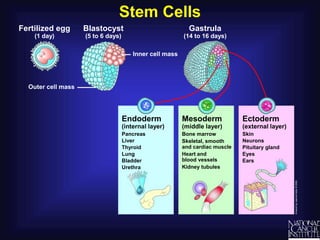
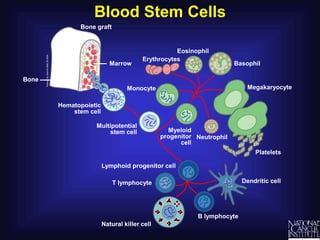
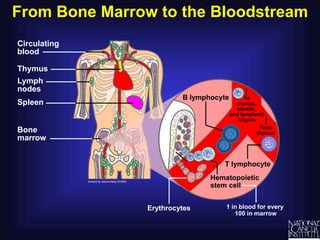
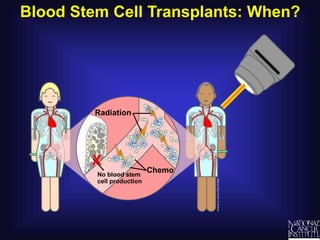
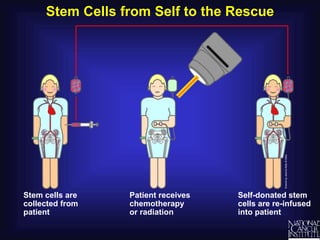
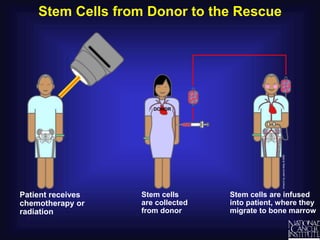
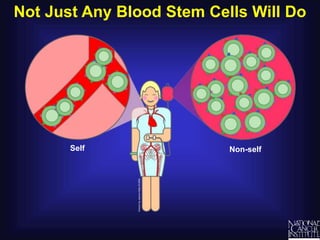
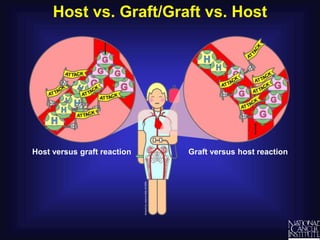
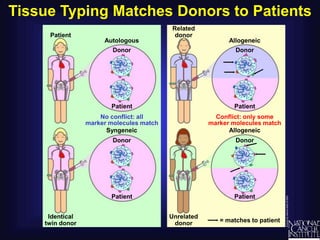
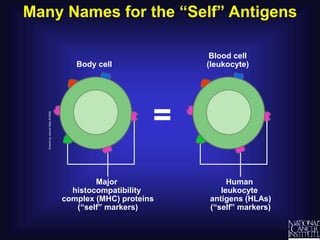
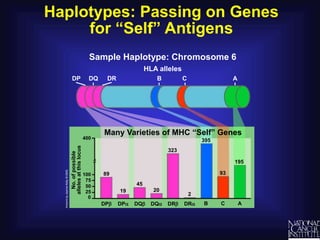
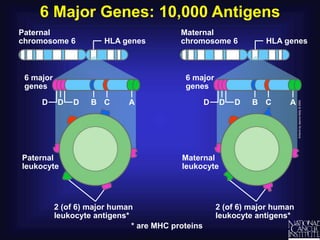
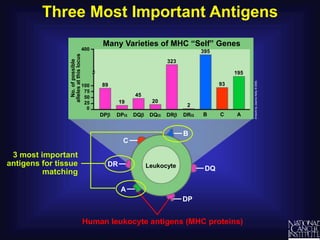
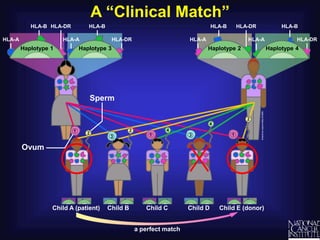
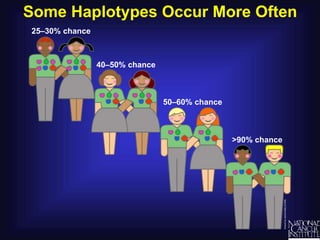
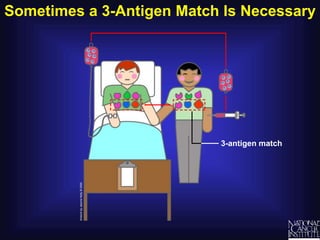
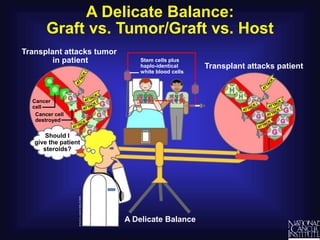
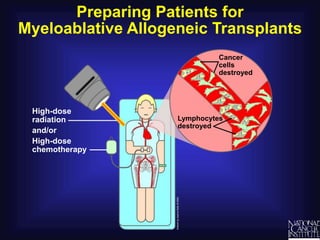
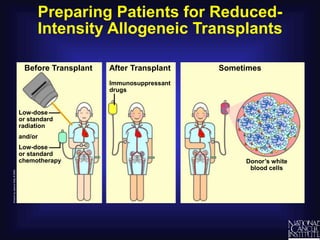
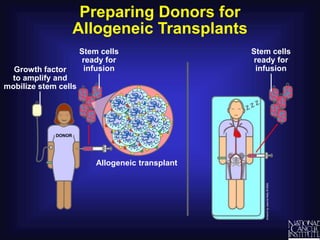
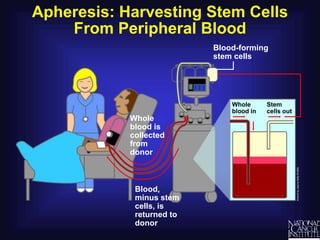
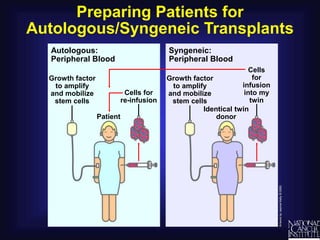
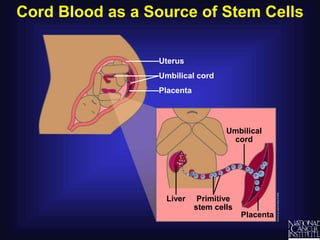
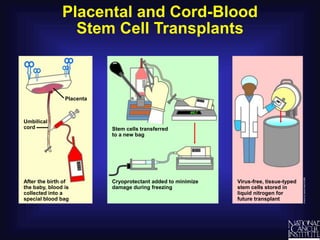
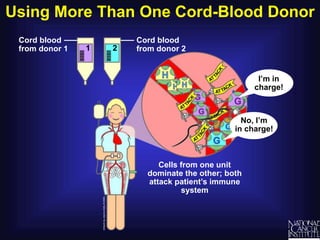
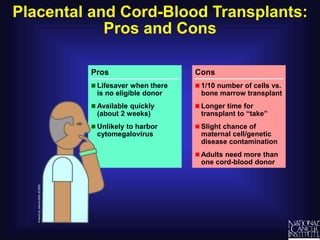
This document discusses blood stem cell transplantation. It begins by explaining how bone marrow produces blood-forming stem cells and how transplantation of healthy stem cells from sources like marrow, blood or cord blood can help patients whose hematopoietic cells have been damaged by diseases or treatments like cancer. It then covers topics like tissue typing to match donors and recipients, the risks of graft-versus-host disease, and how autologous, syngeneic and allogeneic transplants work. The document provides diagrams and explanations of these concepts over several slides.