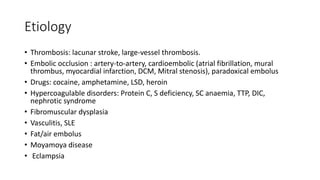
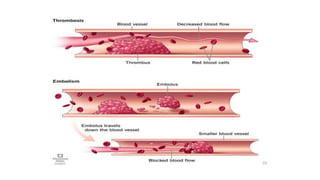
- Ischemic stroke is the second leading cause of death worldwide and is caused by occlusion of cerebral blood vessels leading to brain tissue death.
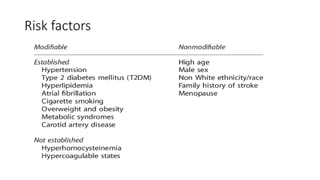
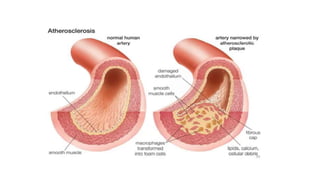
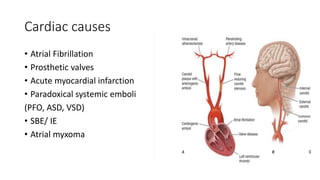
- Risk factors include atrial fibrillation, hypertension, diabetes, and smoking.
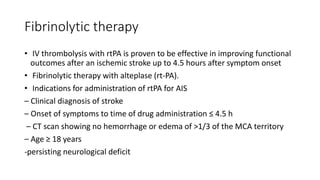
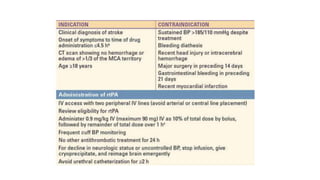
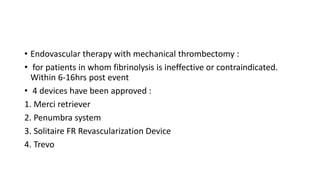
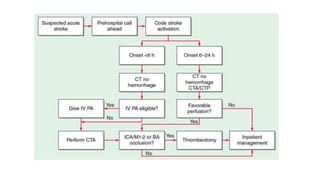
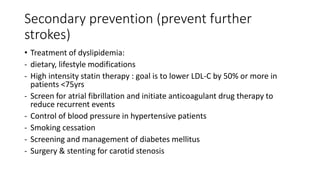
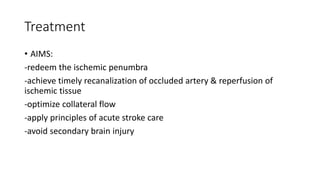
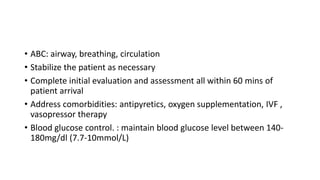
- Treatment involves stabilizing the patient, administering fibrinolytic drugs like rtPA within 4.5 hours, or performing a mechanical thrombectomy for large vessel occlusions. Long term management focuses on prevention of recurrence through antithrombotic drugs and controlling risk factors.

![• Stroke registry in Ibadan gave the annual incidence of stroke in
Nigerians as 26 per 100,000 populations
• At LASUTH stroke was the commonest cause of neurological
admissions
• In Nigeria cerebral ischemia accounted for 64%, ICH for 19% and SAH
for 6% of all strokes
• A cross sectional study between Jan 2010 and July 2013 in NHA
showed 62.5% had ischemic stroke while ICH 30.5% and SAH was
2.9%.[Nura H.A et-al]](https://image.slidesharecdn.com/ischemic20stroke-240415191242-da546932/85/Ischaemic-stroke-pathogenesis-and-treatment-6-320.jpg)


![Blood pressure control
• For patients who are not candidates for fibrinolytic therapy, current
guidelines recommend permitting moderate hypertension in most
patients with acute ischemic stroke.
• The exceptions would be patients who have active comorbidities (eg,
aortic dissection, acute myocardial infarction [MI],
• Acute antihypertensive therapy is typically indicated when blood
pressure is >220/120 mm Hg,(ASA 2013)
• For those who have received IV thrombectomy blood pressure should
be maintained](https://image.slidesharecdn.com/ischemic20stroke-240415191242-da546932/85/Ischaemic-stroke-pathogenesis-and-treatment-40-320.jpg)