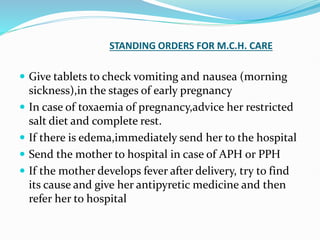
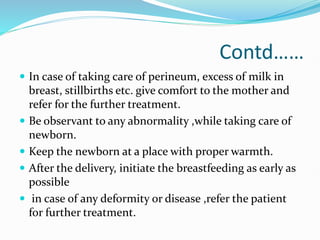
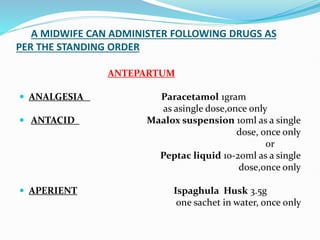
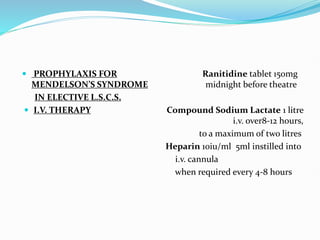
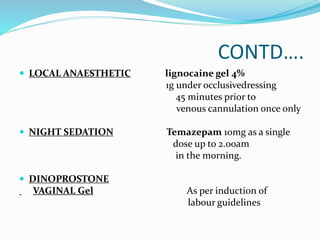
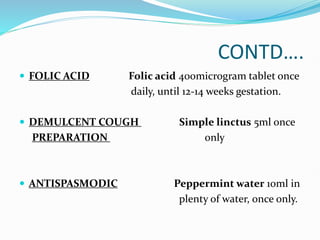
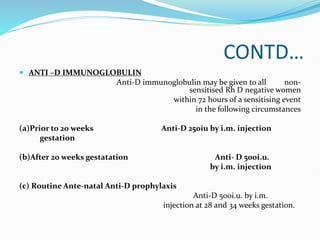
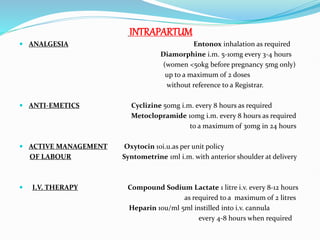
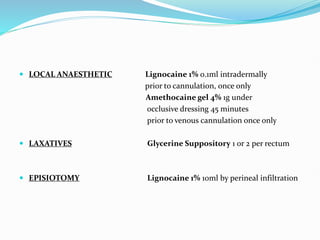
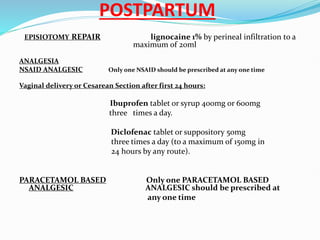
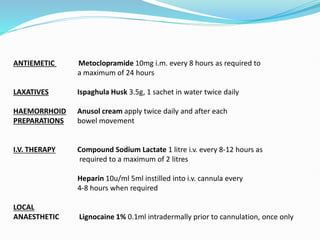
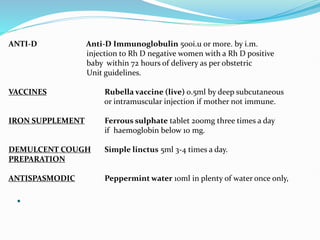
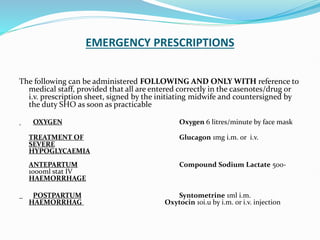
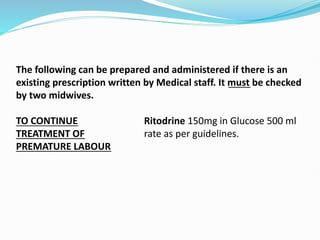
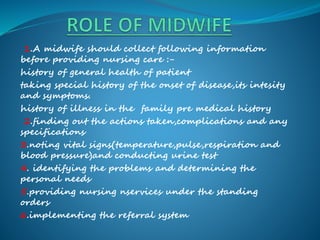
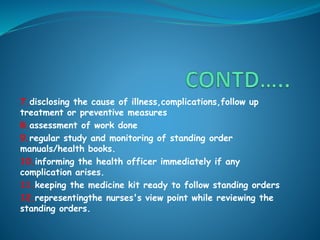
The document discusses standing orders that allow midwives to provide certain medical treatments to patients without an individual doctor's prescription. It defines standing orders as specific directions and orders that allow nurses, midwives, and other medical staff to provide treatment when doctors are unavailable. The document outlines the objectives, uses, and types of standing orders. It then lists the treatments and medications that midwives are authorized to administer under standing orders for antepartum, intrapartum, postpartum, and emergency situations. The treatments include analgesics, antacids, anti-hemorrhage drugs, IV fluids, local anesthetics, antibiotics, and more. It stresses that midwives must be properly trained and follow protocols when administering treatments under