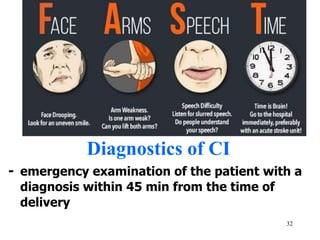
Cerebrovascular diseases are the third leading cause of death and a primary cause of disability. 30% of stroke patients die within the first month, and 45-48% die by the end of the year. Strokes can be classified as acute (transient or permanent) or chronic. Transient ischemic attacks are temporary episodes caused by temporary blockages, while permanent strokes include cerebral infarction (85%) and hemorrhages. Diagnosis involves imaging tests and analysis of risk factors. Treatment depends on the type of stroke but generally focuses on stabilization, blood pressure control, and prevention of complications.