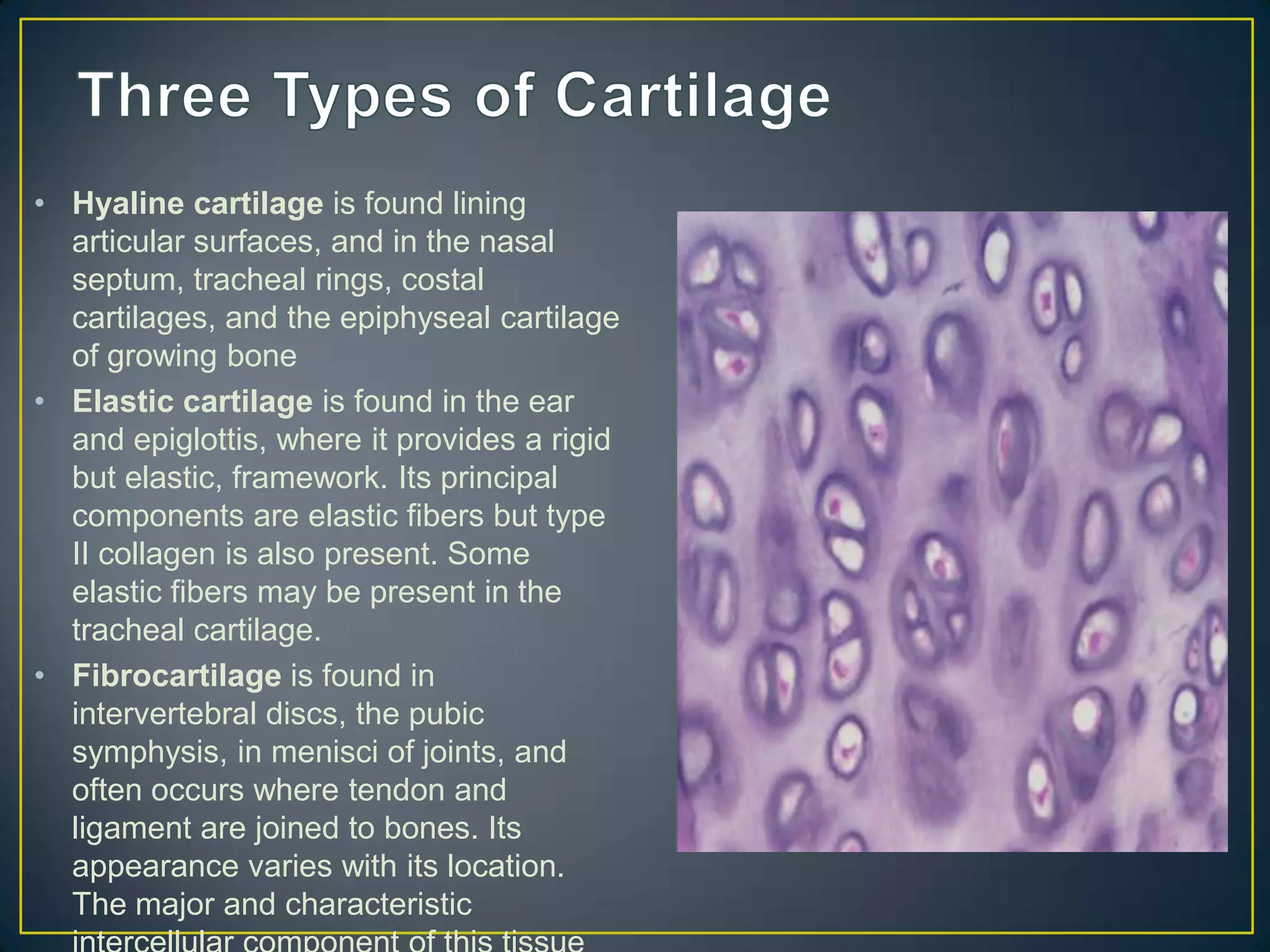
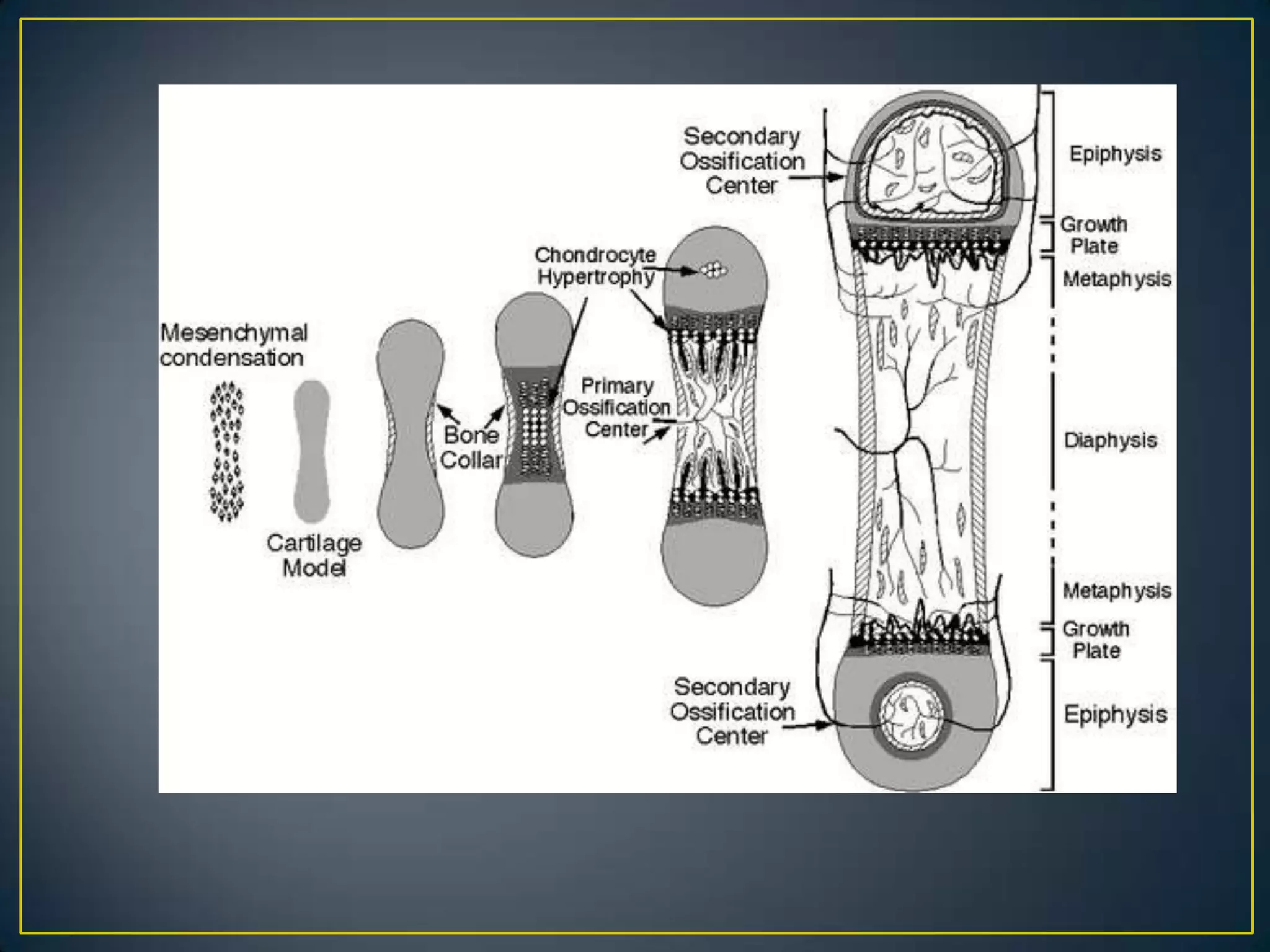
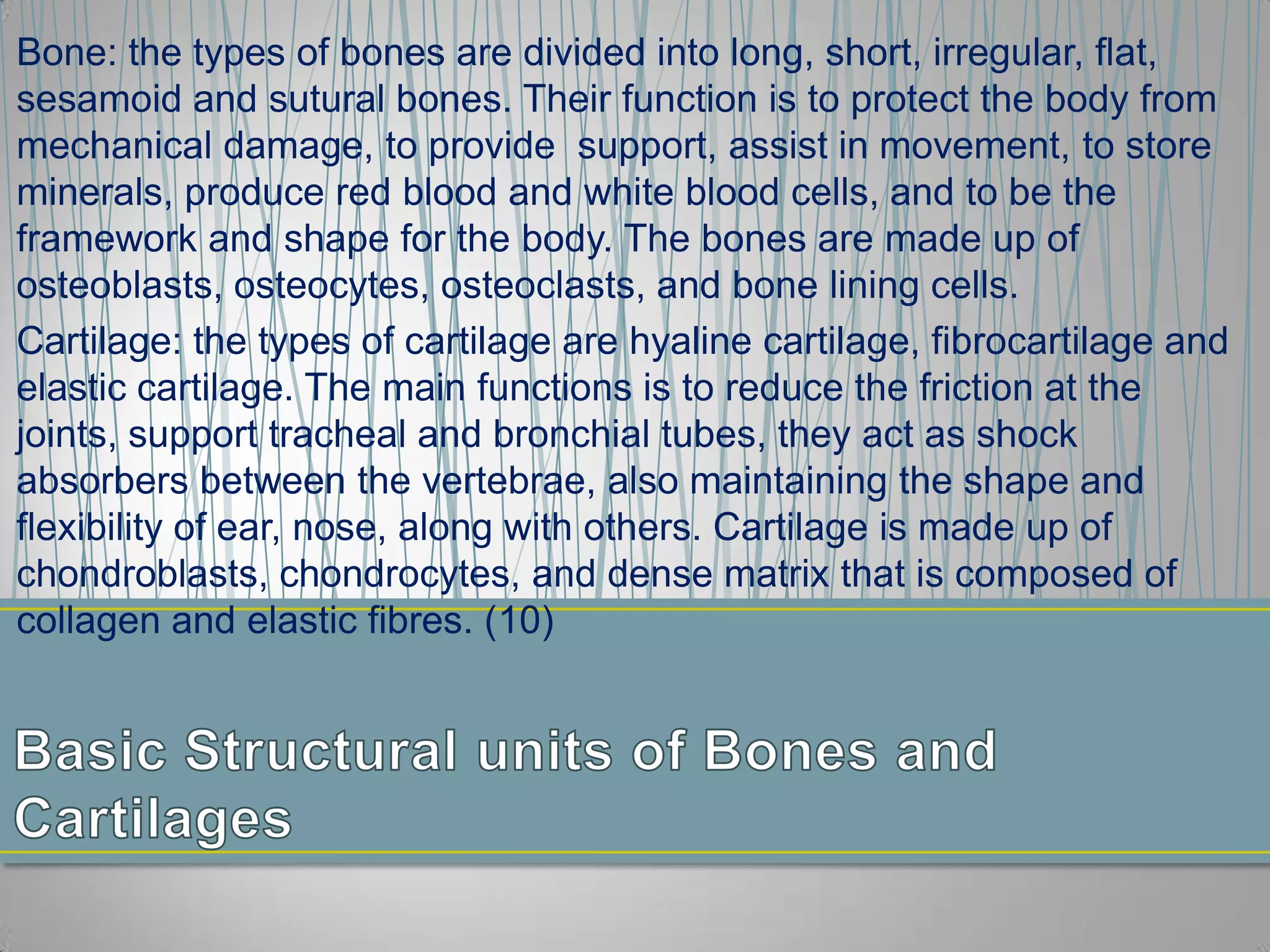
