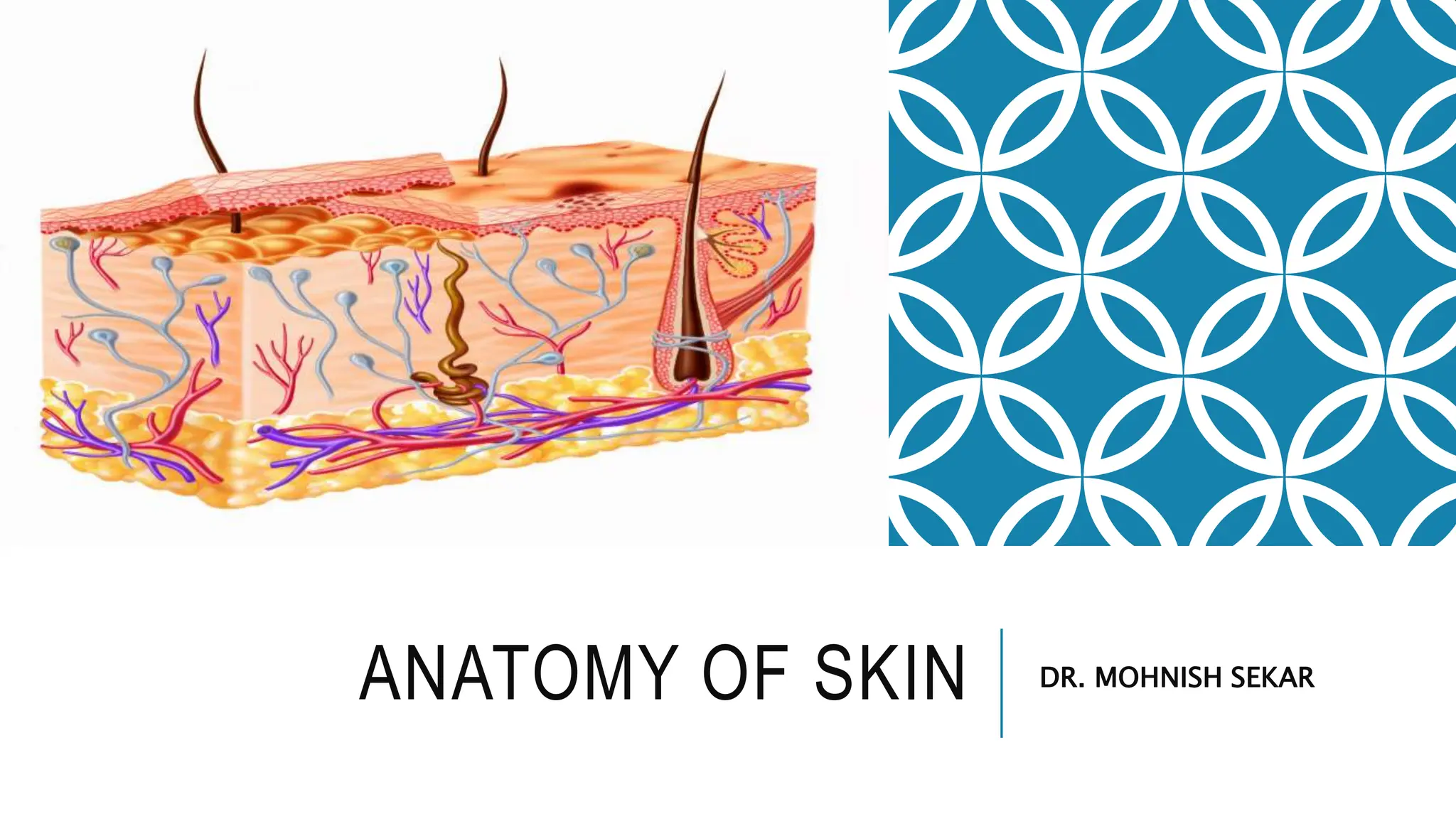
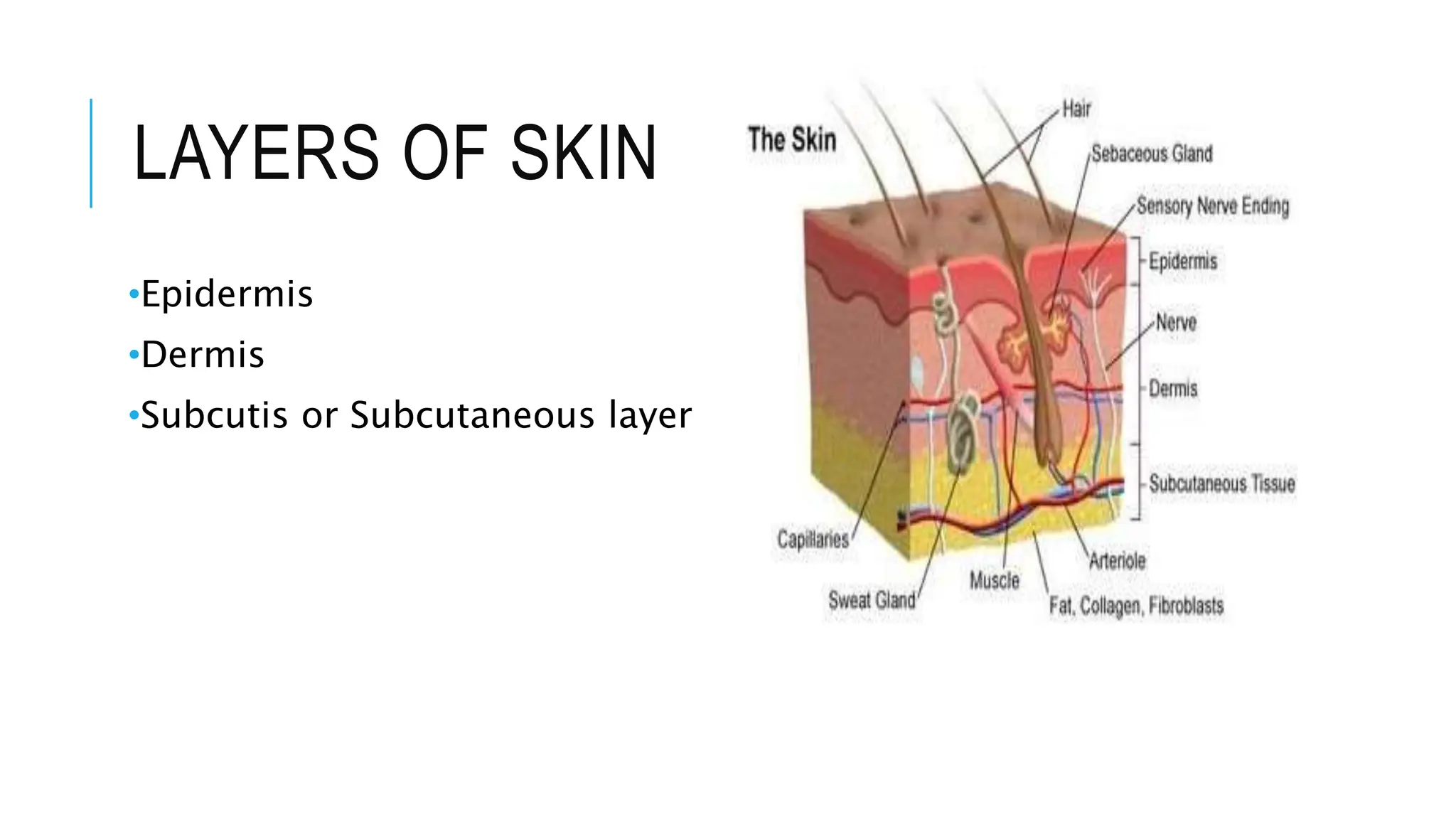
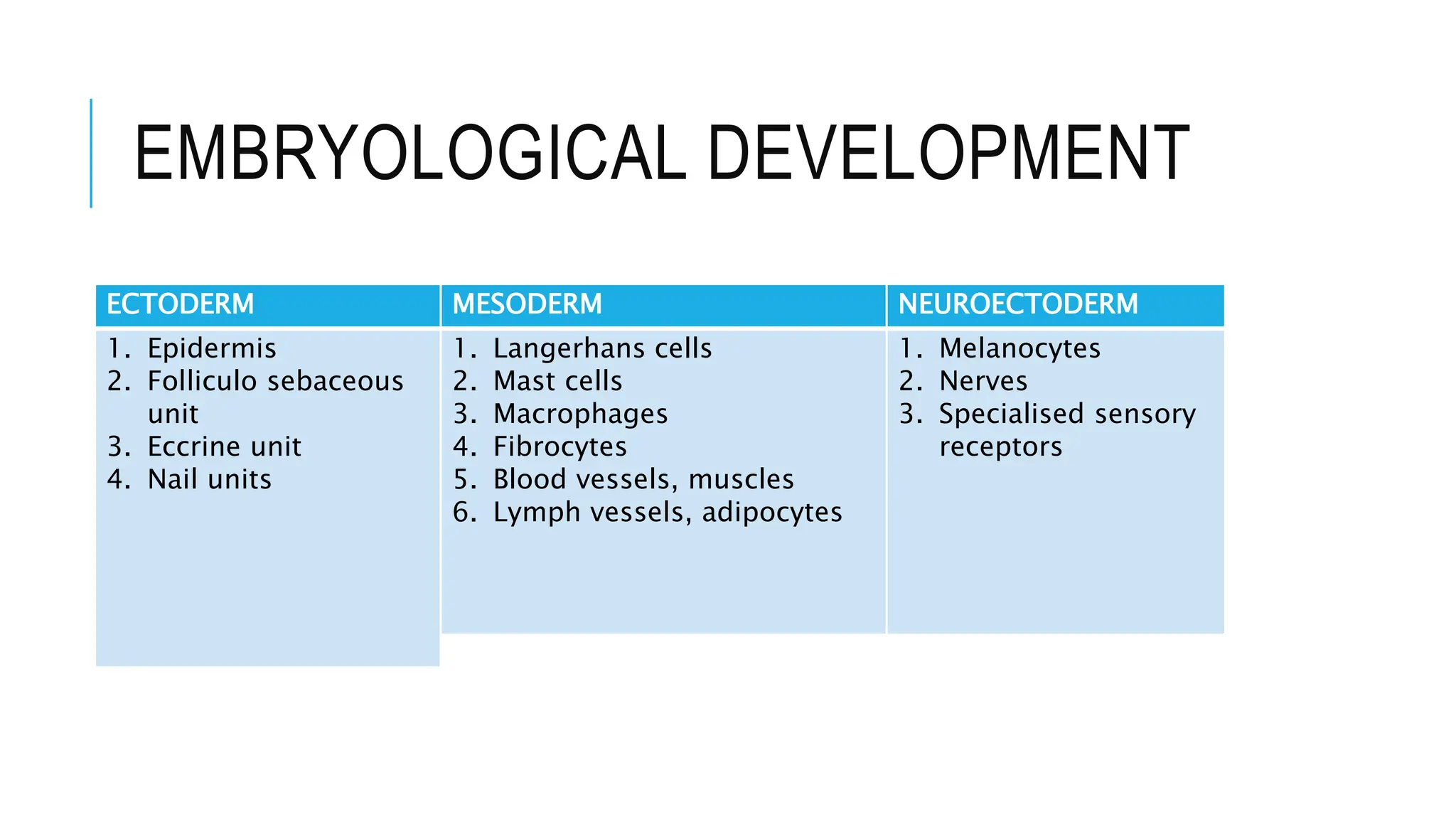
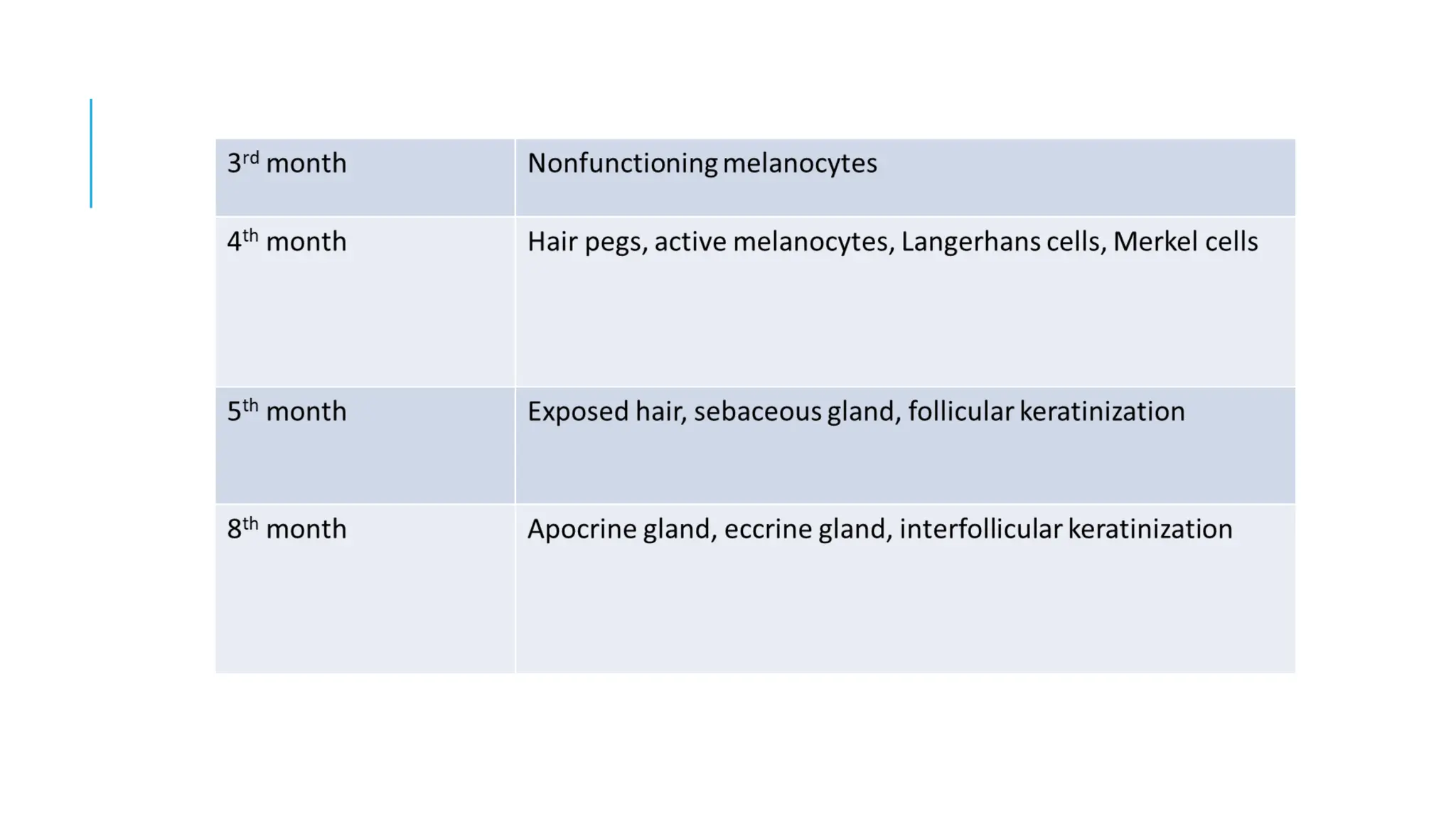
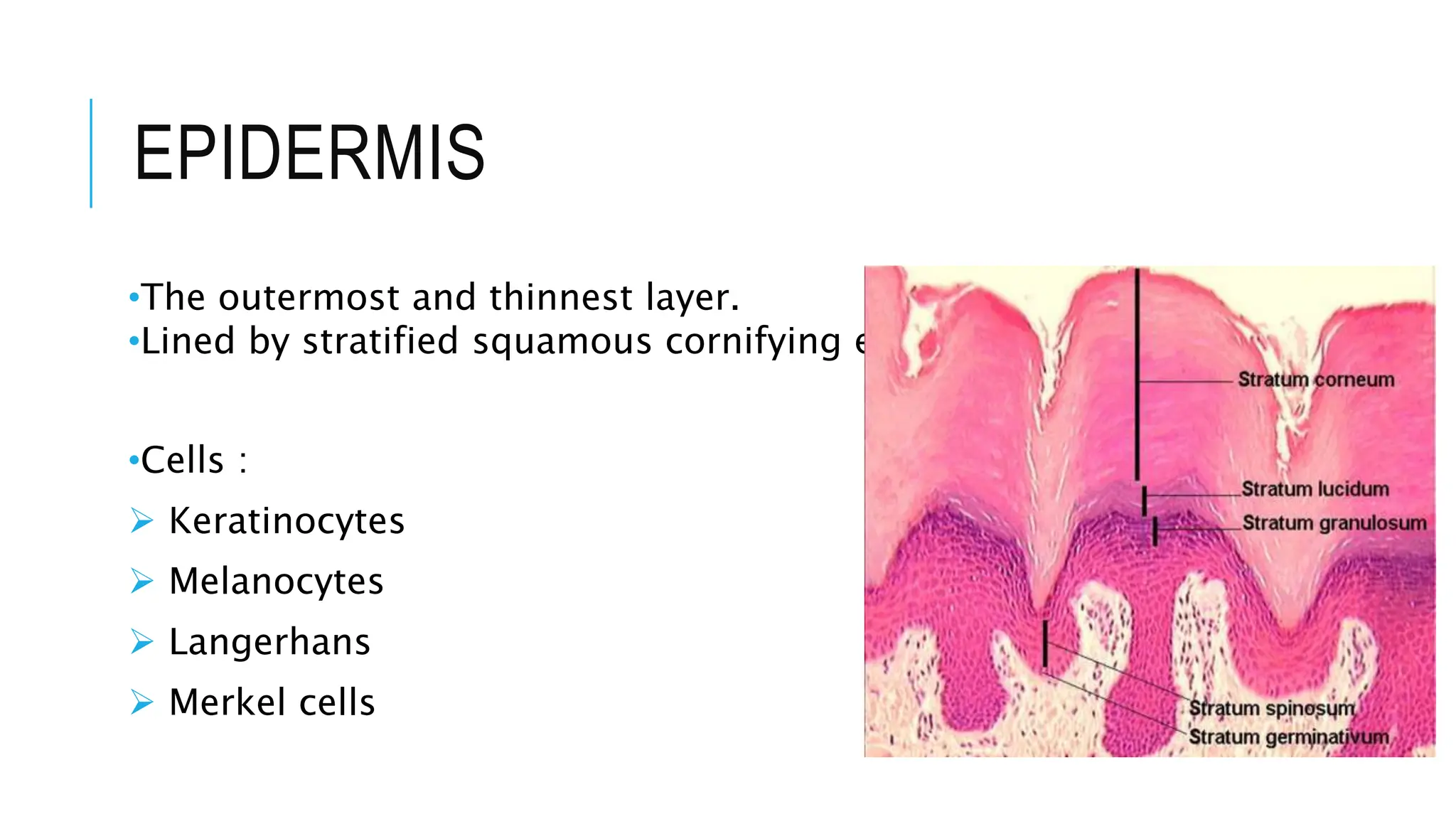
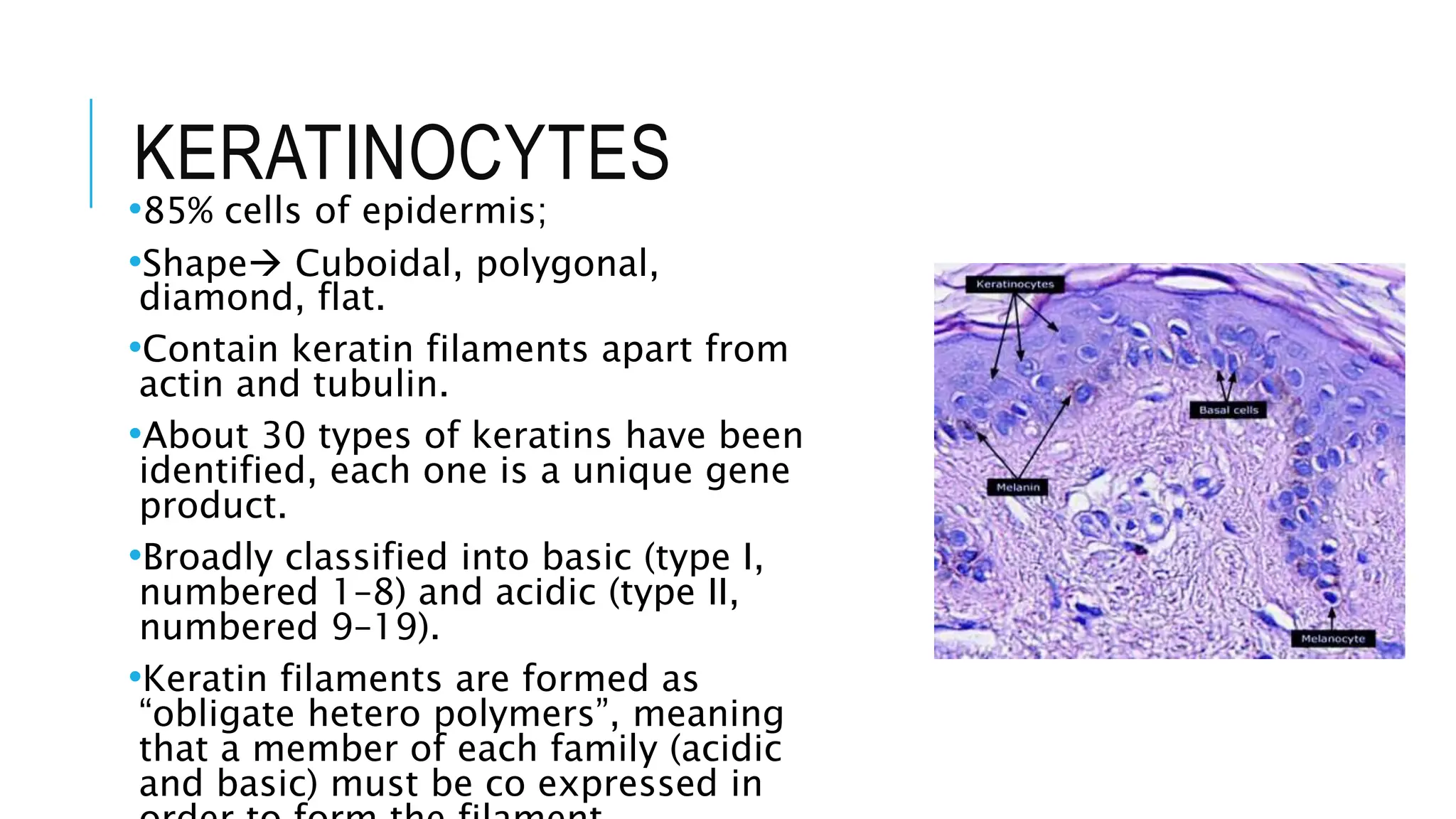
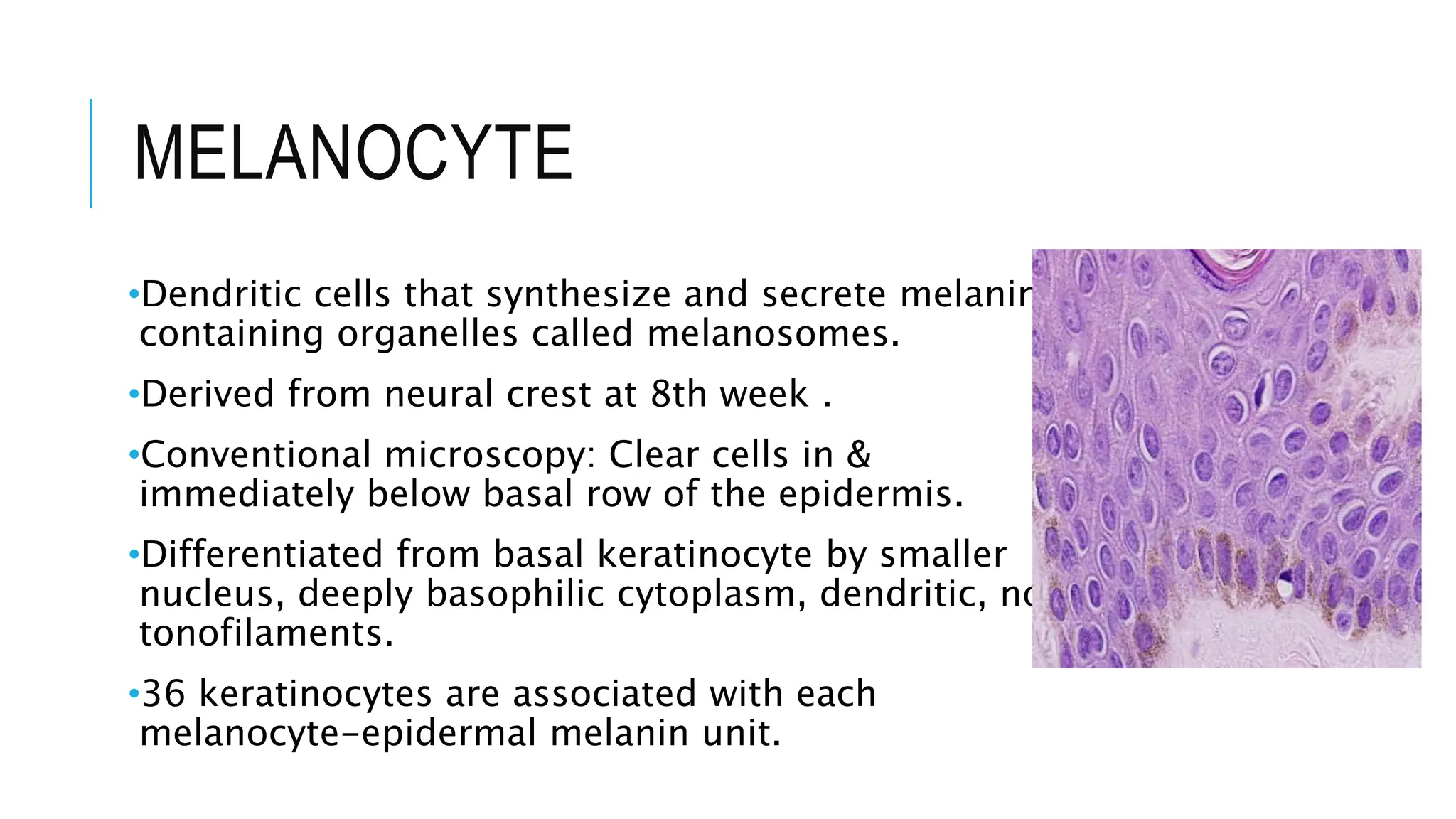
