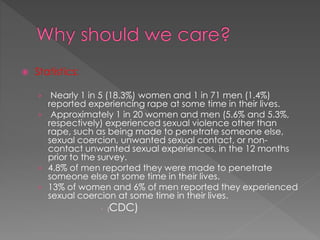
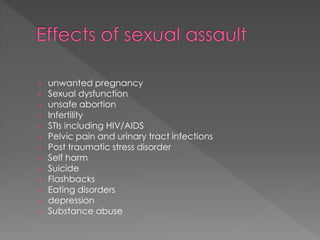
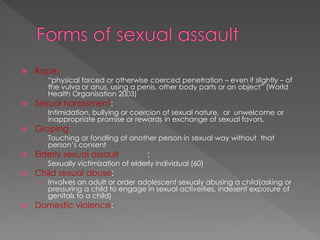
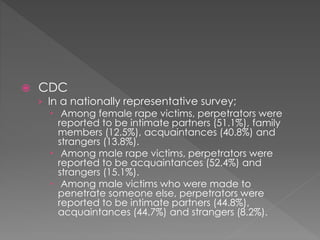
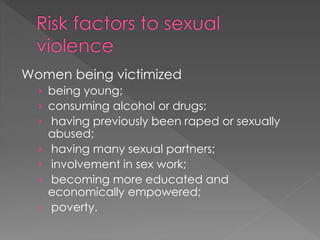
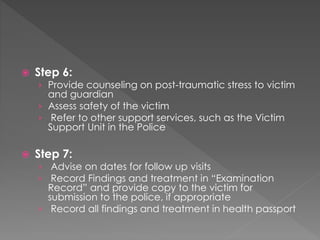
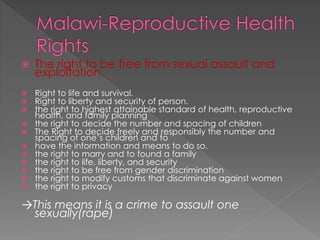
The document discusses sexual assault, including definitions, statistics, forms of assault, risk factors, and protocols for managing assault in Malawi. It provides background on sexual assault and its health effects. It then outlines forms of assault like rape, harassment, and child abuse. Risk factors for victims and perpetrators are identified. The management protocol describes examining victims, investigations, treatments, counseling, and referrals to support services.