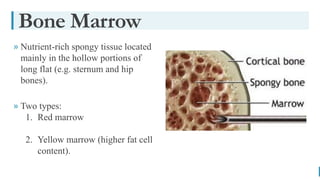
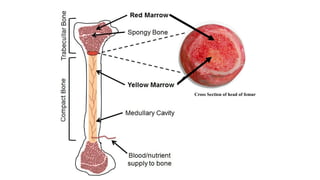
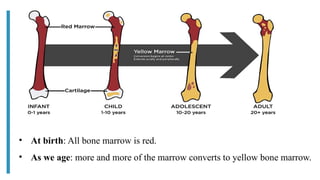
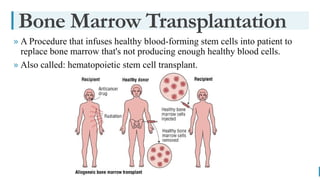
This presentation provides a comprehensive overview of bone marrow transplantation (hematopoietic stem cell transplantation).
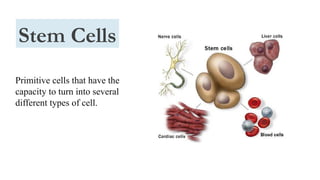
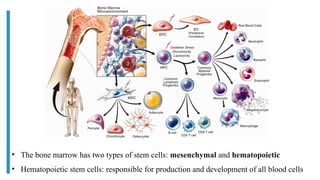
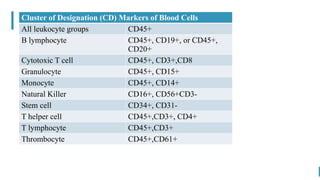
It explains bone marrow physiology, stem cell biology, and the principles of transplantation.
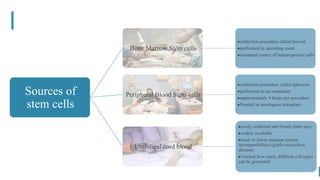
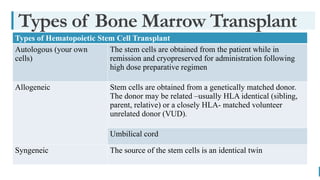
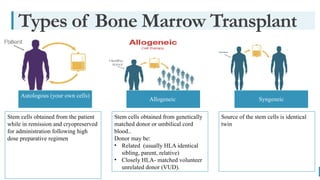
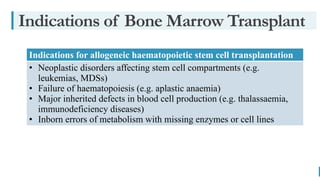
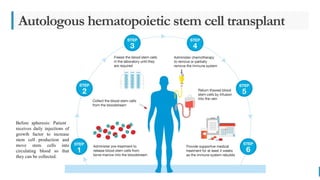
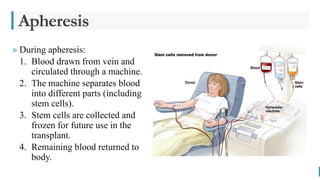
Types of transplant including autologous, allogeneic, and syngeneic are discussed along with stem cell sources.
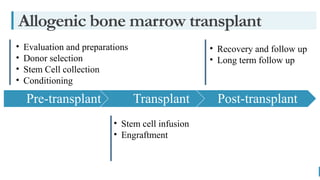
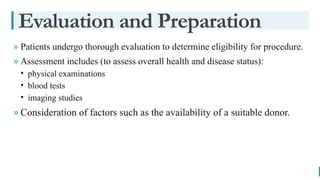
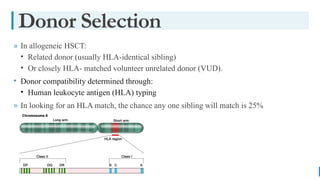
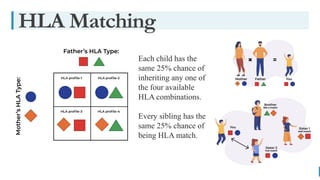
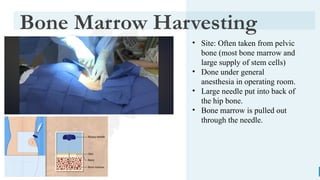
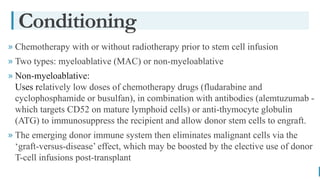
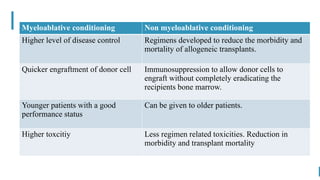
The presentation covers patient evaluation, donor selection, HLA matching, stem cell collection, conditioning regimens, infusion, engraftment, recovery, and long-term follow-up.
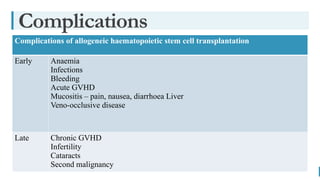
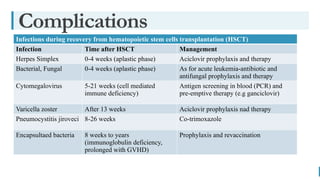
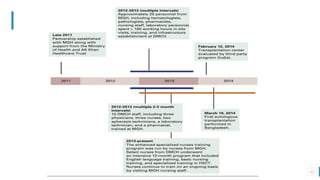
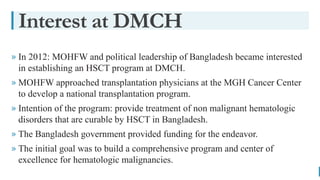
Complications and the development of a national HSCT program in Bangladesh are also highlighted.
Intended for medical students, residents, and physicians.