Staphylococcus aureus (S. aureus) is a common, highly pathogenic bacterium that is responsible for many skin, soft tissue, and systemic infections in humans. It is one of the most clinically important bacteria in medicine.
1. Basic Description
Gram-positive cocci
Arranged in clusters (like grapes 🍇)
Non-motile
Non-spore forming
Facultative anaerobe (can survive with or without oxygen)
2. Habitat (Where it is found)
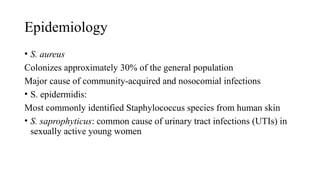
S. aureus is part of normal human flora, commonly found in:
Anterior nares (nose) (most common site)
Skin
Throat
Perineum
Many people are carriers without being sick.
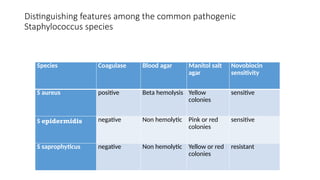
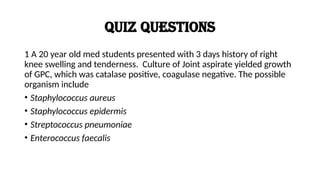
3. Key Laboratory Identification
Microscopy
Gram-positive cocci in clusters
Culture
Grows well on ordinary media.
On blood agar: shows beta-hemolysis (clear zone).
On mannitol salt agar (MSA):
Grows because it tolerates high salt.
Ferments mannitol → turns agar yellow
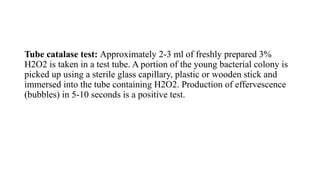
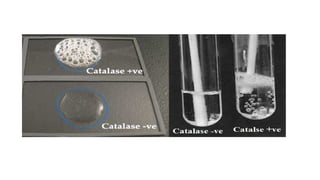
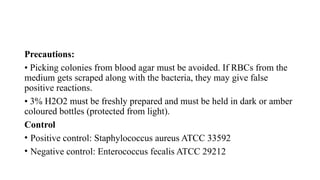
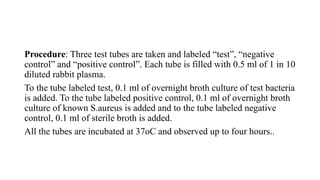
Biochemical Tests
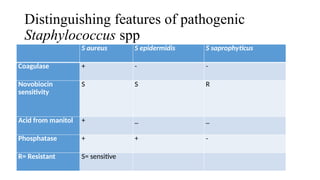
Catalase positive (bubbles with H₂O₂)
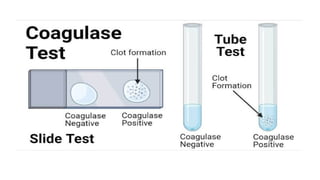
Coagulase positive (major differentiating feature from other staphylococci)
DNase positive
4. Important Virulence Factors
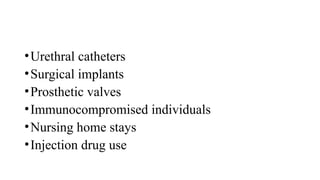
S. aureus is dangerous because it has many virulence mechanisms:
A. Surface factors
Protein A: binds Fc portion of IgG → prevents opsonization/phagocytosis
Capsule/slime layer: helps evade immunity and form biofilm
Adhesins: allow attachment to tissues and prosthetic materials
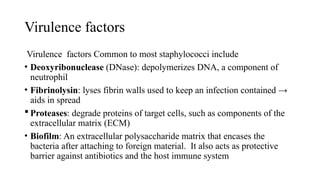
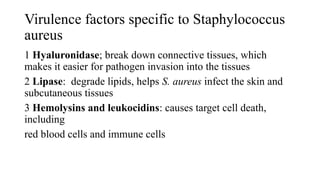
B. Enzymes
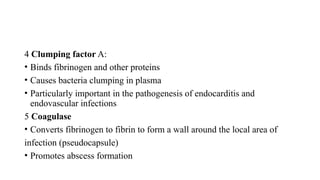
Coagulase: forms fibrin clot → hides bacteria
Hyaluronidase: spreads infection through tissues
Staphylokinase: dissolves clots
Lipase: helps colonize skin
β-lactamase (penicillinase): antibiotic resistance
C. Toxins
α-toxin: damages cell membranes
Panton-Valentine leukocidin (PVL): destroys WBCs → severe skin infections and necrotizing pneumonia
Exfoliative toxin: causes scalded skin syndrome
Enterotoxin: causes food poisoning
TSST-1 (toxic shock syndrome toxin): causes toxic shock syndrome
5. Diseases Caused by Staphylococcus aureus
A. Skin and Soft Tissue Infections (most common)
Boils (furuncles)
Carbuncles
Impetigo
Cellulitis
Abscesses
Wound infections
Classic feature: pus formation (pyogenic infection)
B. Deep/Systemic Infections
Pneumonia (especially post-influenza, can be necrotizing)
Osteomyelitis
Septic arthritis
Endocarditis (especially IV drug users → tricuspid valve)
Bacteremia and sepsis
Brain abscess
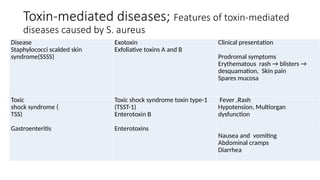
C. Toxin-Mediated Conditions
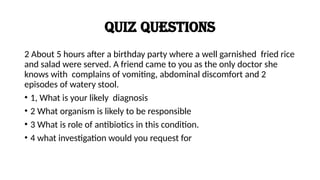
Food Poisoning
Rapid onset vomiting (1–6 hours)
Due to preformed enterotoxin
Usually no fever
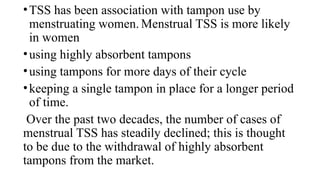
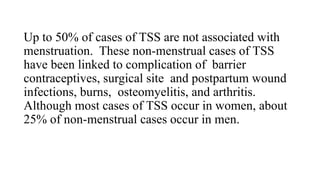
Toxic Shock Syndrome (TSS)
High fever
Hypotension/shock
Diffuse rash → later desquamation
Multi-organ failure
Staphylococcal Scalded Skin Syndrome (SSSS)
Mostly in infants/children
Skin peeling and blistering
Caused by exfoliative toxin
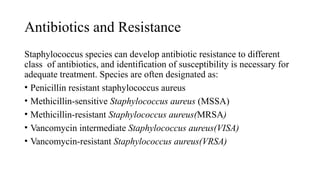
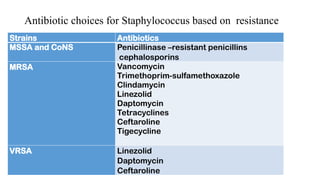
6. Antibiotic Resistance
MRSA (Methicillin Resistant S. aureus)
Caused by mecA gene
Produces altered PBP (PBP2a) → resistance to beta-lactams
Often resistant to multiple drugs
Treatment Options
MSSA: cloxacillin/flucloxacillin, nafcillin, cefazolin
MRSA: vancomycin, linezolid, daptomycin (not for pneumonia)