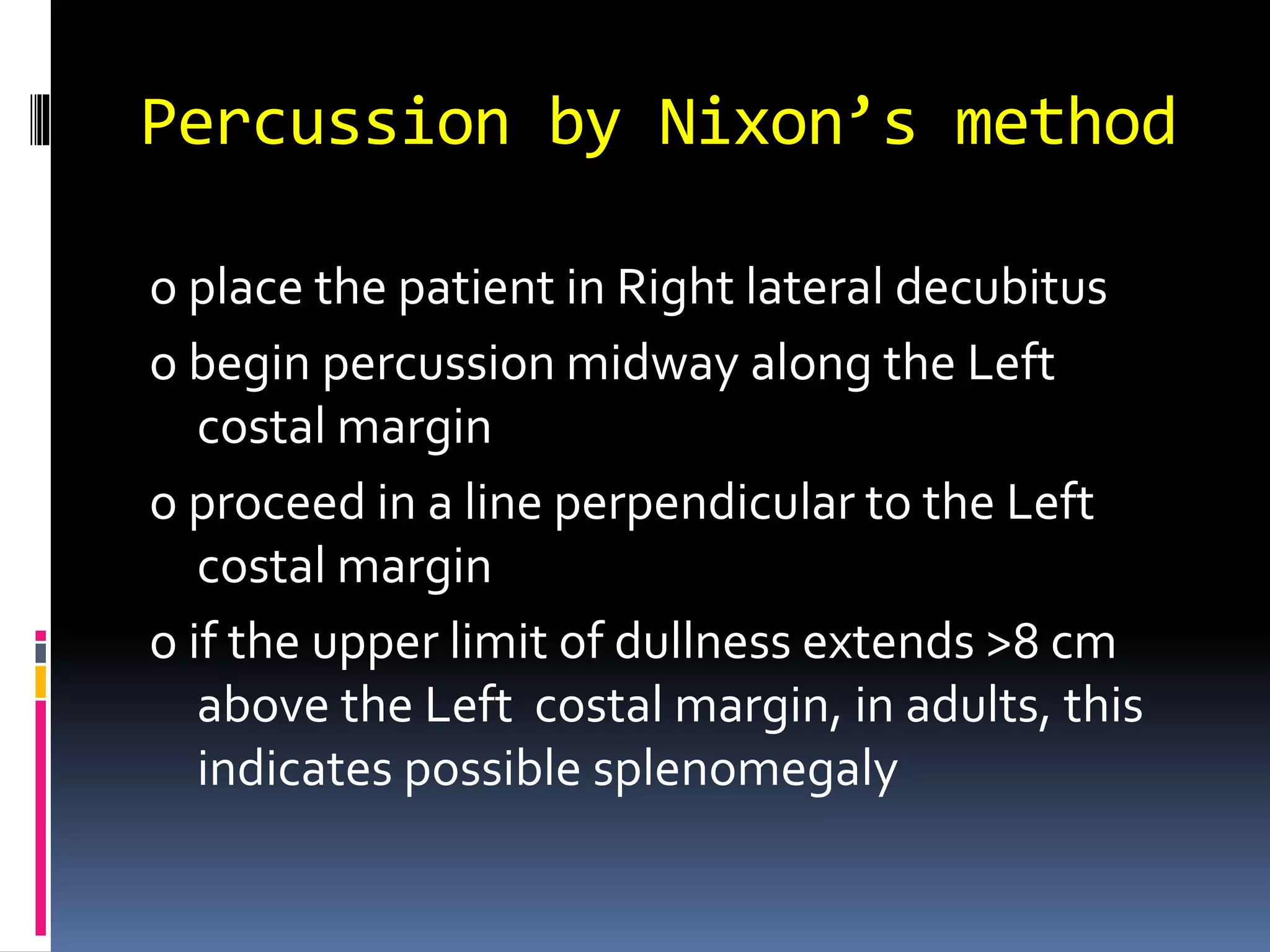
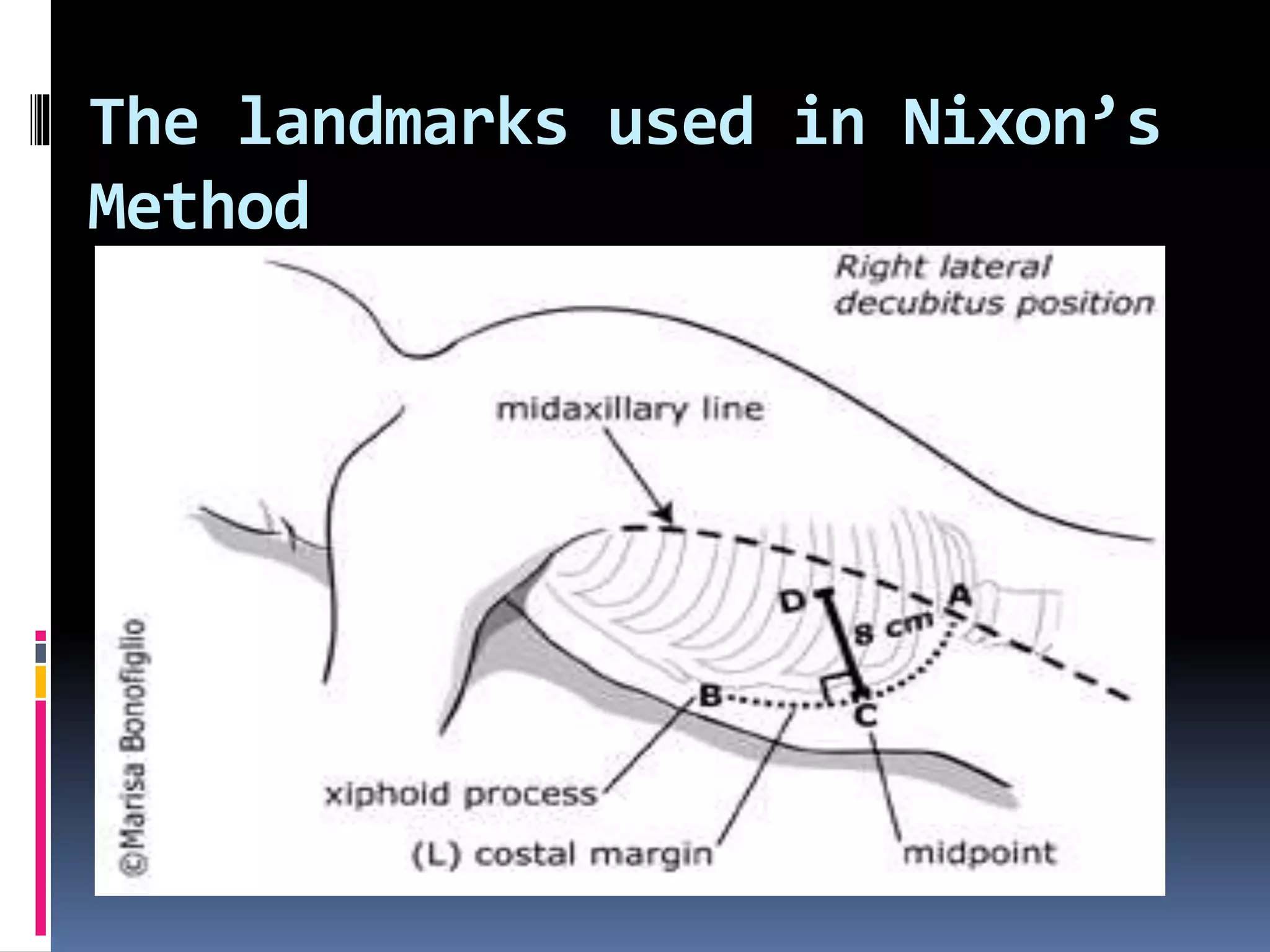
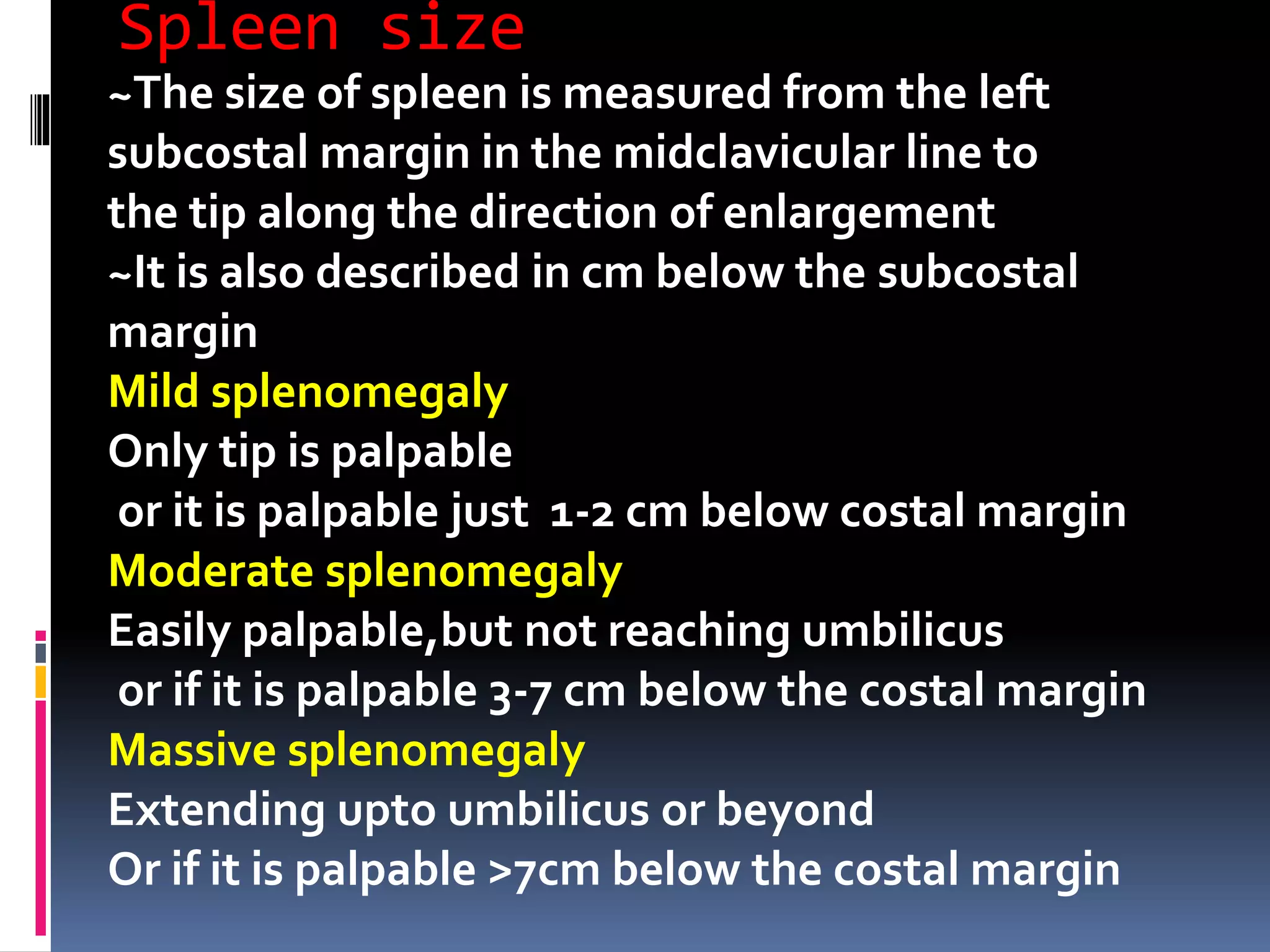
