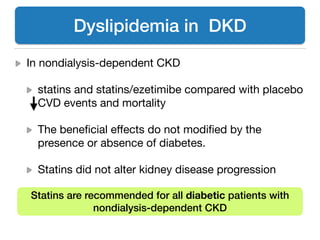
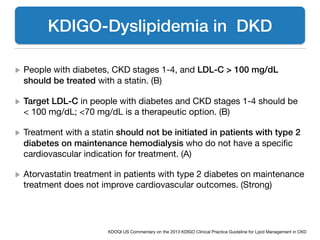
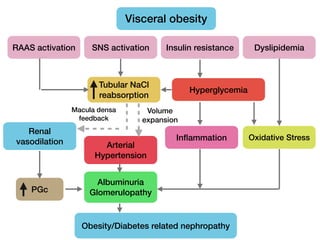
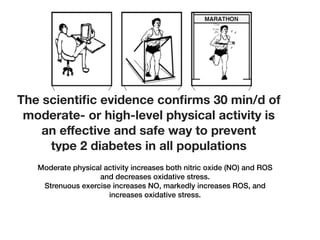
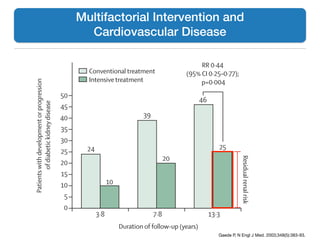
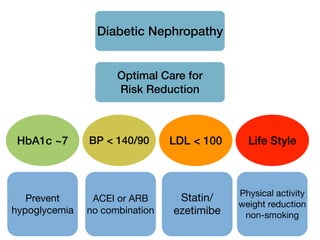
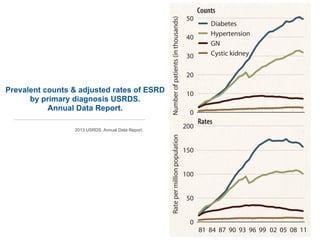
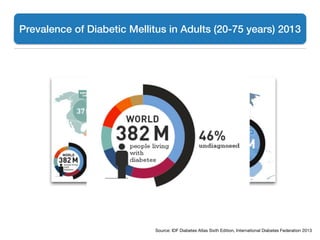
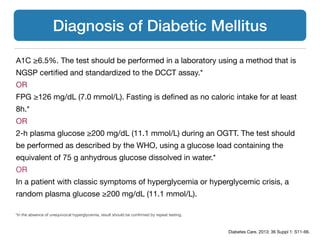
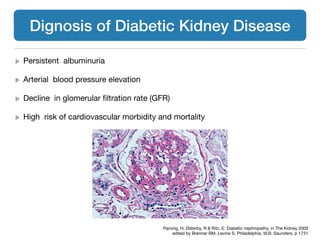
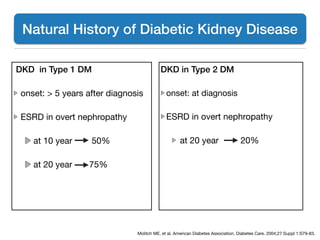
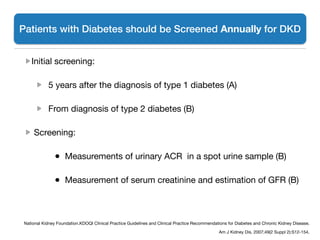
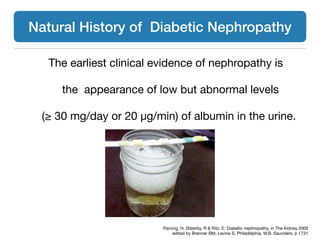
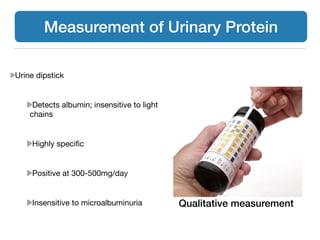
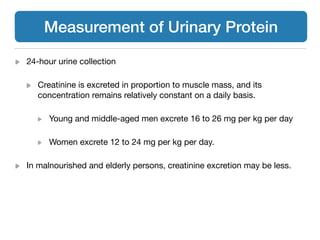
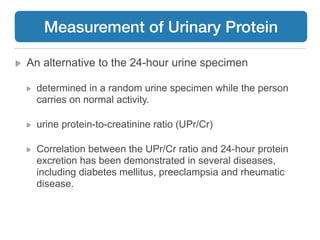
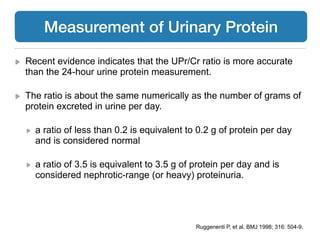
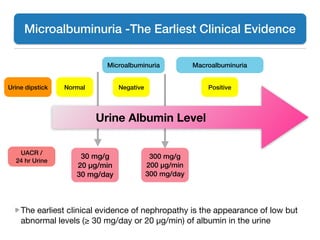
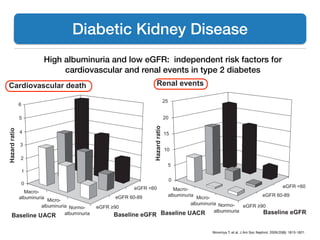
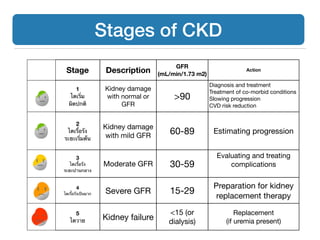
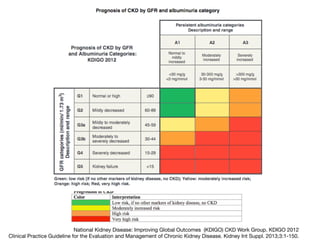
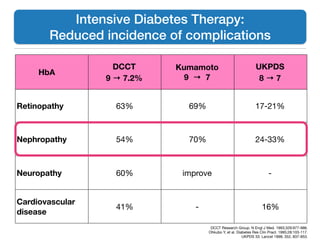
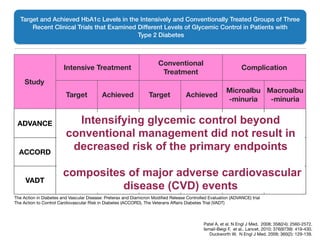
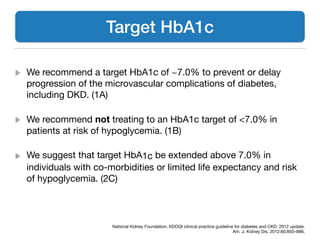
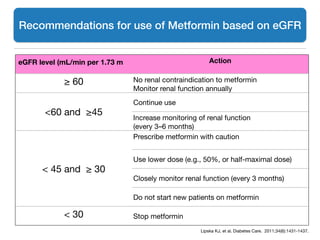
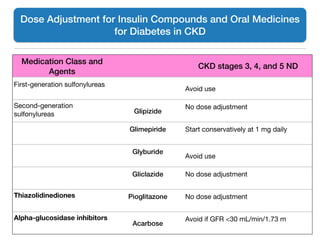
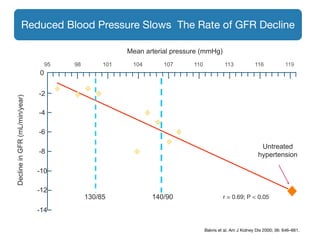
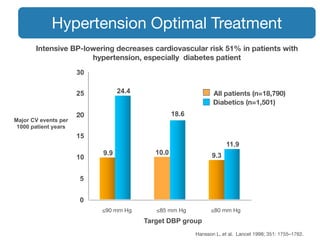
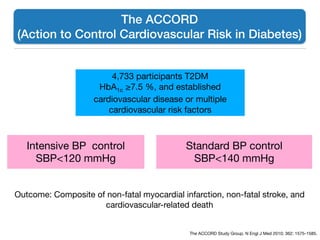
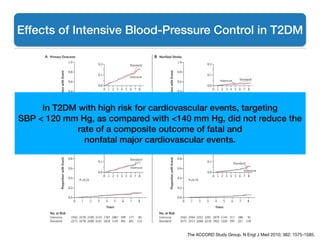
