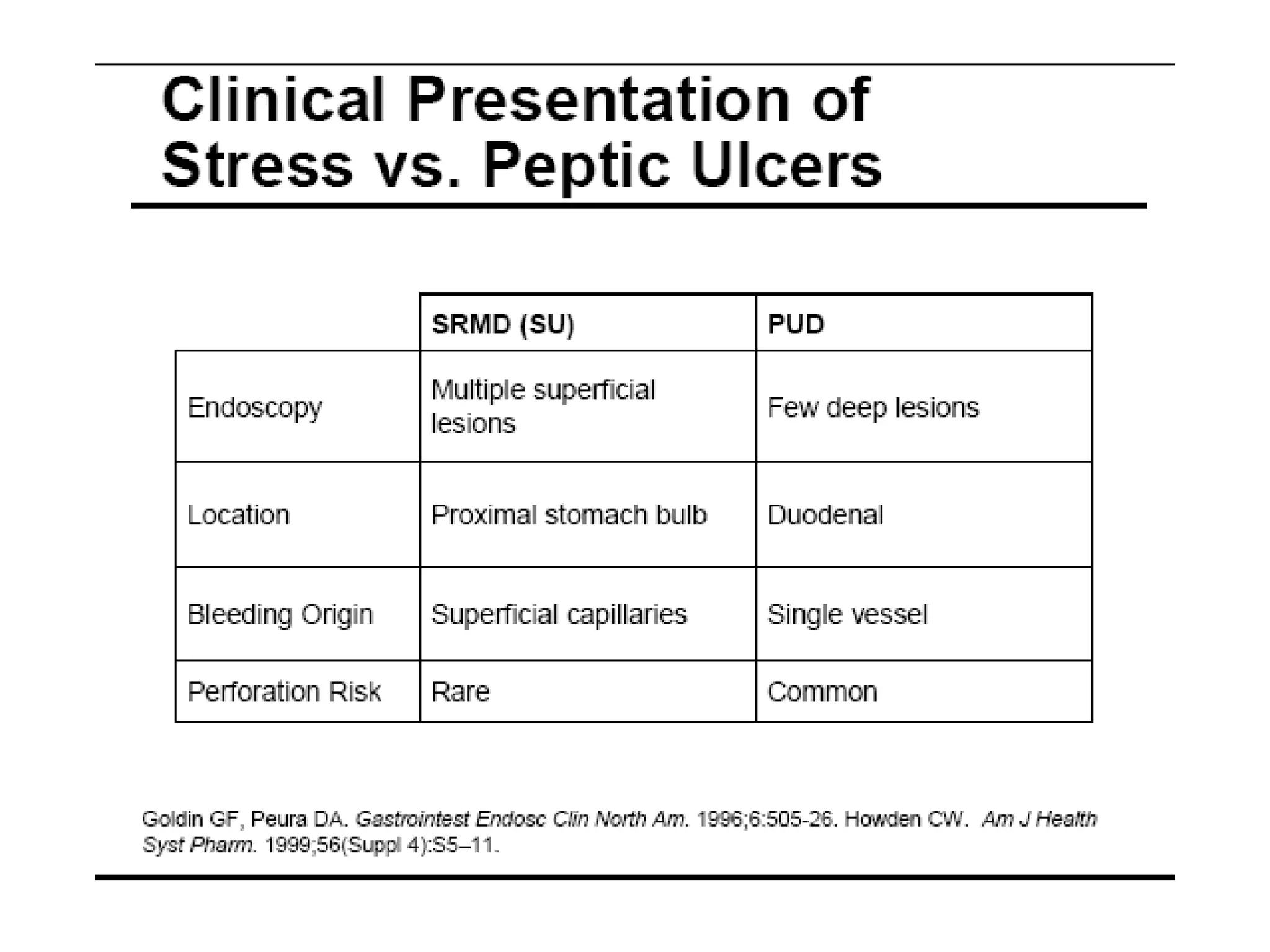
This document summarizes stress ulcer prophylaxis in the ICU. It discusses that stress ulcers are superficial gastric erosions caused by impaired blood flow to the stomach that prevents normal mucosal lining replacement. Left untreated, stress ulcers can lead to translocation of bacteria and hemorrhage. Patients at highest risk include those with head injuries, major burns, surgery, trauma, shock or ventilation over 48 hours. Prevention strategies focus on maintaining splanchnic blood flow, enteral nutrition, and pharmacologic treatments.