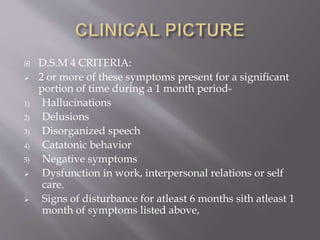
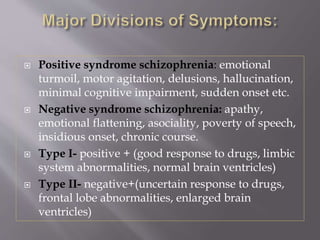
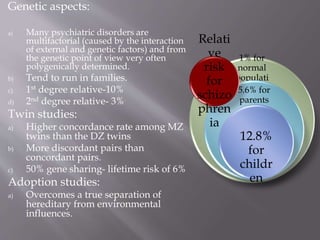
The document discusses schizophrenia from several perspectives. It covers the symptoms and types of schizophrenia based on DSM-IV criteria. It also examines the biological, genetic, neurological and environmental factors potentially involved in the development and presentation of schizophrenia. Finally, it reviews both pharmacological and psychosocial treatment approaches for schizophrenia.