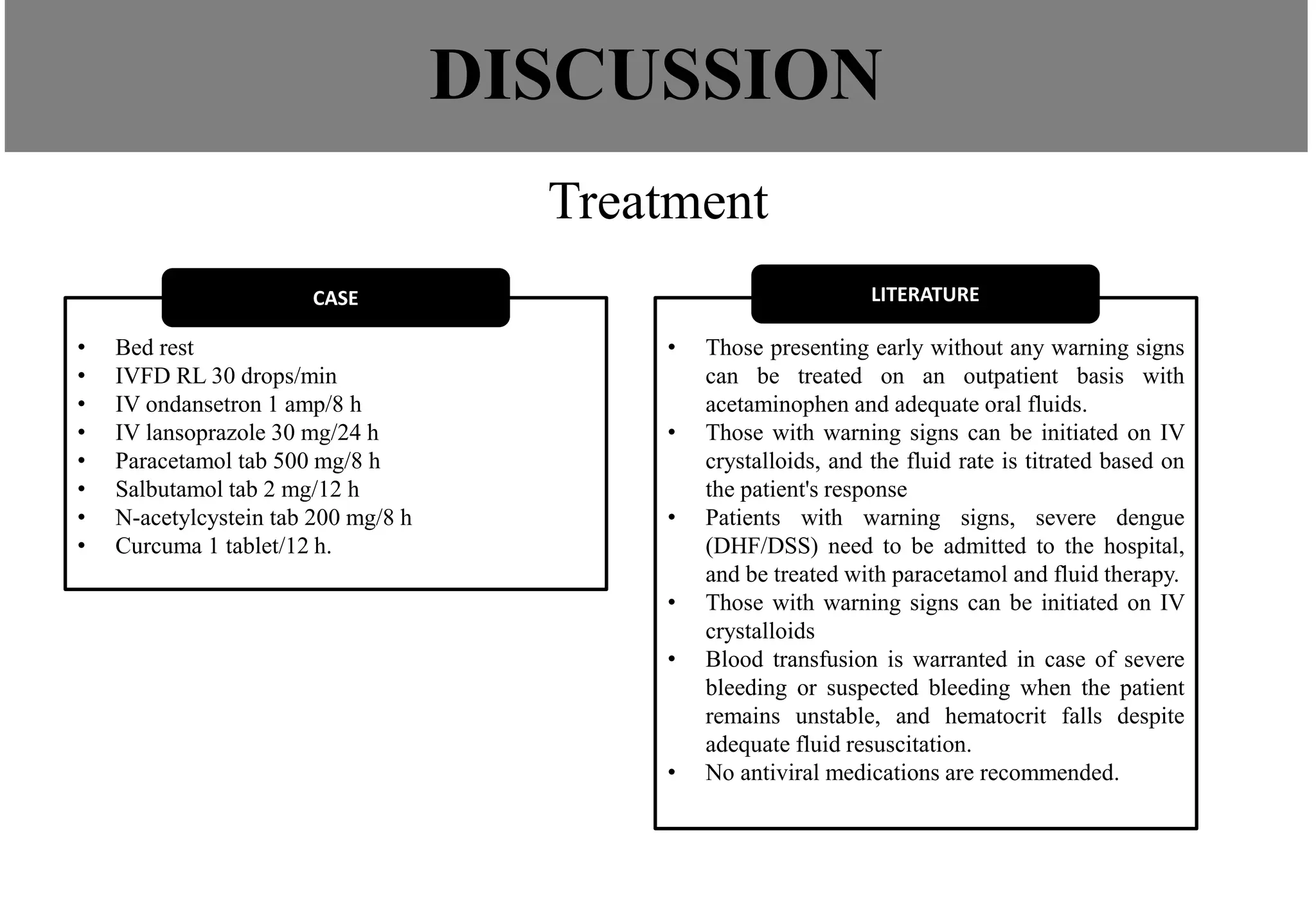
This case report describes a 37-year-old man diagnosed with Grade II dengue hemorrhagic fever who presented with sinus bradycardia. Laboratory tests confirmed dengue infection and showed thrombocytopenia and elevated liver enzymes. Chest X-ray found left pleural effusion. The patient was treated conservatively with IV fluids, antiemetics, and analgesics. Dengue virus can cause myocardial inflammation and arrhythmias like bradycardia through direct viral invasion or immune mediated mechanisms. This case emphasizes that bradycardia is a common finding in dengue that results from the cardiac effects of the viral infection.