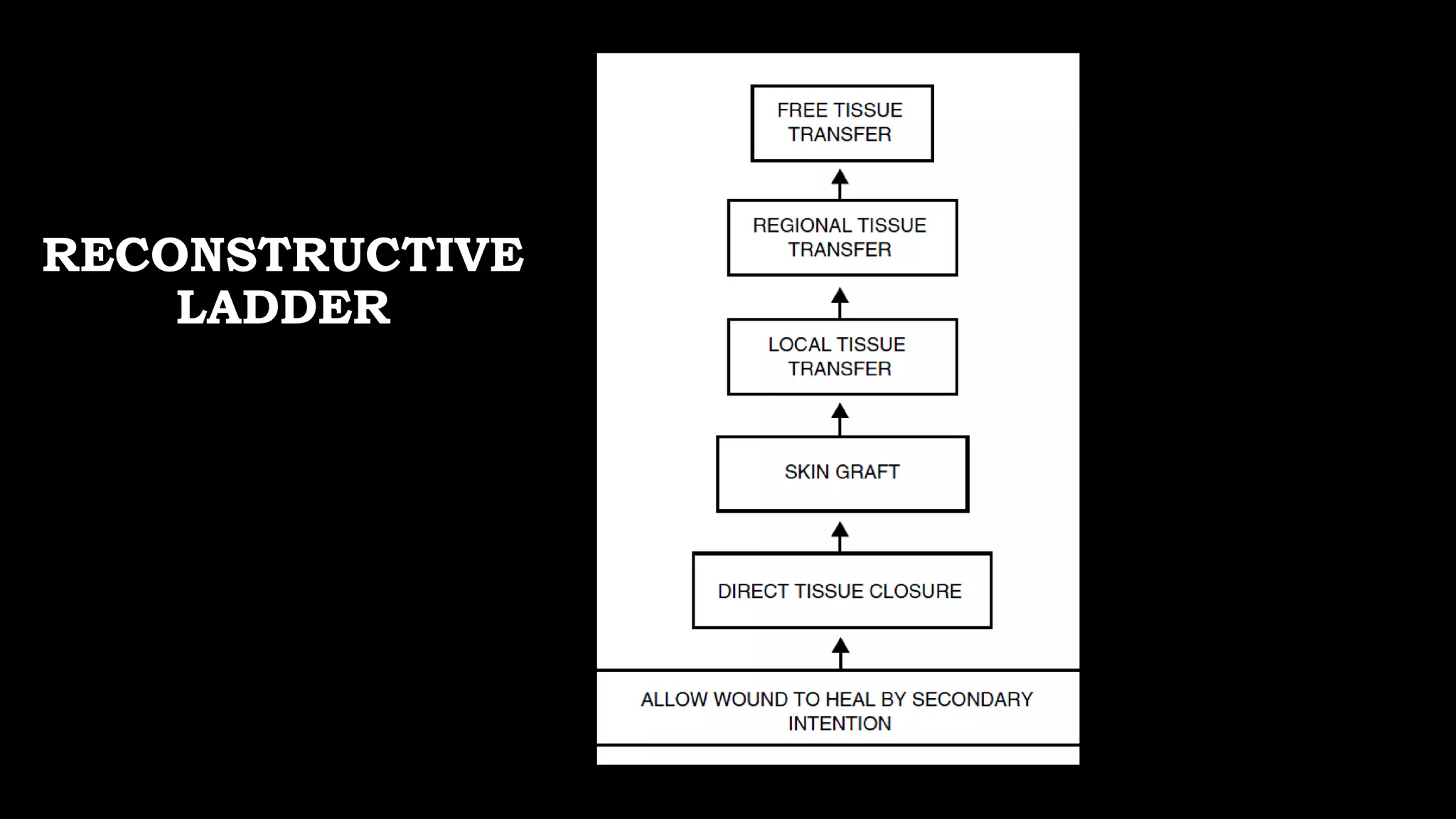
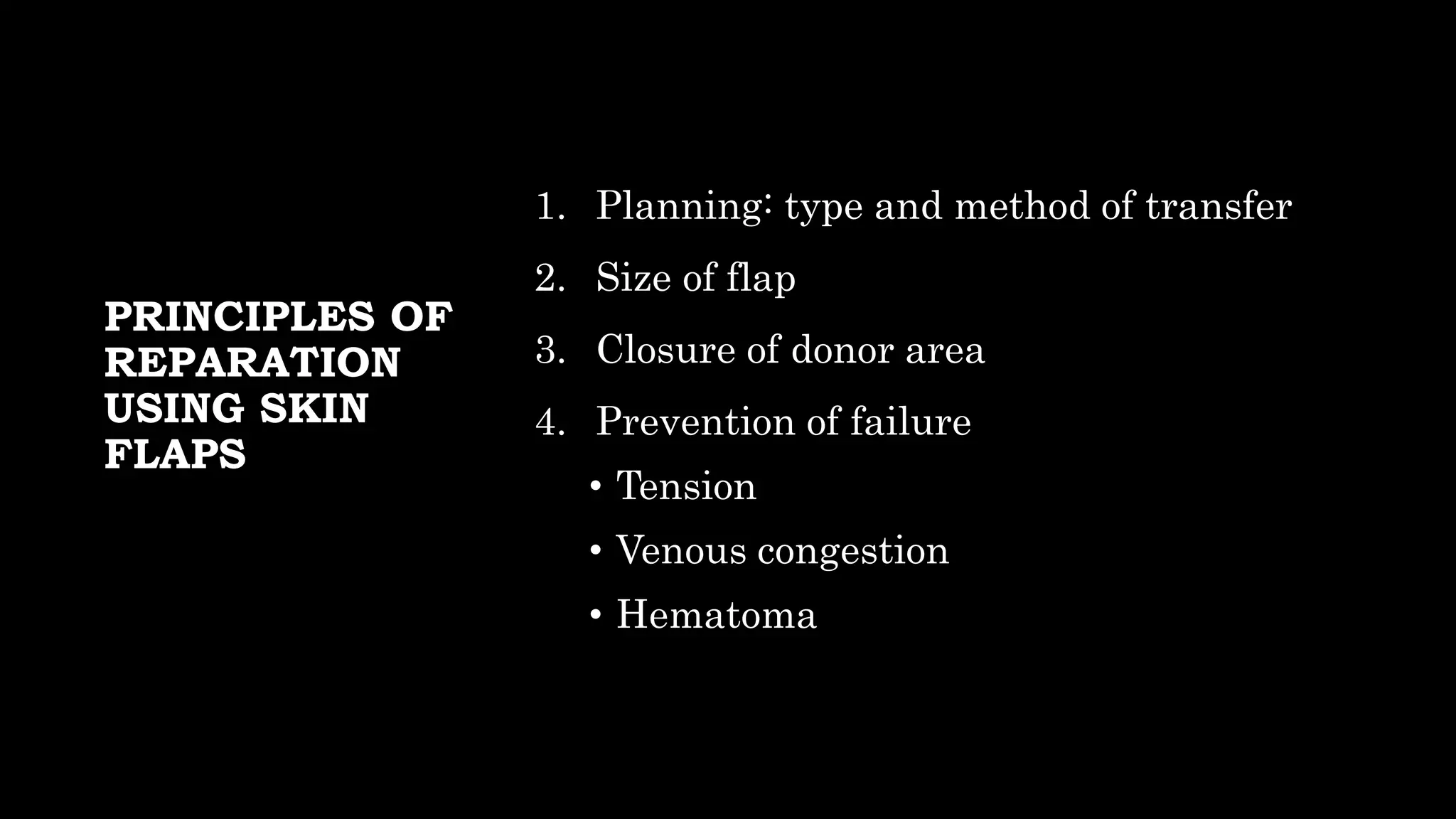
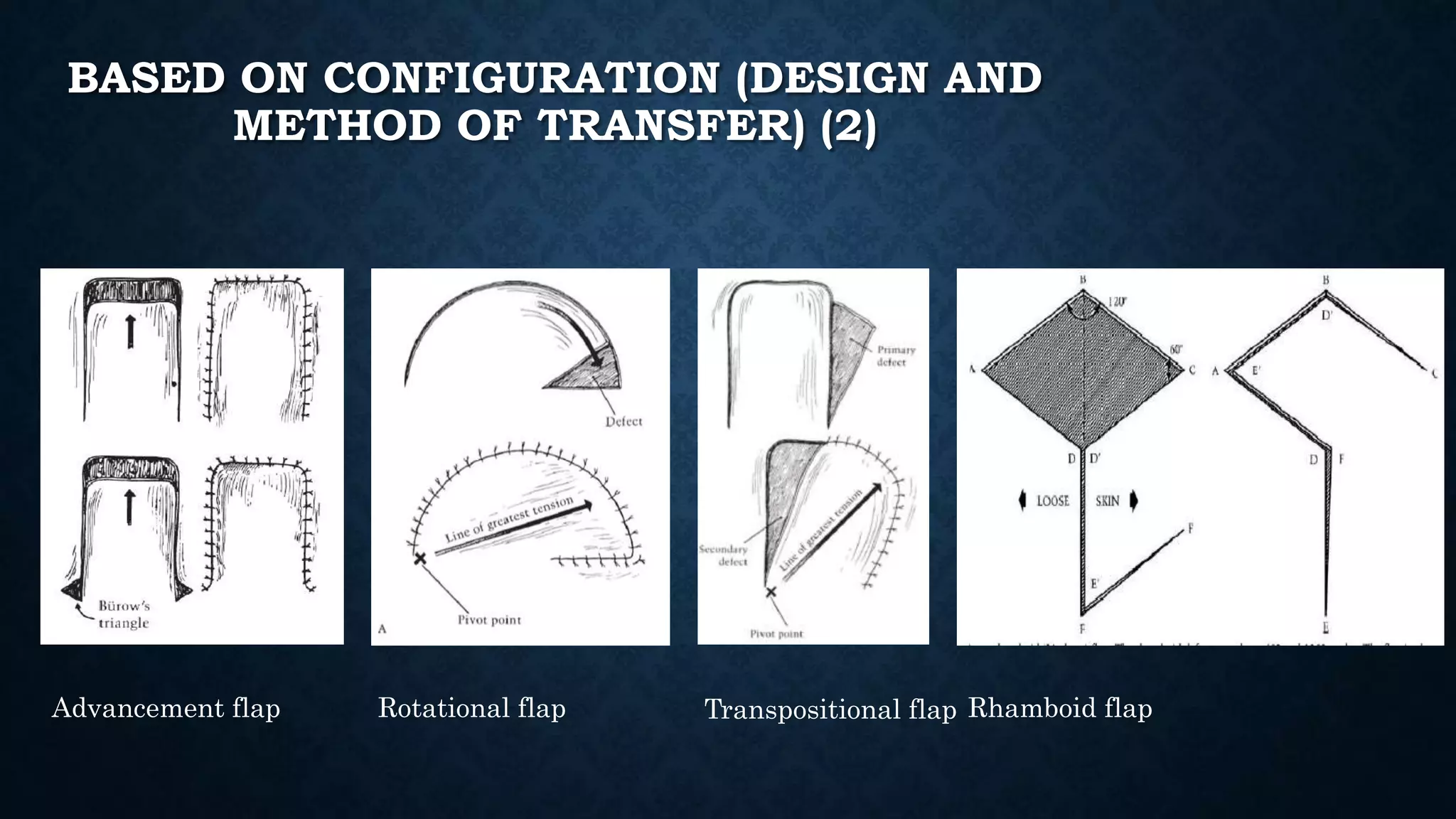
The document discusses skin grafts and flaps for reconstructive purposes. There are two main types of skin grafts - split thickness skin grafts (STSG) and full thickness skin grafts (FTSG). STSGs carry some risk of contraction and color change, while FTSGs have a lower risk but a smaller coverage area. Flaps differ in that they maintain their own blood supply from the donor site. Local flaps are the simplest type, while free flaps require microsurgery to reconnect blood vessels. The choice depends on factors like the wound site and desired tissue characteristics. Proper planning is essential for successful reconstruction with grafts or flaps.