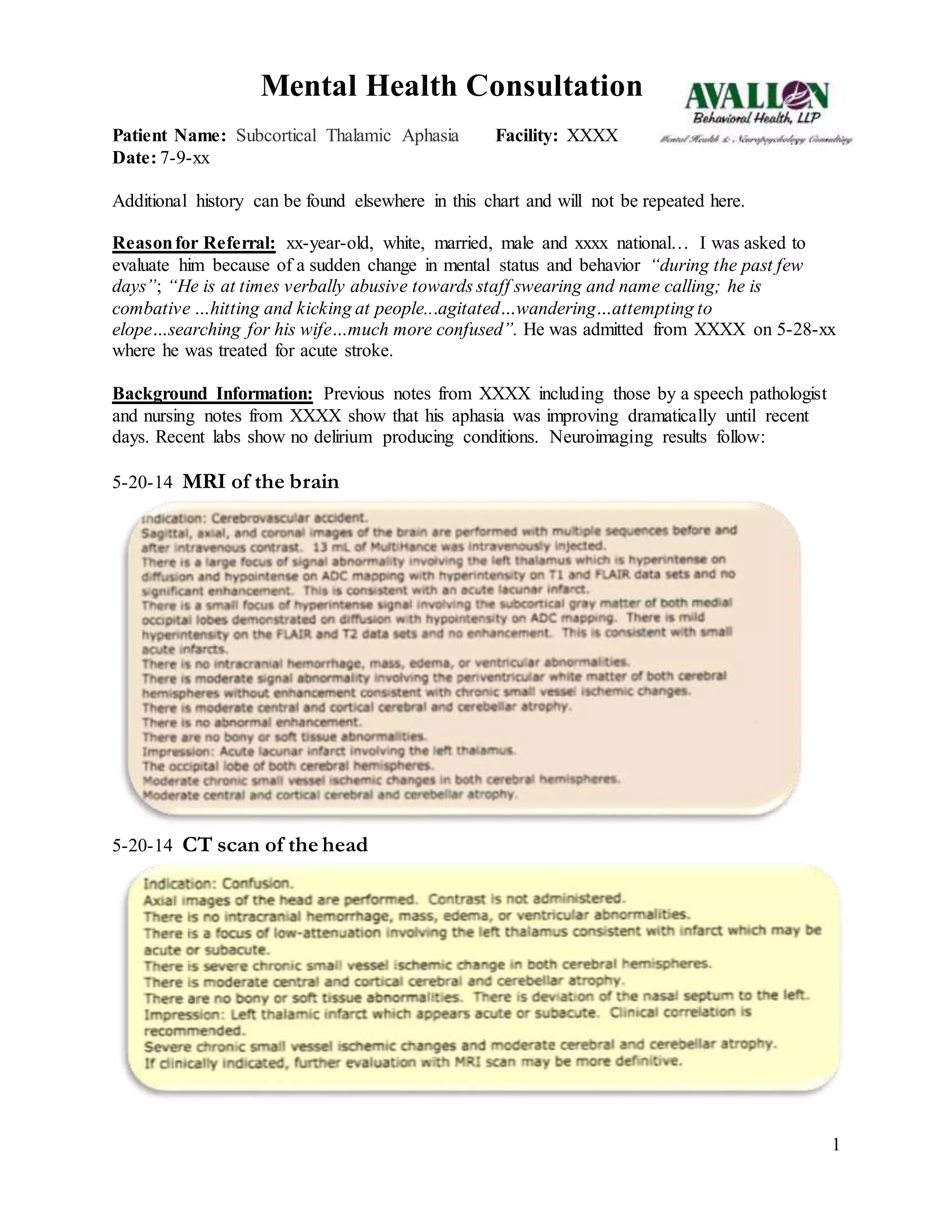
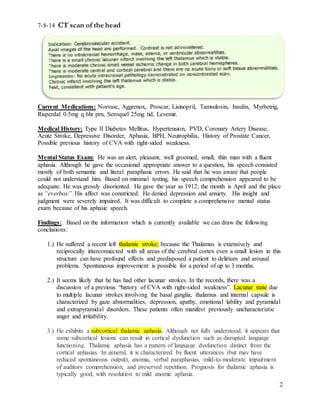
1. The patient suffered a recent left thalamic stroke and likely previous smaller strokes, leaving him vulnerable to delirium. He exhibits subcortical thalamic aphasia characterized by fluent but paraphasic speech with good repetition and mild comprehension deficits.
2. The patient's recent problematic behaviors are likely due to emotional and behavioral disinhibition from his strokes. Recommendations include trying Depakote to address this and involving speech therapy as thalamic aphasia often improves.
3. The patient seems acutely confused but not overtly delirious. His confusion may cause him to feel threatened and lash out. Recommendations to make him feel safe and secure include soothing his environment and having