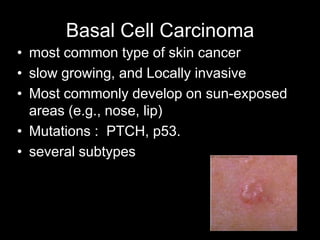
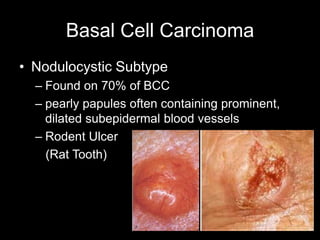
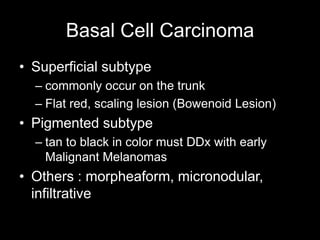
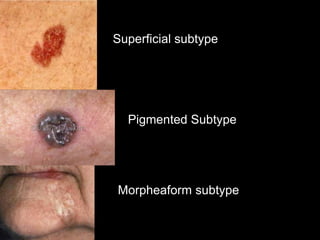
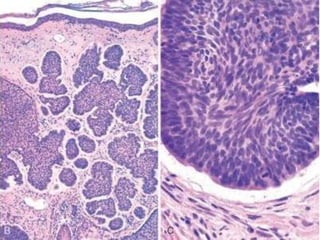
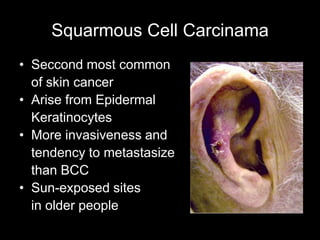
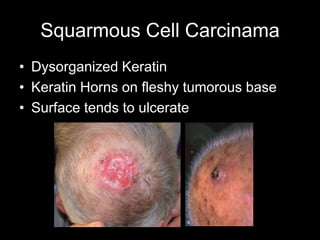
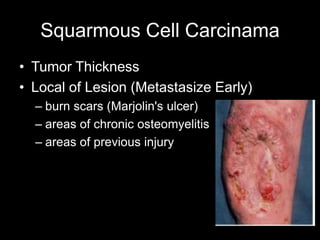
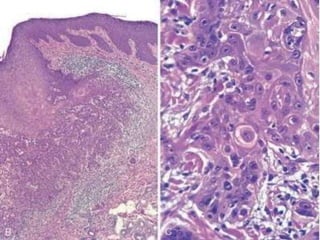
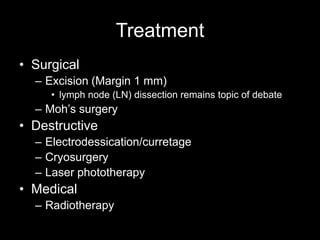
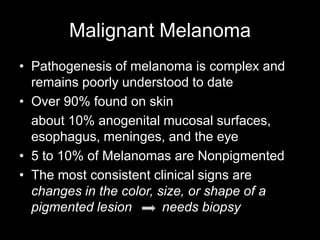
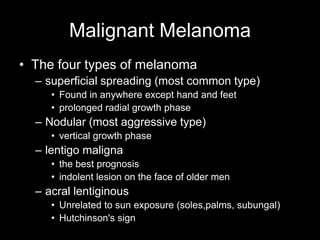
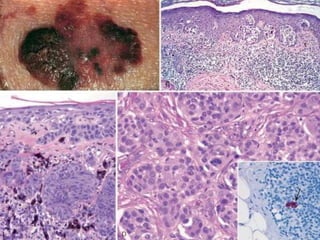
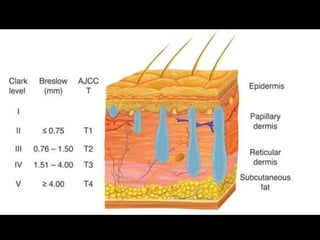
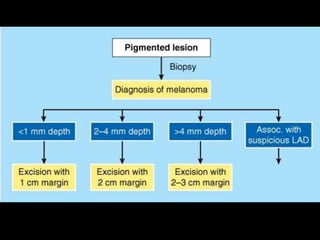
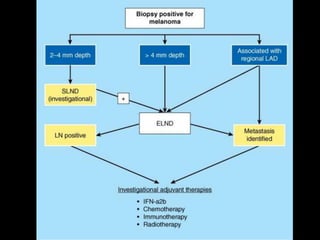
This document summarizes different types of skin cancer and their characteristics. It discusses the three main types: non-melanoma skin cancers like basal cell carcinoma and squamous cell carcinoma, and melanoma. Basal cell carcinoma is the most common type, usually appearing as nodular lesions on sun-exposed areas. Squamous cell carcinoma is also common and can metastasize. Melanoma subtypes include superficial spreading, nodular, lentigo maligna, and acral lentiginous. Prevention strategies focus on reducing sun exposure and applying sunscreen. Surgical excision is a common treatment, along with Mohs surgery, radiation, and medical therapies.