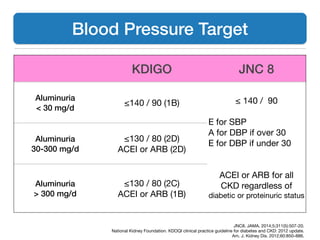
This document discusses diabetic kidney disease (DKD). It begins by outlining the prevalence and scope of DKD, defining DKD, and listing the optimal management of DKD as topics. It then provides details on the diagnosis of DKD, including the earliest clinical evidence being microalbuminuria. It discusses screening guidelines and measuring urinary protein. It outlines the stages of chronic kidney disease and strategies for treating DKD, including blood glucose control, blood pressure control, and lifestyle modifications. Target HbA1c levels for preventing DKD complications are also discussed.
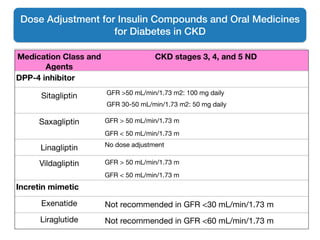
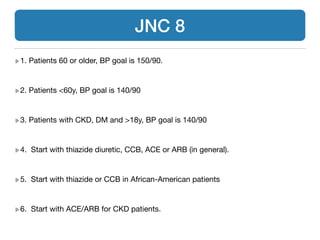
![Life-table plot of effects of allocation to simvastatin plus ezetimibe versus placebo on major atherosclerotic events
Numbers remaining at risk of a first major atherosclerotic event at the beginning of each year are shown for both treatment groups.
Lowering LDL-C reduces cardiovascular events in
a wide range of patients with diabetes and CKD
Baigent C, et al. Lancet. 2011;377(9784):2181-2192.
for triglyceri
3023 (33%
dialysis at ra
496 [5%] p
cholesterol
dialysis tha