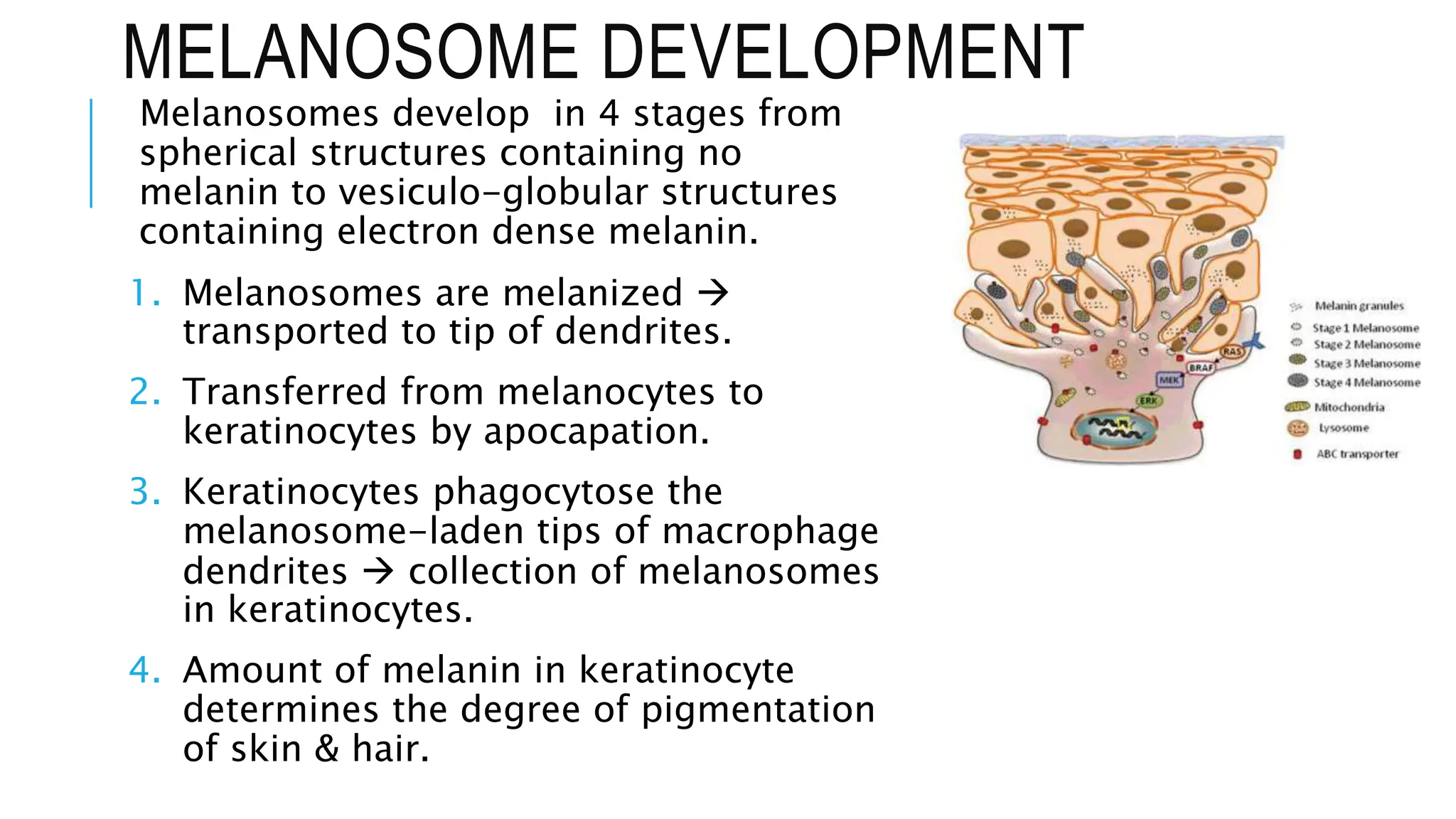
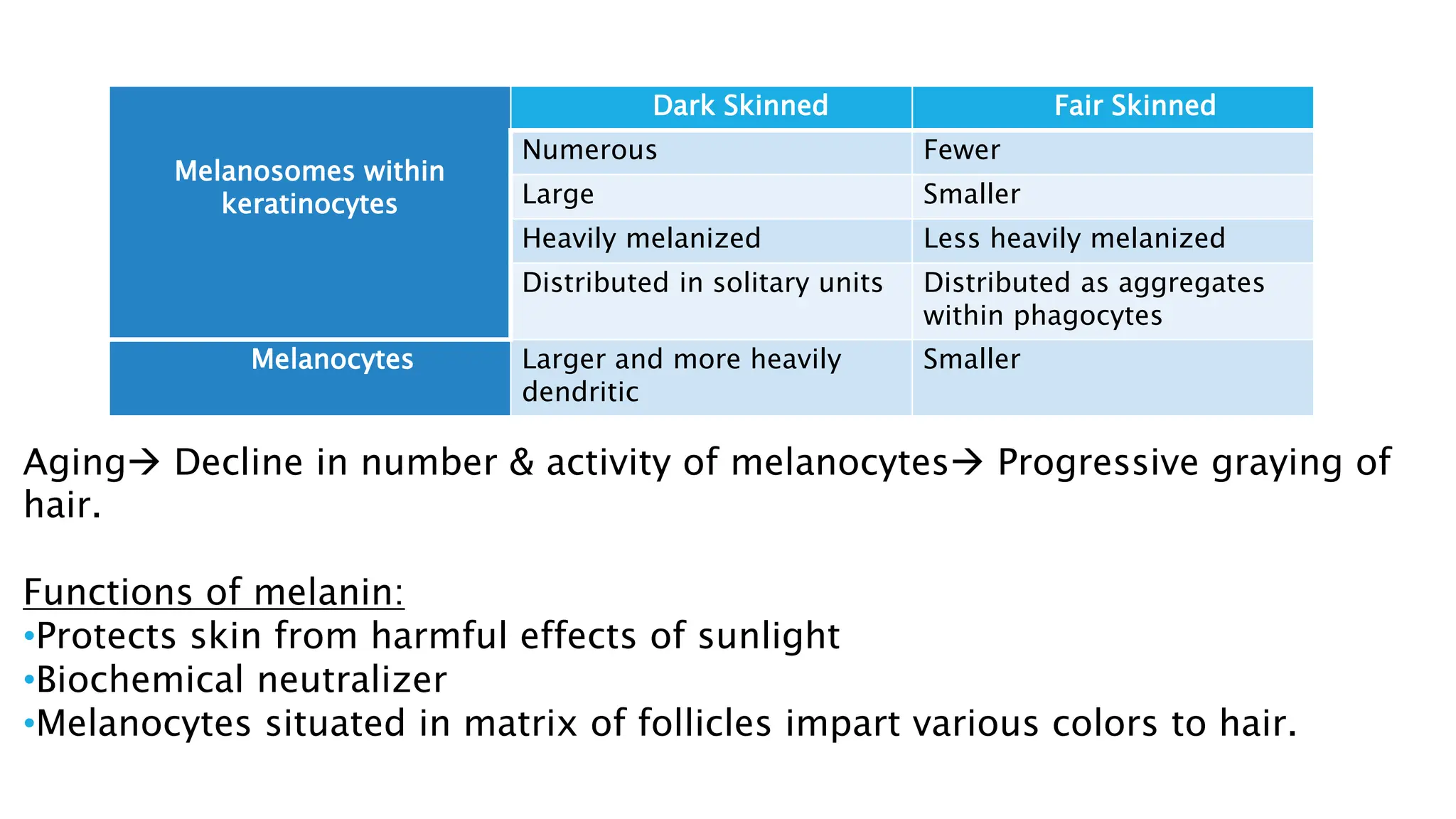
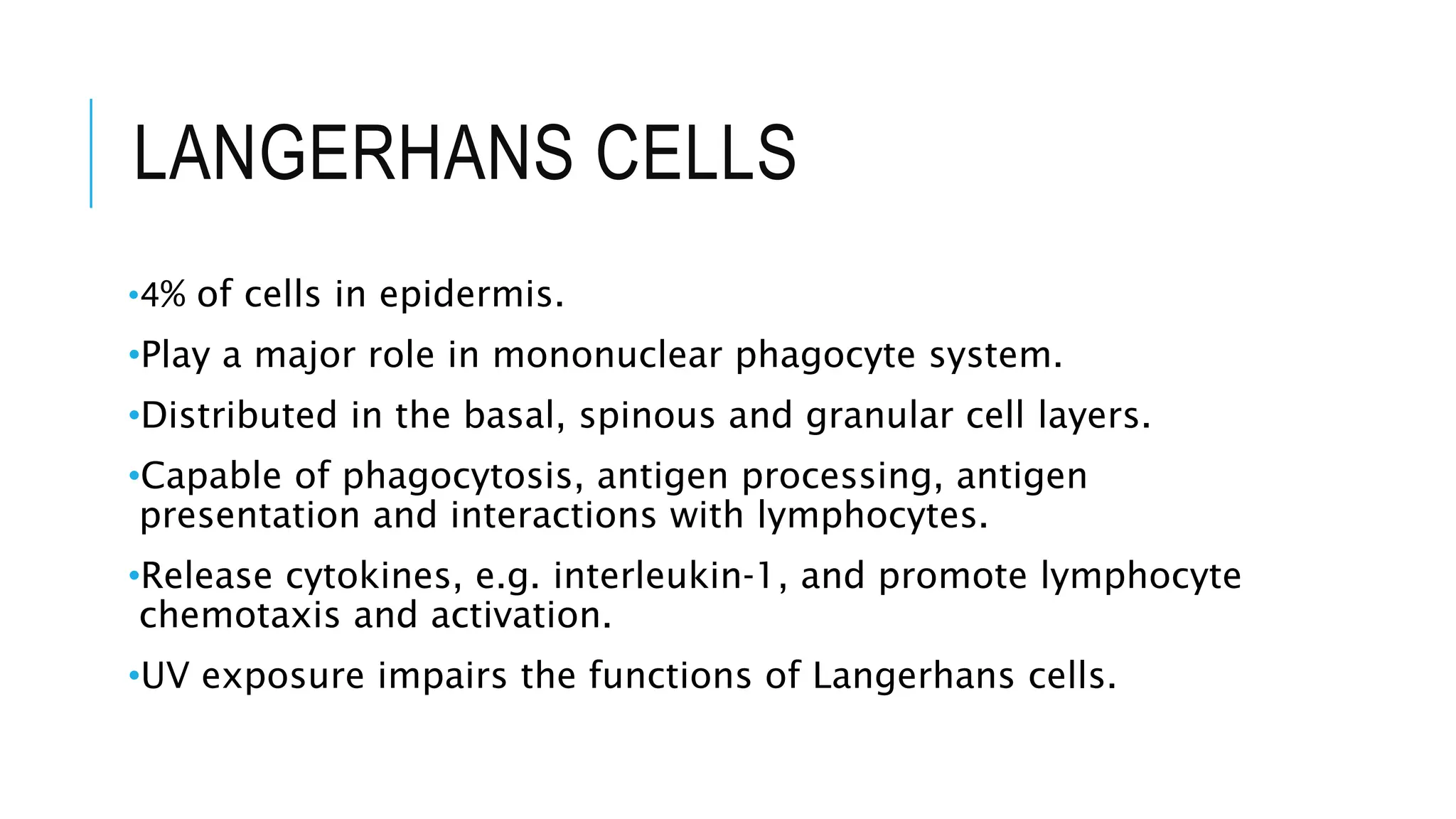
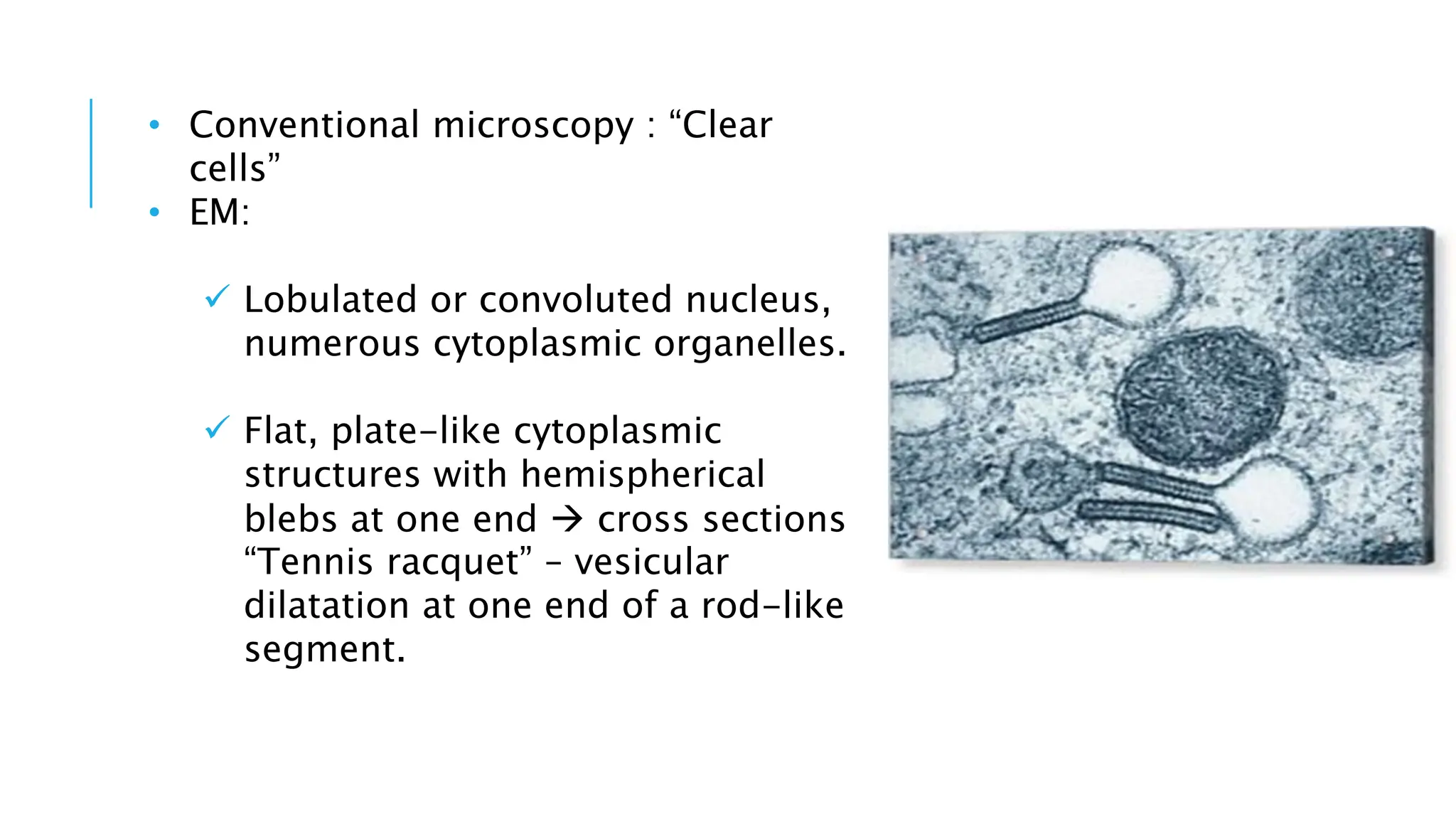
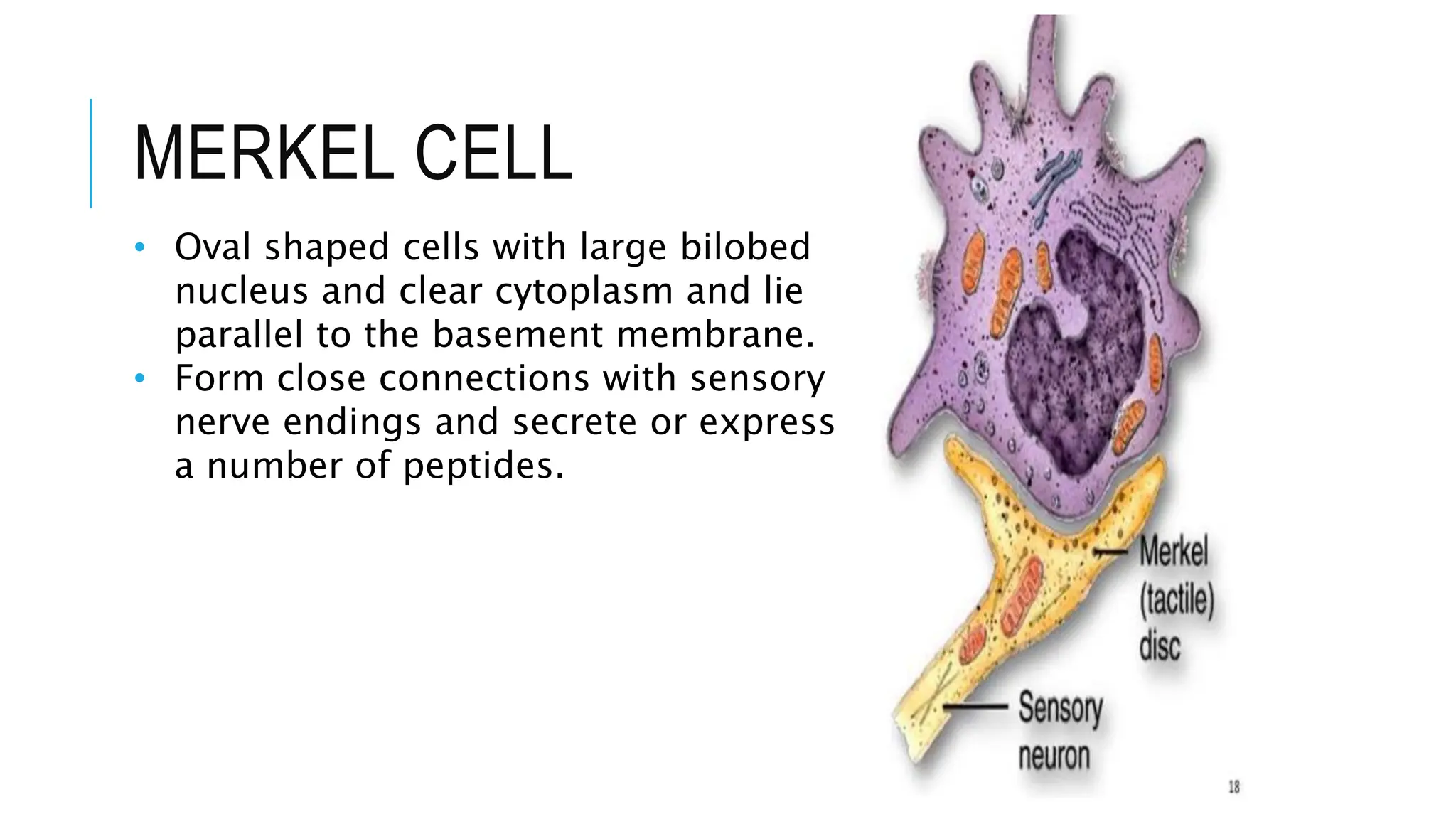
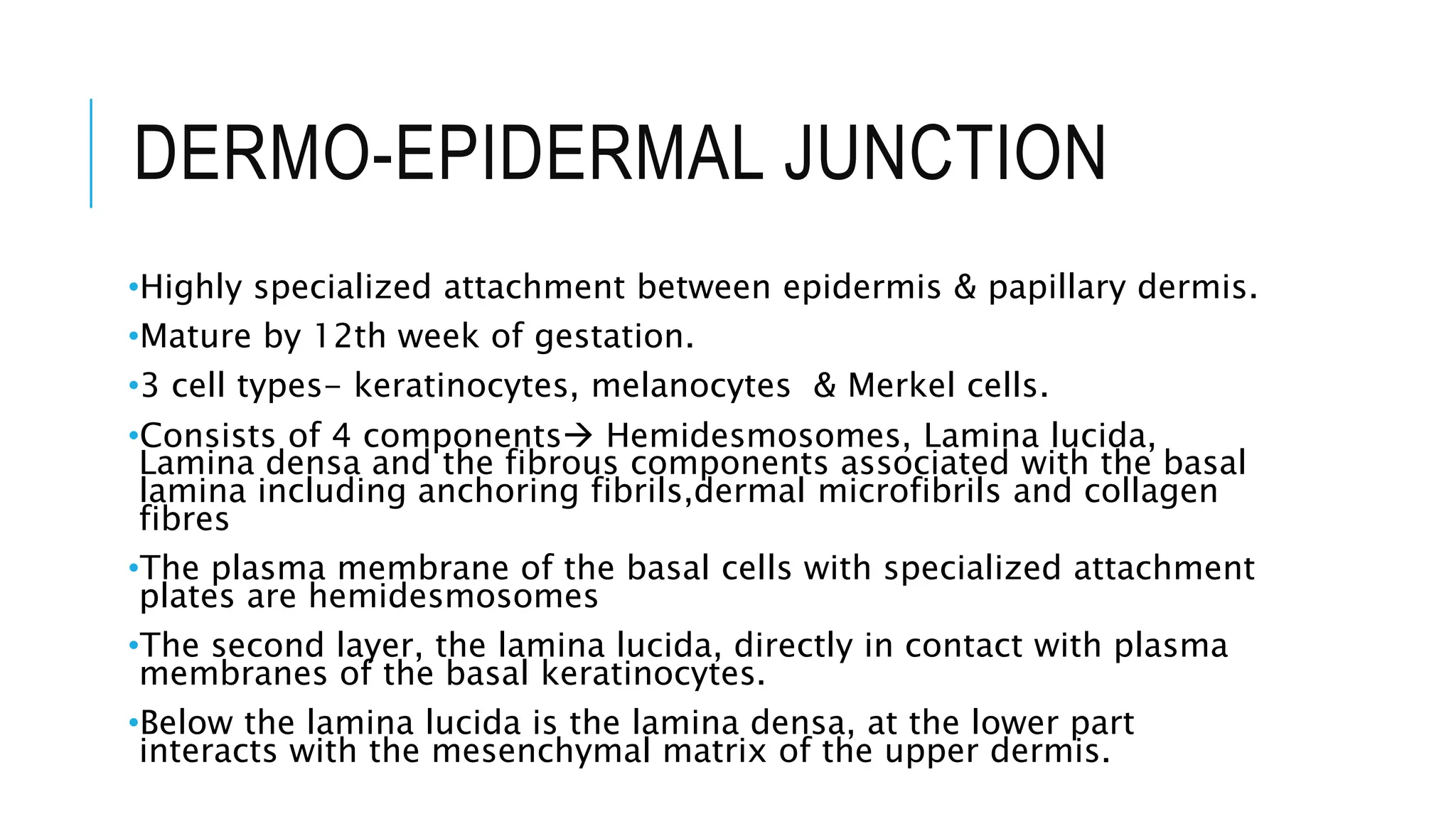
