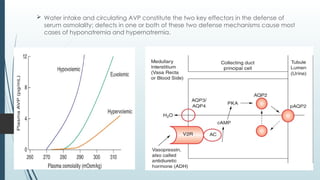
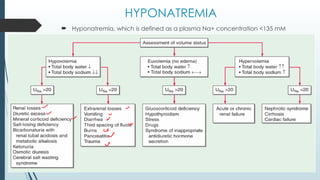
Hyponatremia and hypernatremia are disorders characterized by abnormal serum sodium concentrations due to issues with water homeostasis. Hyponatremia, defined as a plasma Na+ concentration <135 mM, can occur in various forms: hypovolemic, hypervolemic, and euvolemic, each with distinct causes and treatment approaches, while hypernatremia, with Na+ >145 mM, often presents with altered mental status and requires careful correction to avoid complications such as cerebral edema. Appropriate diagnostic evaluations and tailored treatments are critical for managing both conditions effectively.

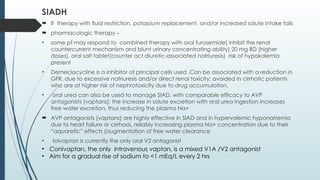
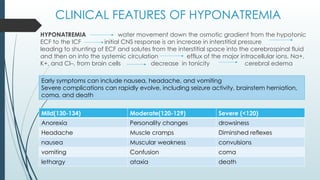
![HYPERVOLEMIC HYPONATREMIA
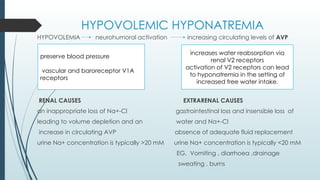
Increase in total-body Na+-Cl– that is accompanied by a proportionately greater
increase in total-body water leading to a reduced plasma Na+ concentration.
URINARY SODIUM >20MM
Acute or chronic renal failure
URINARY SODIUM <10 MM
• congestive heart failure [CHF]
( cardiac dysfunction in CHF)
• cirrhosis
peripheral vasodilation in cirrhosis
• nephrotic syndrome](https://image.slidesharecdn.com/sodiumdisorders-241230193322-da5c6373/85/sodium-disorders-hypo-and-hypernatremia-pptx-7-320.jpg)
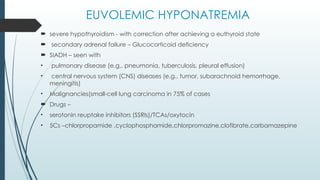
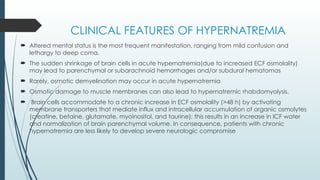
![TREATMENT OF HYPONATREMIA
First, the presence and/or severity of symptoms determine the urgency and goals of
therapy.
Patients with euvolemic hyponatremia due to SIAD, hypothyroidism, or secondary
adrenal failure will respond to successful treatment of the underlying cause, with an
increase in plasma Na+ concentration
Hypervolemic hyponatremia
improve by therapy of the
underlying cardiomyopathy
By using (ACE) inhibition
Hypovolemic hyponatremia
I.V hydration with isotonic NS
rapid reduction in AVP
brisk water diuresis text here
euvolemic hyponatremia
Respond to fluid restriction
The urine-to plasma electrolyte
ratio (urinary [Na+] +
[K+]/plasma [Na+])
• ratio oof >1 should be more
aggressively
restricted (<500 mL/d)
ratio of ~1 should be restricted
to 500–700 mL/d
• ratio <1 should be
restricted to <1 L/d](https://image.slidesharecdn.com/sodiumdisorders-241230193322-da5c6373/85/sodium-disorders-hypo-and-hypernatremia-pptx-12-320.jpg)