2·9 [SD 0·9
of 6247 patie
creatinine,
Modification
26·6 (SD 13
had Kidney
3 disease (
(43%) stage
and 1221 (20
1·73 m²). Am
dialysis with
creatinine r
30 mg/g, 2
2359 (42%)
The medi
surviving p
period, sligh
ezetimibe d
simvastatin
finding was
*In patients initially allocated to simvastatin, no 1-year sample was collected, while samples scheduled for collection at
2·5 and 4 years were collected at 1·5 and 3 years after rerandomisation.
Table 2: Average use of study simvastatin plus ezetimibe or non-study statin and average change in
plasma LDL cholesterol from baseline, by period of follow-up
Figure 2: Life-table plot of effects of allocation to simvastatin plus ezetimibe versus placebo on major
atherosclerotic events
Numbers remaining at risk of a first major atherosclerotic event at the beginning of each year are shown for both
treatment groups.
543210
4620
4650
4204
4271
3849
3939
3469
3546
2566
2655
1269
1265
Years of follow-up
Number at risk
Placebo
Simvastatin
plus ezetimibe
0
5
10
15
20
25
Peoplesufferingevents(%)
Placebo
Simvastatin plus ezetimibe
Rate reduction 17% (95% CI 6–26%)
Log-rank p=0·0021
Rate Reduction 17%](https://image.slidesharecdn.com/2-160403141557/85/slide-47-320.jpg)