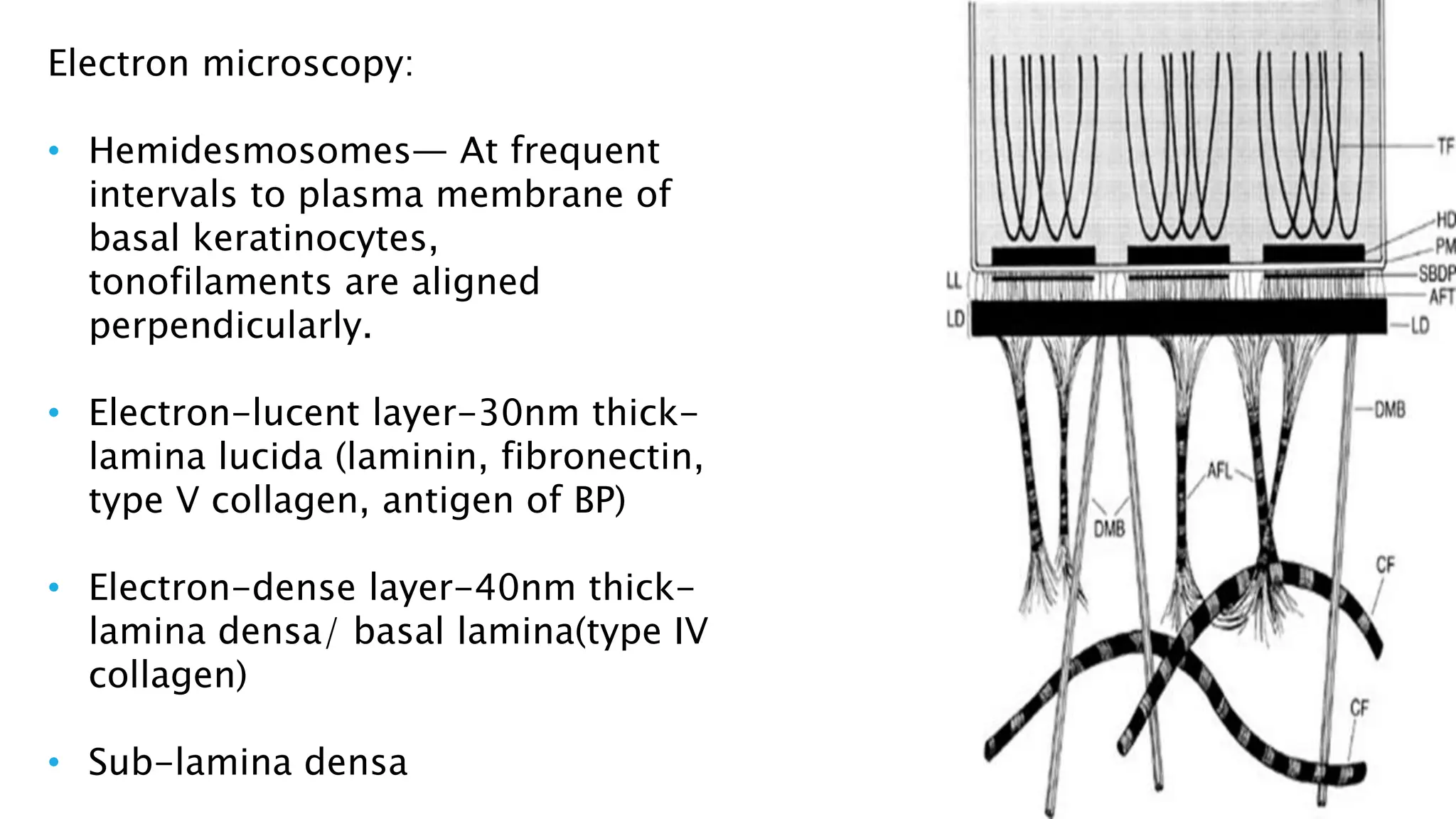
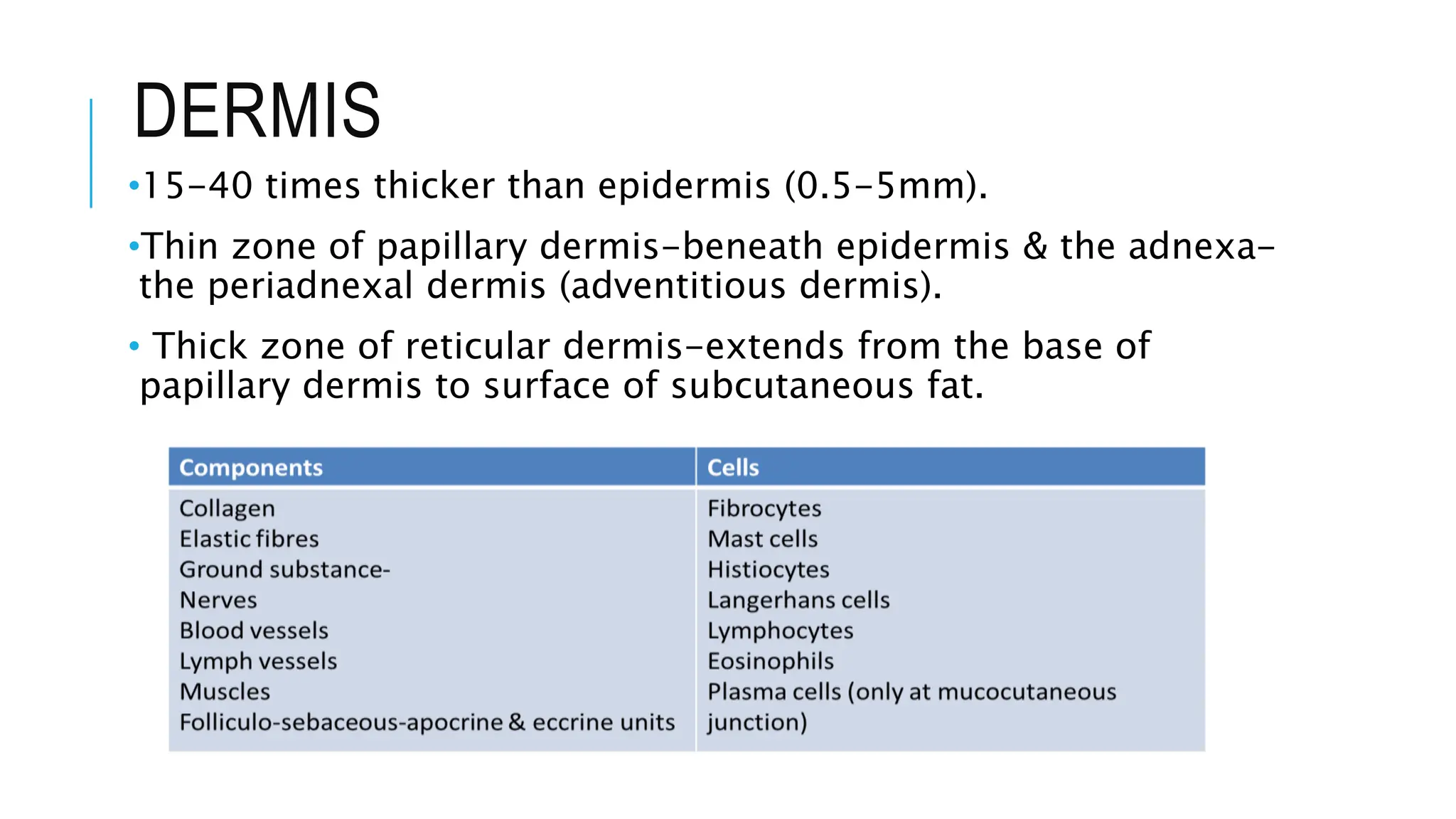
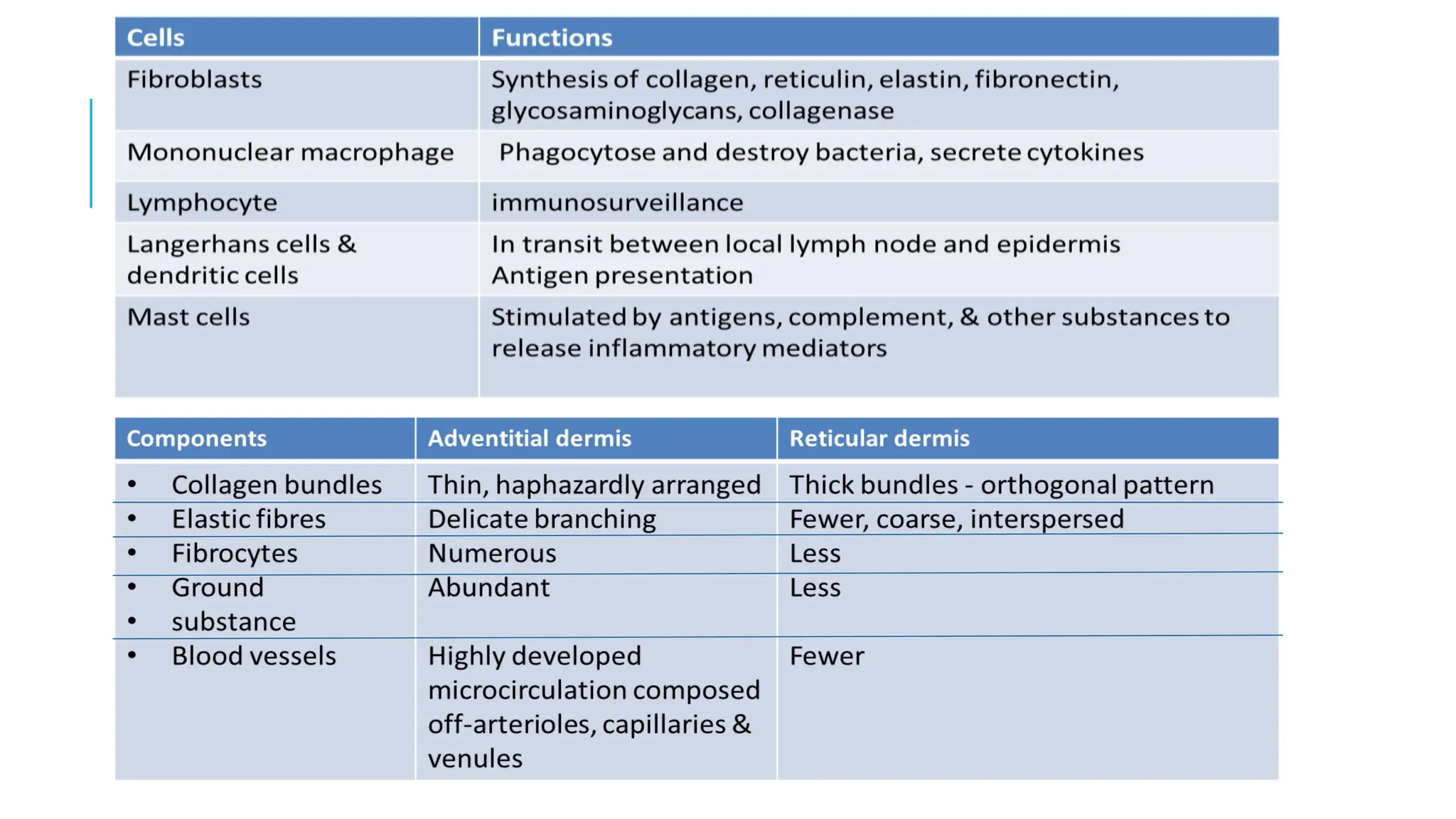
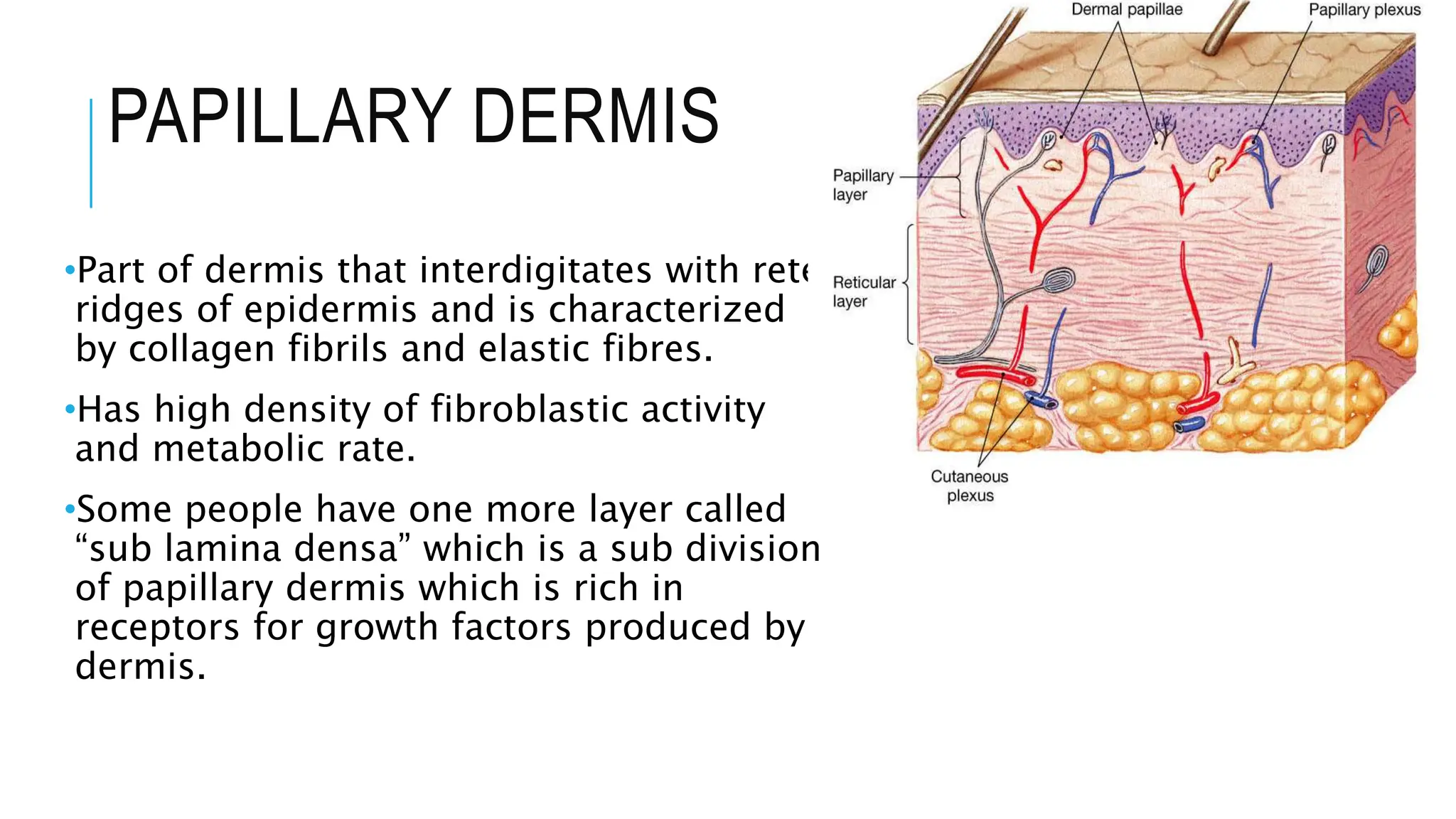
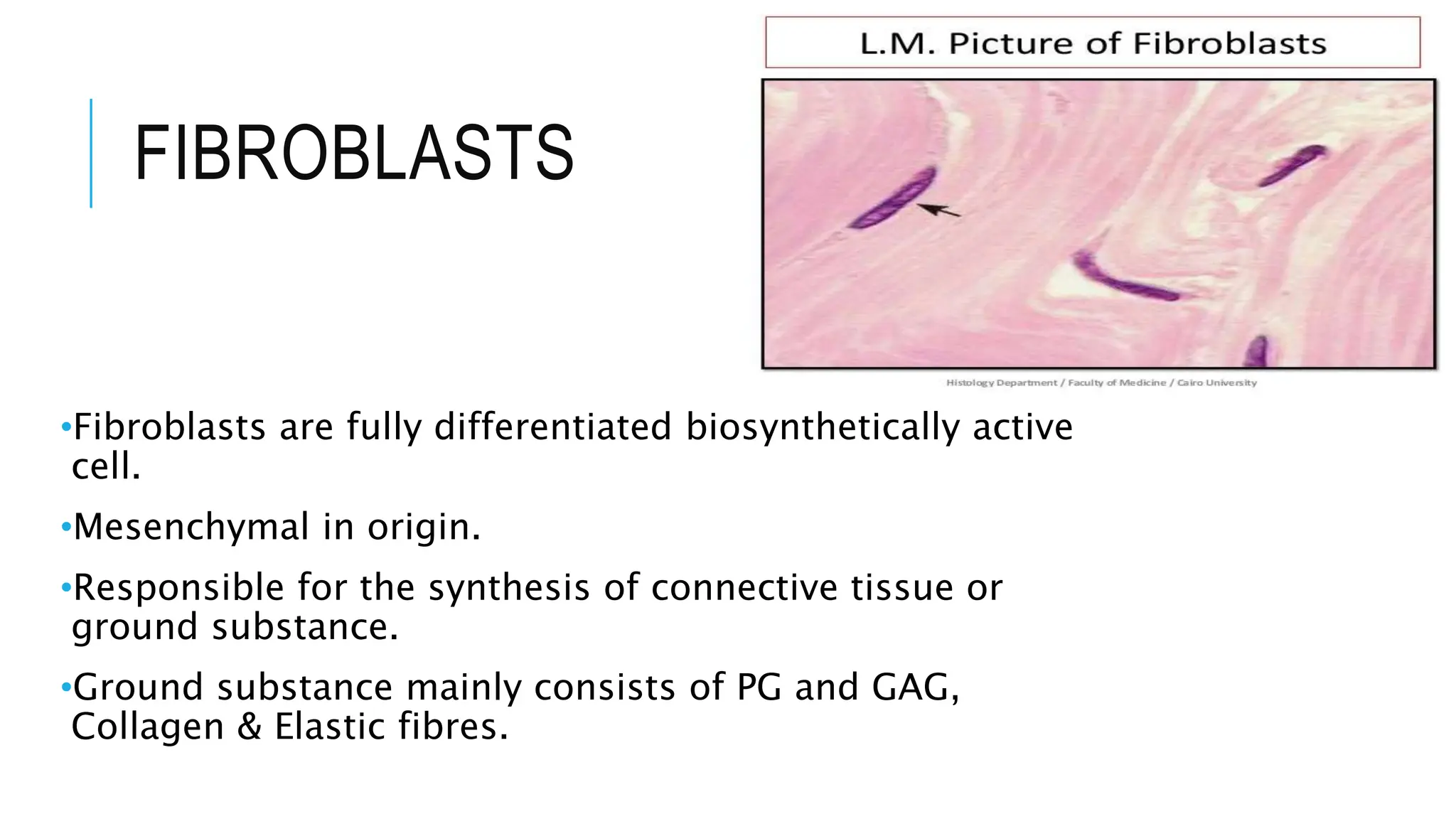
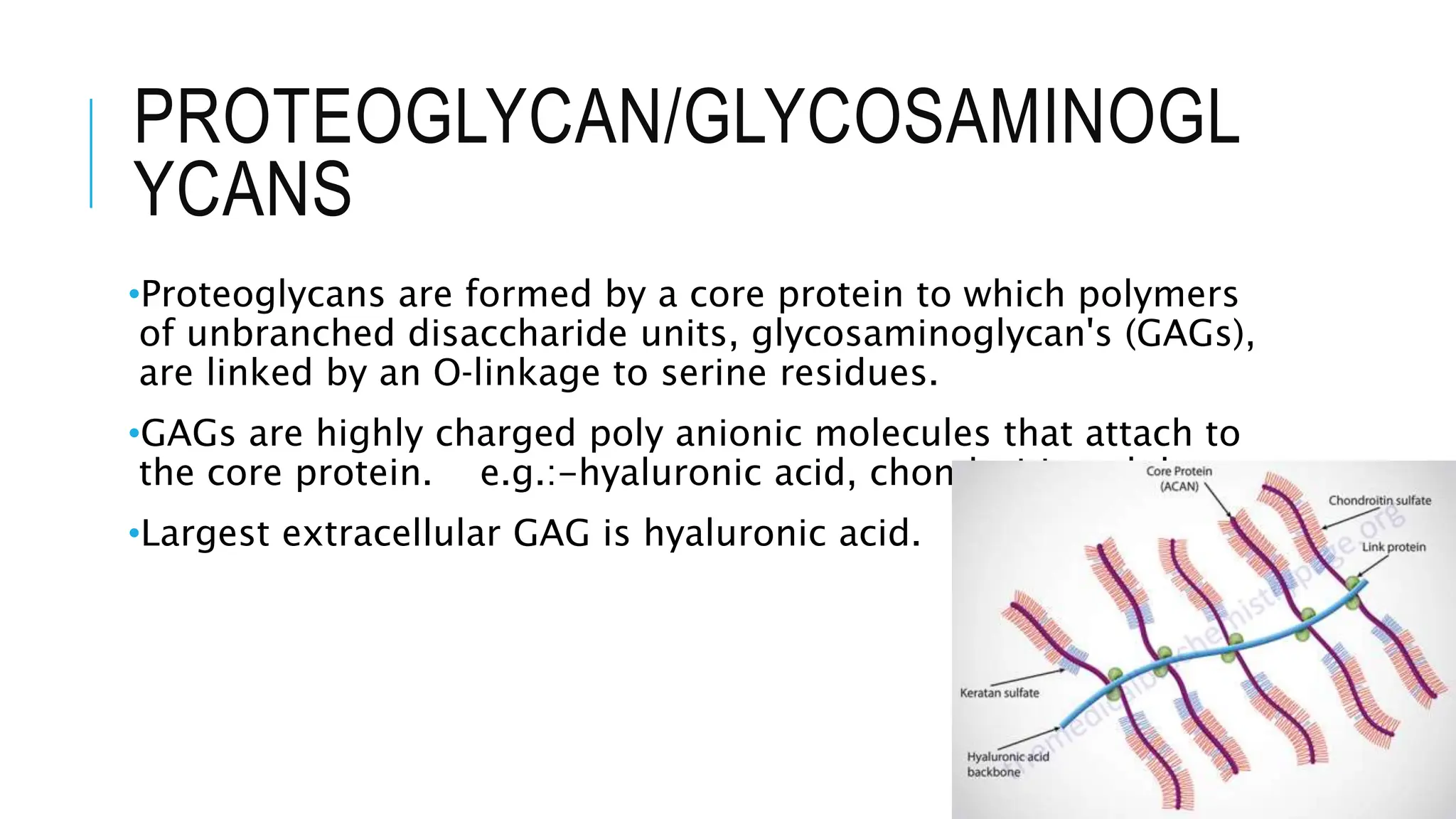
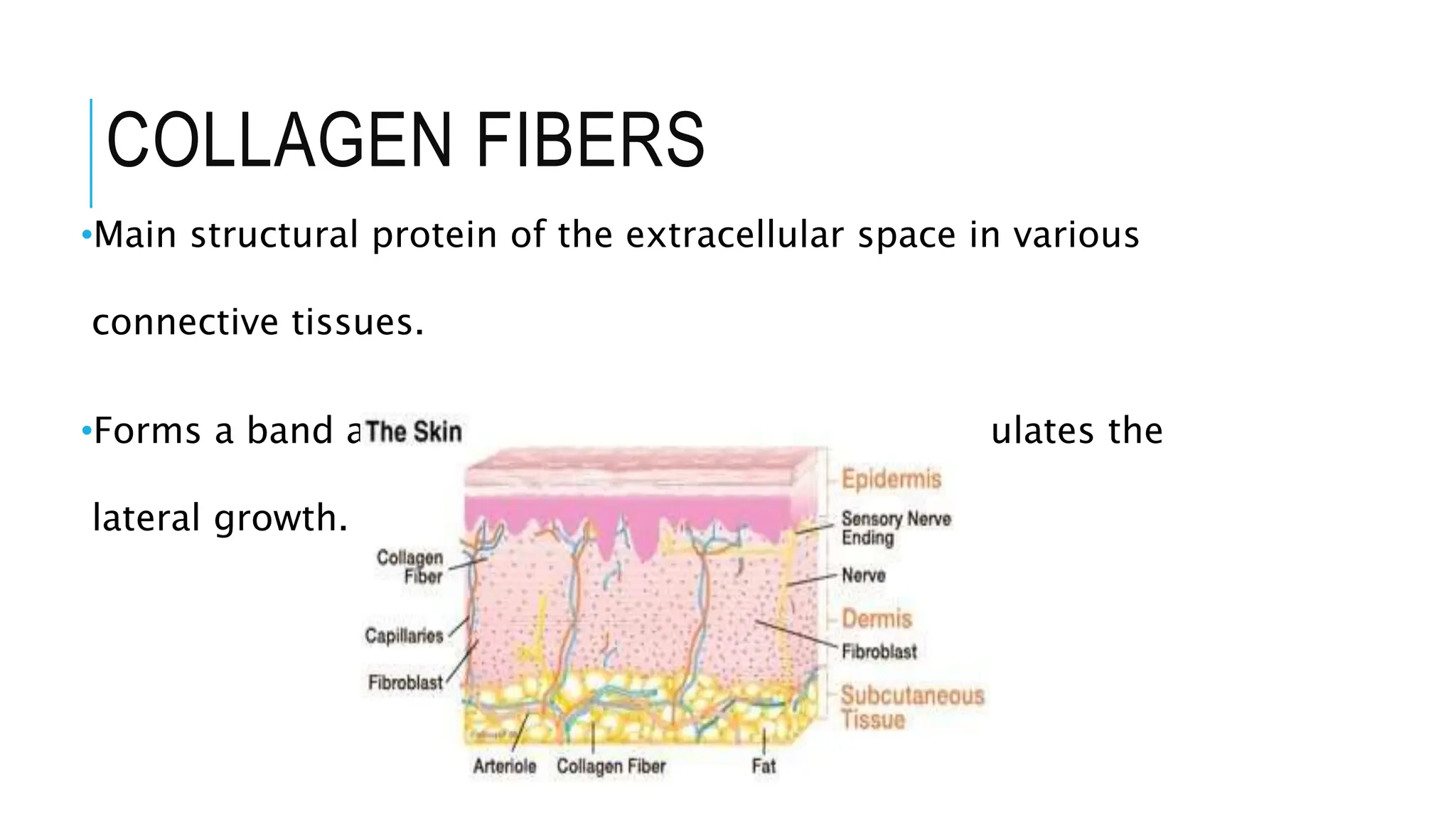