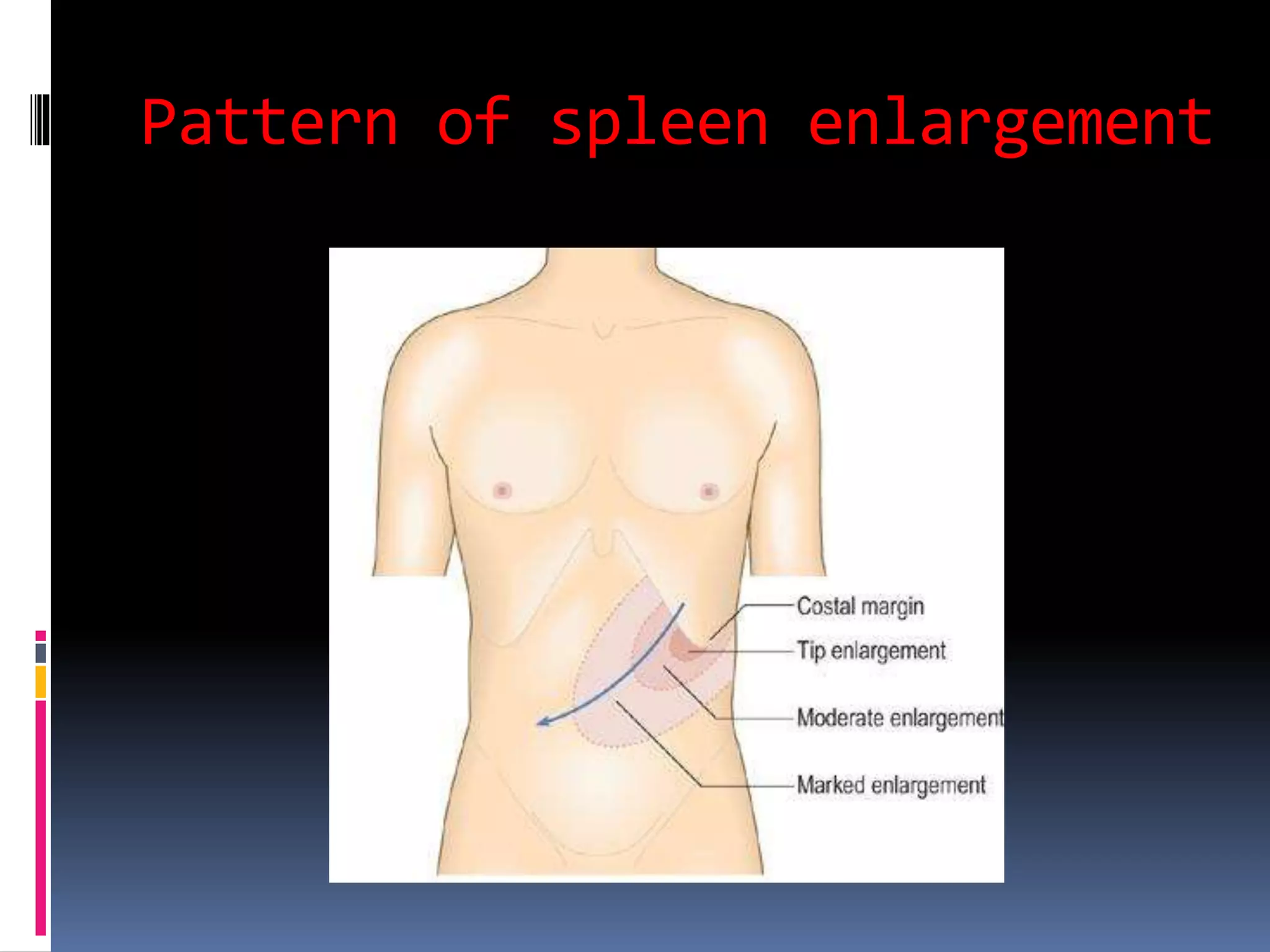
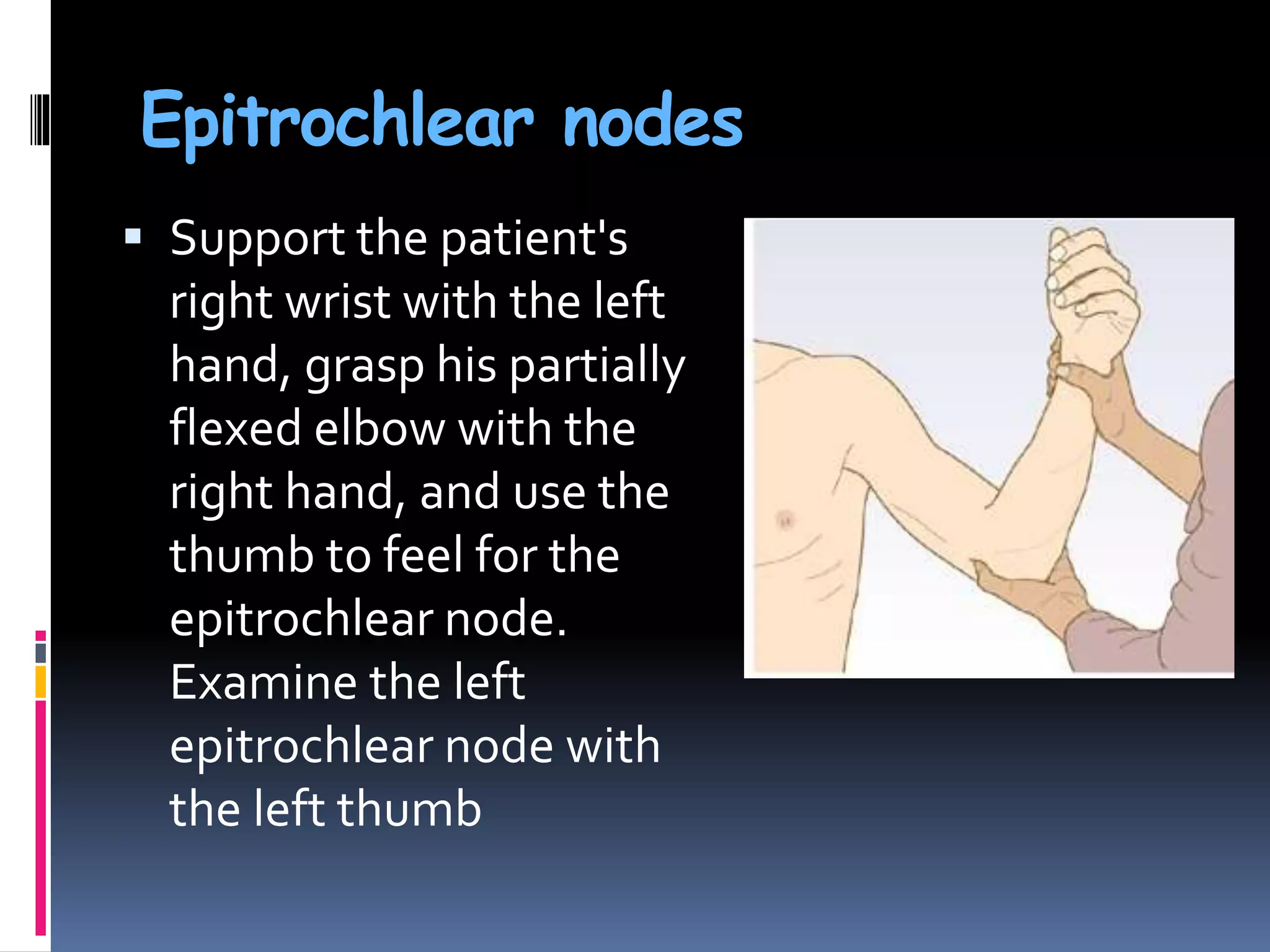
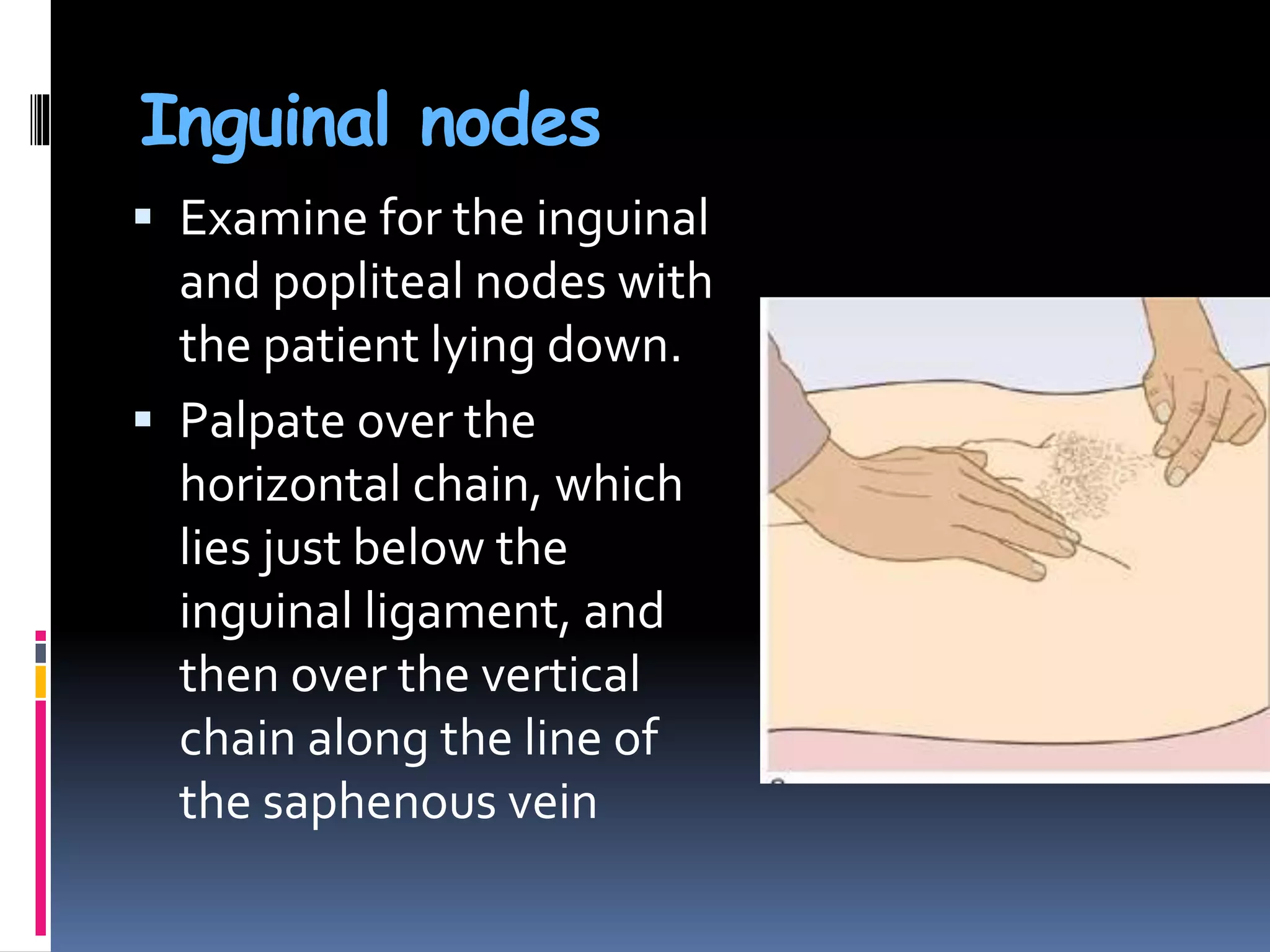
