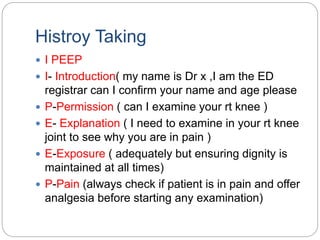
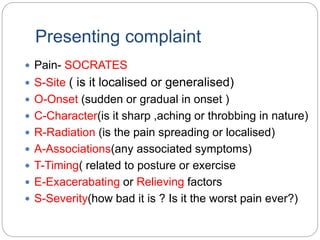
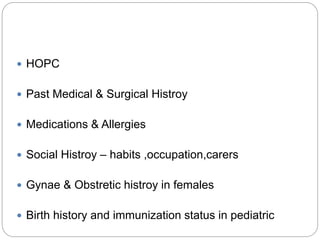
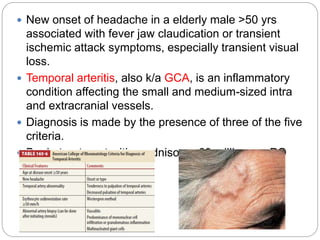
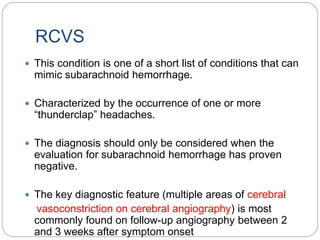
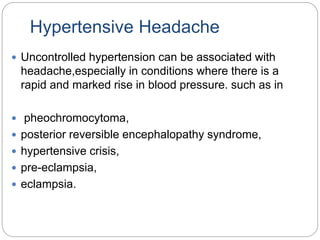
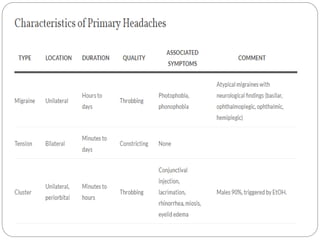
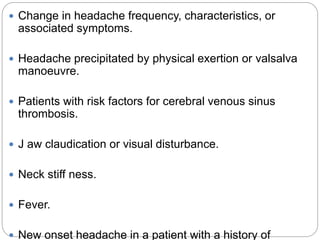
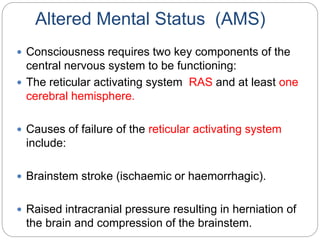
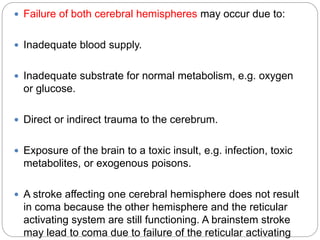
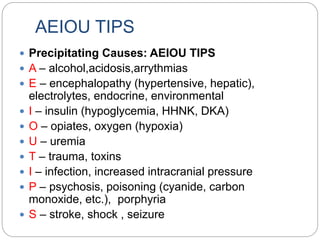
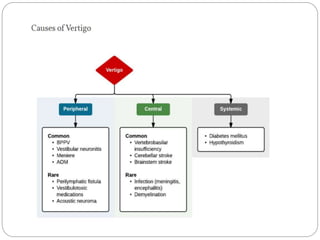
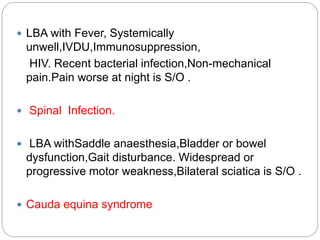
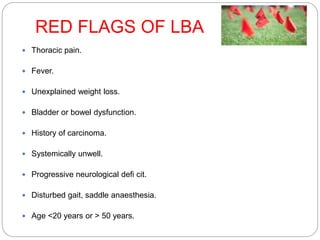
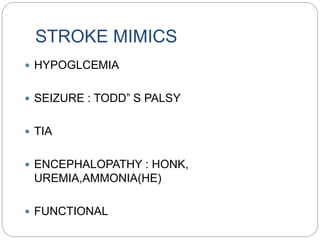
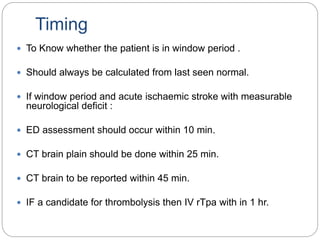
The document outlines a comprehensive approach to emergency neurology assessment, including history taking, differential diagnoses, and management strategies for conditions such as headaches, seizures, and altered mental status. It emphasizes the importance of recognizing red flags in headaches and other neurological symptoms, with guidelines for urgent treatments and imaging when necessary. Additionally, it provides a framework for the evaluation of dizziness, low back pain, and stroke signs, highlighting the critical clinical features and management protocols.