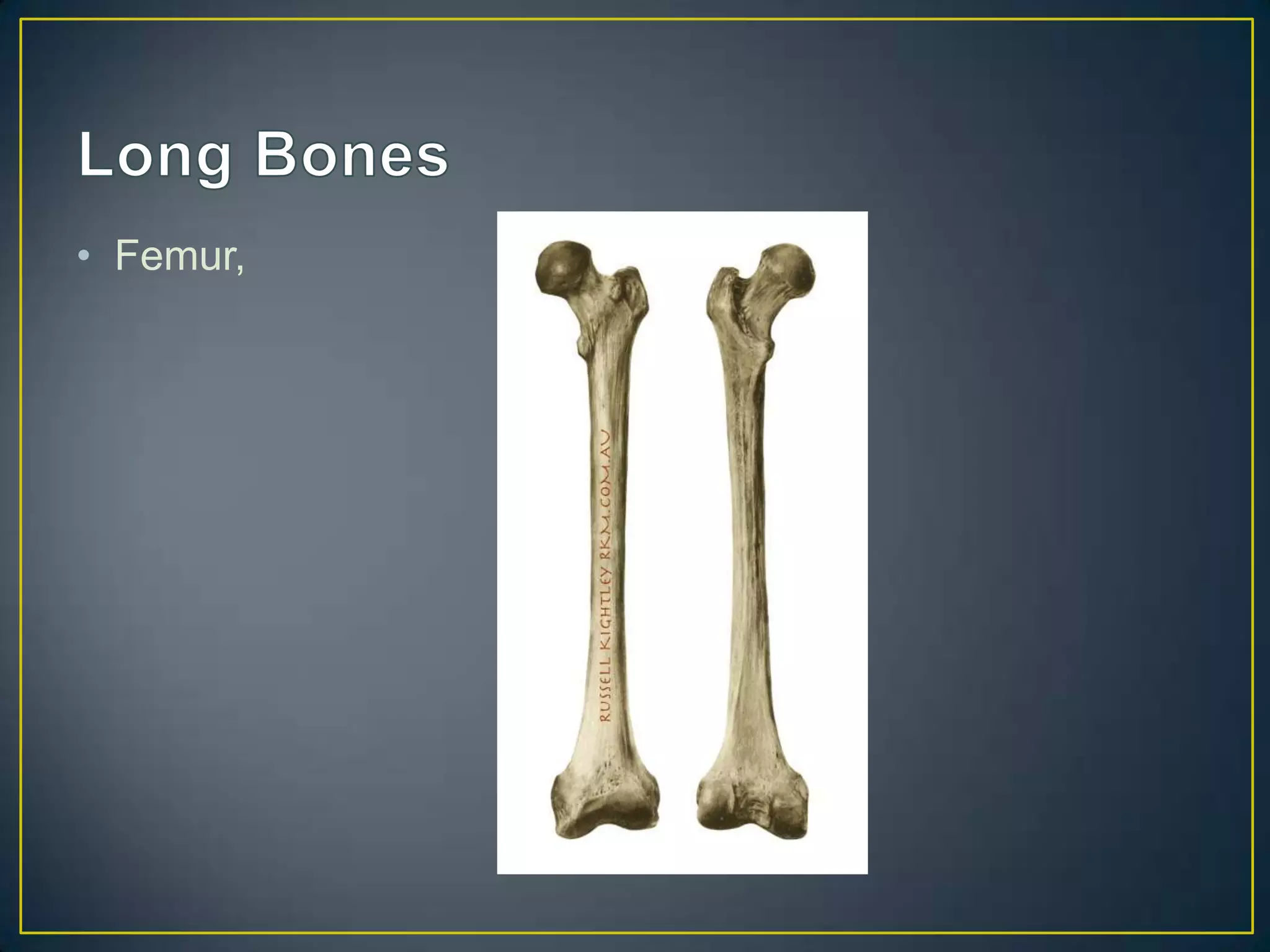
Cartilage is a specialized connective tissue containing cells called chondrocytes that secrete an extracellular matrix. There are three main types of cartilage - hyaline, elastic, and fibrocartilage - each with different compositions and locations in the body. Growth plate fractures often result from sprains and strains in growing children and involve the growth plates located at the ends of long bones.