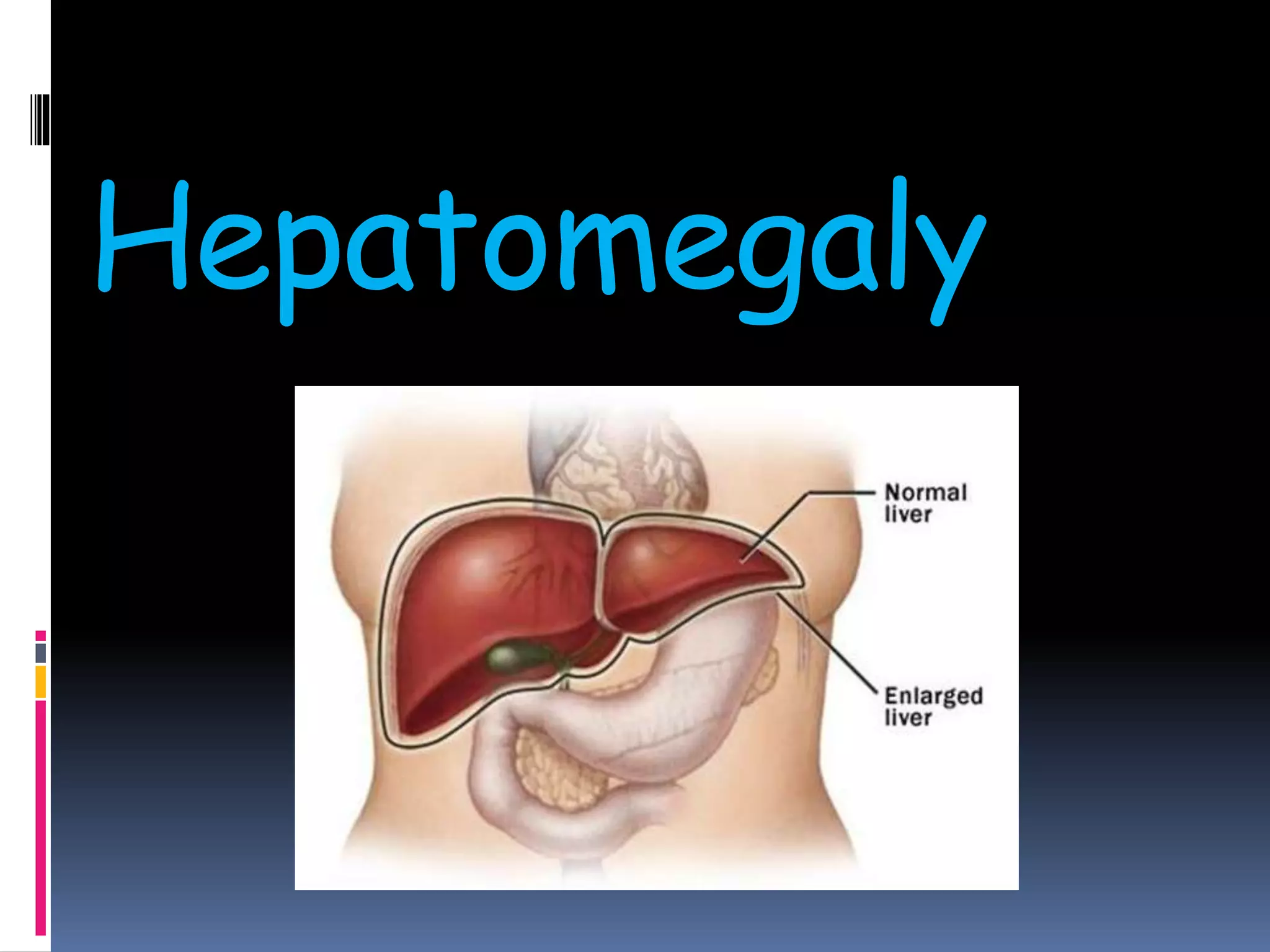
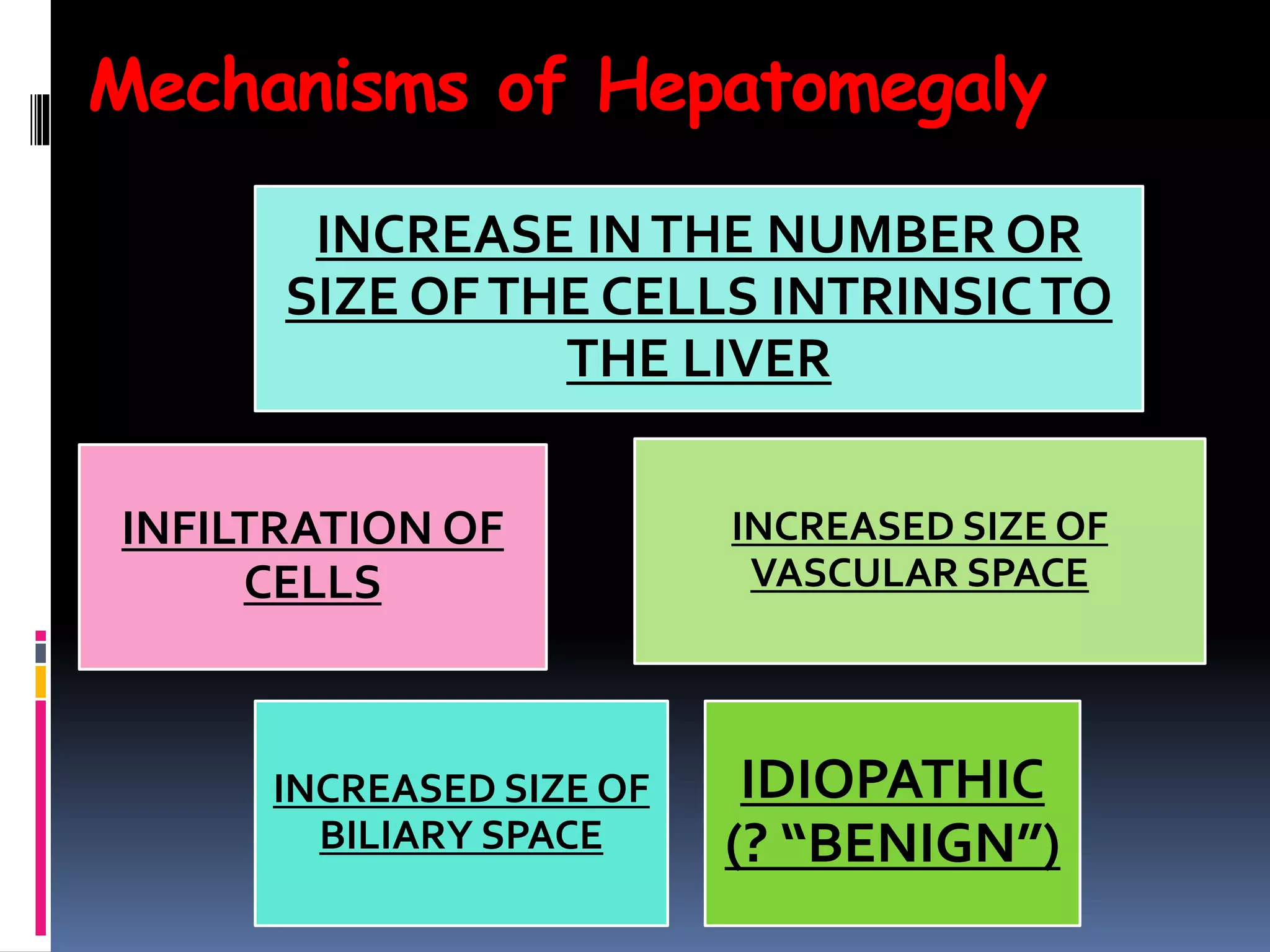
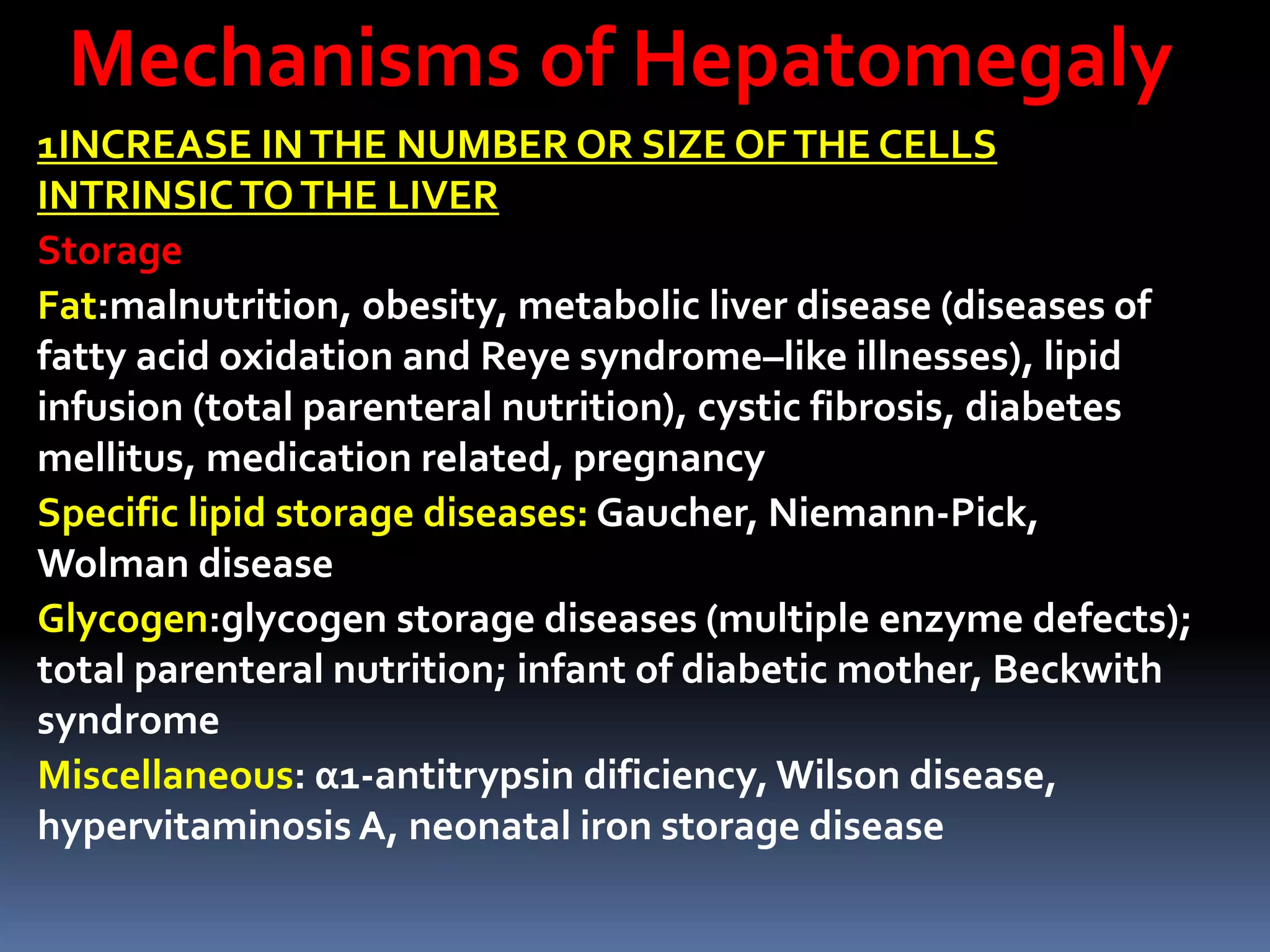
