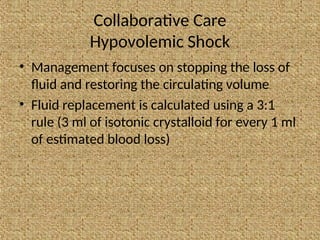
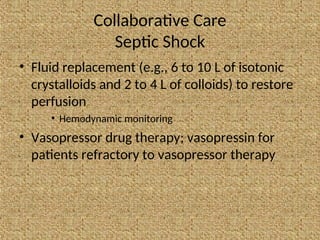
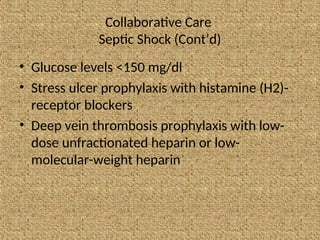
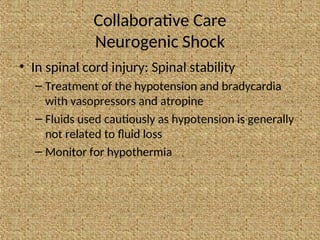
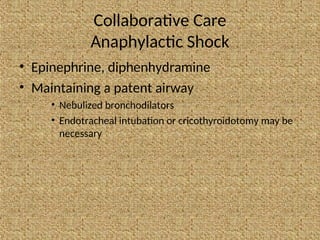
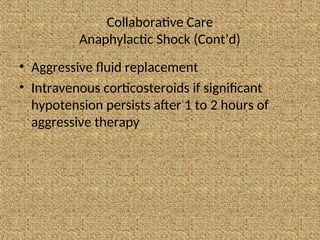
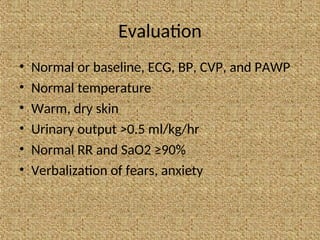
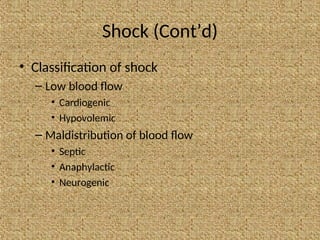
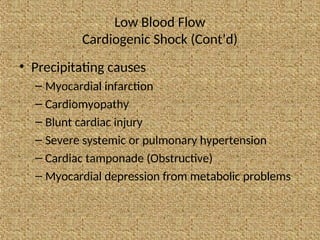
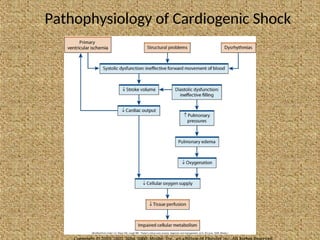
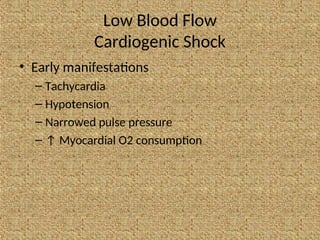
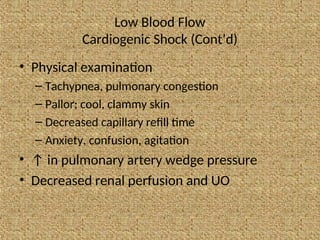
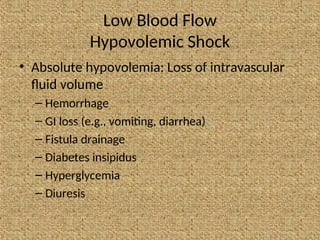
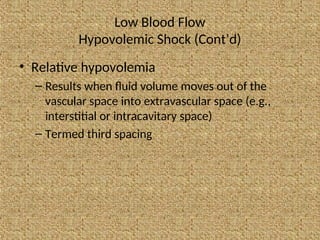
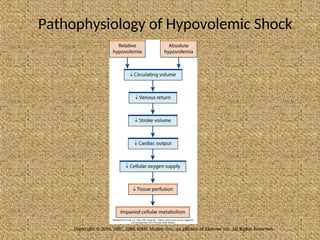
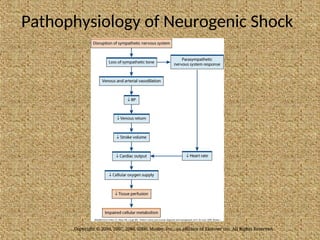
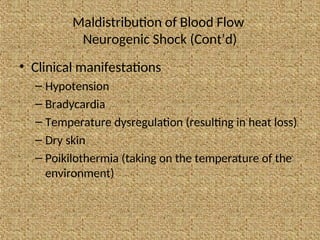
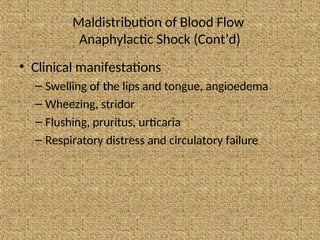
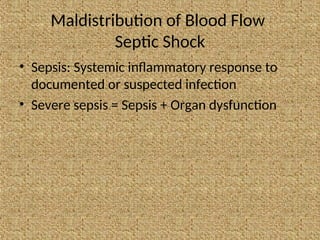
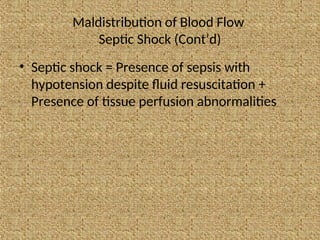
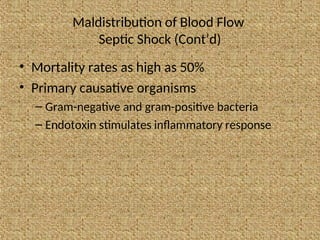
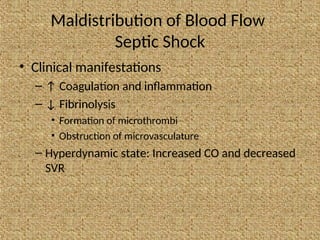
The document presents a comprehensive overview of shock management, detailing various types of shock including cardiogenic, hypovolemic, neurogenic, anaphylactic, and septic shock, along with their causes, clinical manifestations, and treatment strategies. It emphasizes the importance of early identification and intervention to prevent organ dysfunction and complications, including fluid resuscitation and pharmacologic therapy. Key nursing assessments and collaborative care approaches are discussed to ensure adequate tissue perfusion and patient recovery.
![Collaborative Care (Cont’d)
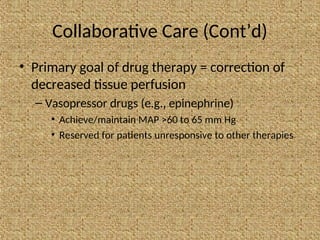
• Primary goal of drug therapy = correction of
decreased tissue perfusion
– Vasodilator therapy (e.g., nitroglycerin
[cardiogenic shock], nitroprusside [noncardiogenic
shock])
• Achieve/maintain MAP >60 to 65 mm Hg](https://image.slidesharecdn.com/shockpresentation-240806062754-b5ed903a/85/Shock-Presentation-Definition-etiology-types-and-management-52-320.jpg)