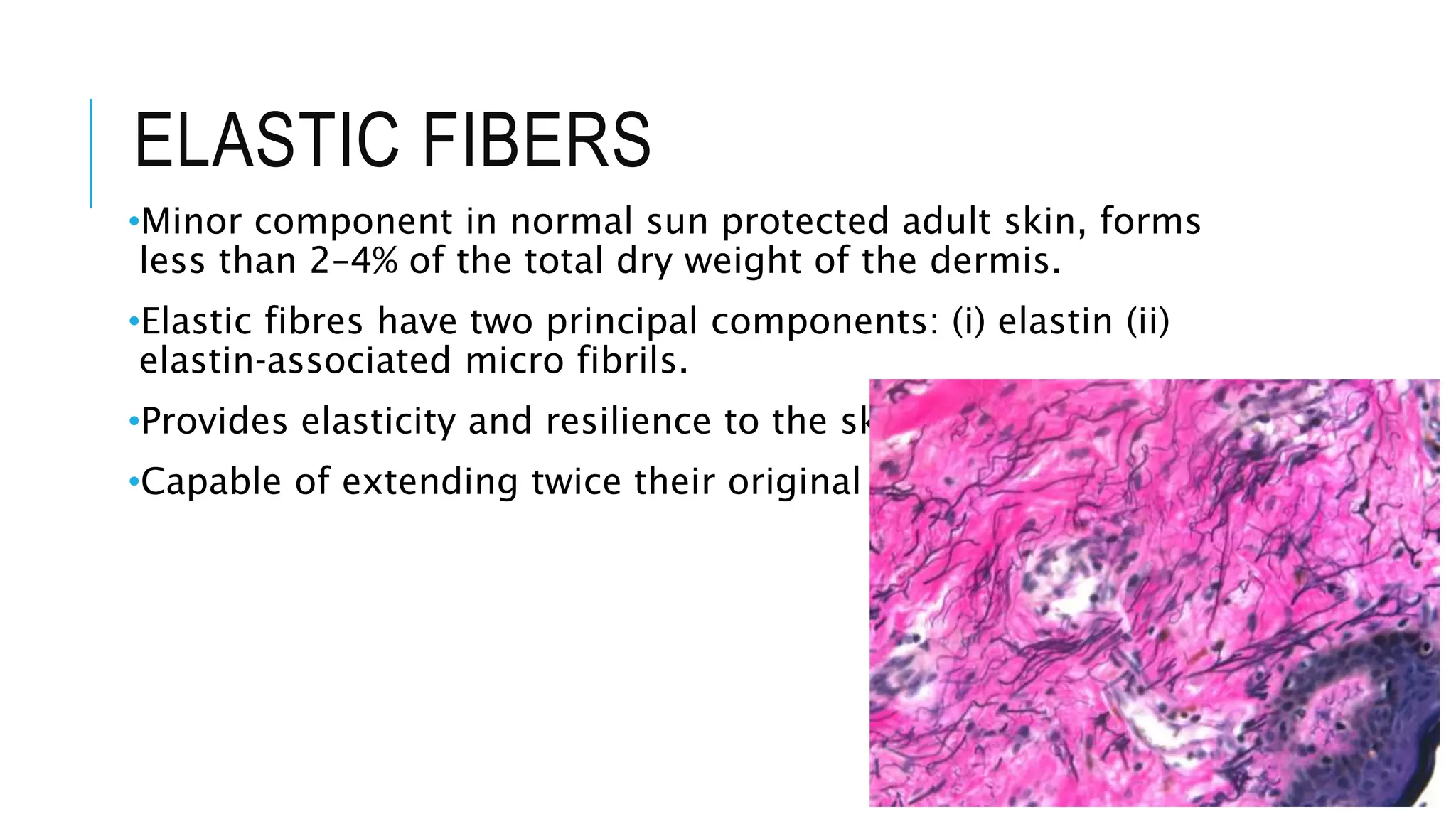
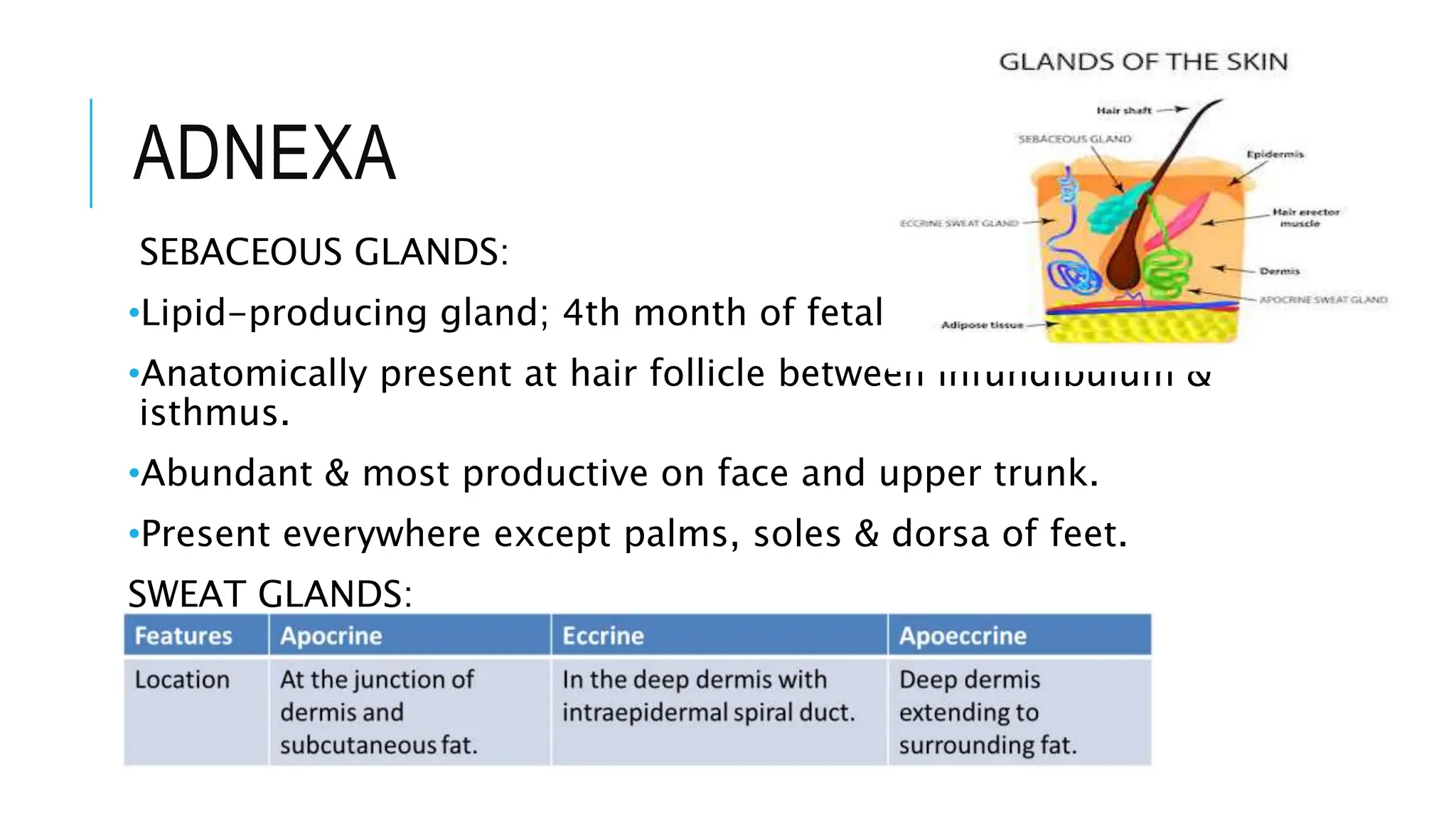
The document provides a comprehensive overview of skin anatomy, emphasizing its layers (epidermis, dermis, and subcutaneous layer) and their functions, including protection and physiological roles such as immunity and temperature regulation. It details the structure and function of various skin cells, including keratinocytes, melanocytes, and Langerhans cells, as well as connective tissue components like collagen and elastic fibers. Additionally, it covers embryological development, skin aging, and the role of skin adnexa such as sebaceous and sweat glands.
![REFERENCES
•Yousef H, Alhajj M, Sharma S. Anatomy, Skin (Integument),
Epidermis. [Updated 2020 Jul 27]. In: StatPearls [Internet].
Treasure Island (FL): StatPearls Publishing; 2020 Jan
•Agarwal S, Krishnamurthy K. Histology, Skin. [Updated 2020 Jul
3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls
Publishing; 2020 Jan
•Garza L. developmental biology of skin. In Kang S, Amagai M,
Bruckner AL, Enk AH, Margolis DJ, Orringer AS editors.
Fitzpatrick’s Dermatology in General medicine, 9th edn. Mc
Graw Hill Company, 2019;4,49-61.](https://image.slidesharecdn.com/mohnishpowerpoint-240522053755-25802d09/75/Structure-and-Anatomy-of-Skin-Layer-by-Layer-43-2048.jpg)