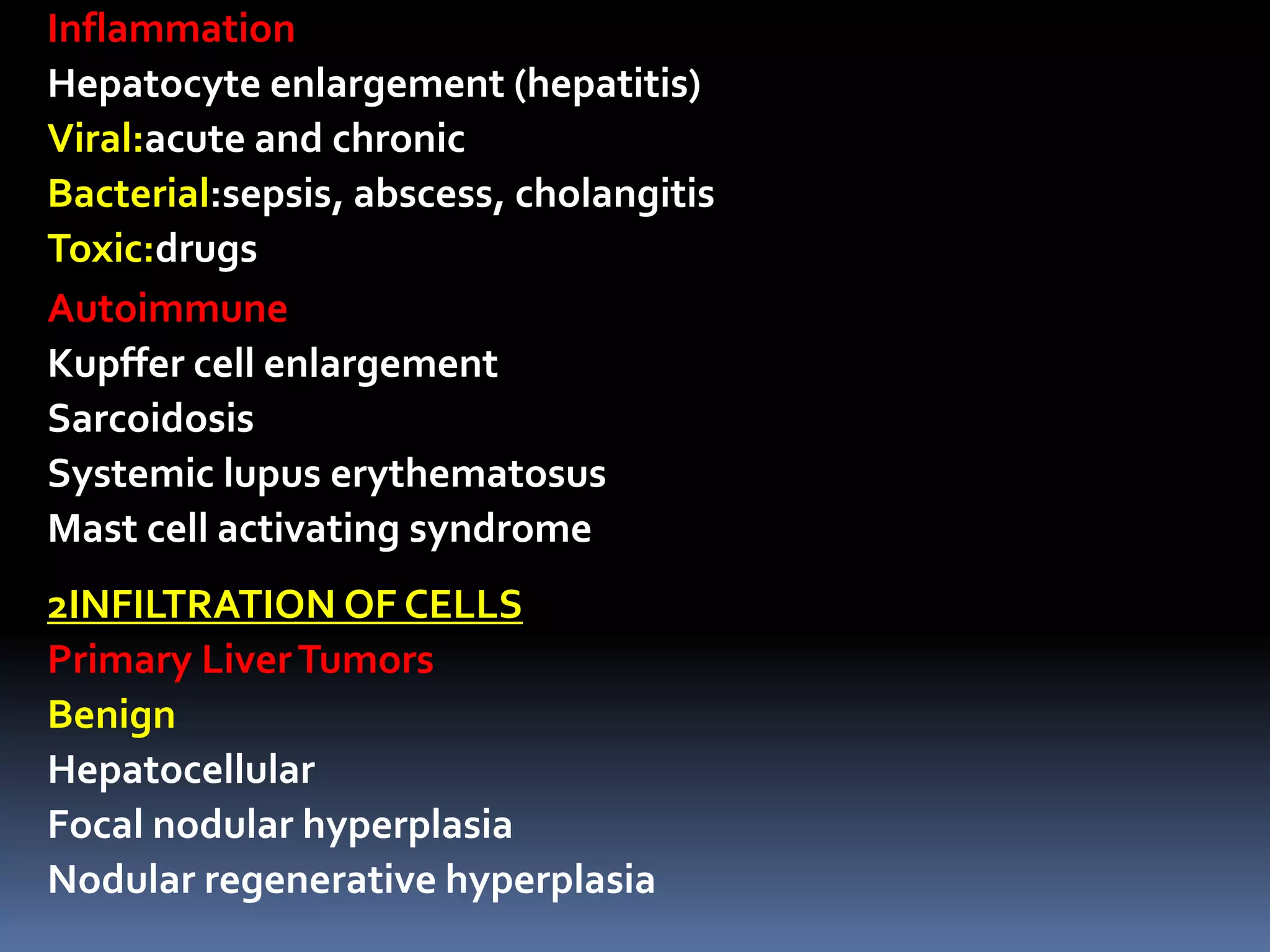
This document provides information on signs of abnormal liver and spleen, as well as mechanisms and causes of hepatomegaly, splenomegaly, and hepatosplenomegaly. It describes how the liver and spleen should feel on examination and lists various conditions that can lead to enlargement. These include increased cell size/number from storage diseases, inflammation, infiltrating cells from tumors or infections, increased vascular/biliary spaces from congestion, and idiopathic causes. Specific infectious, oncologic, metabolic, and hematologic etiologies are outlined.
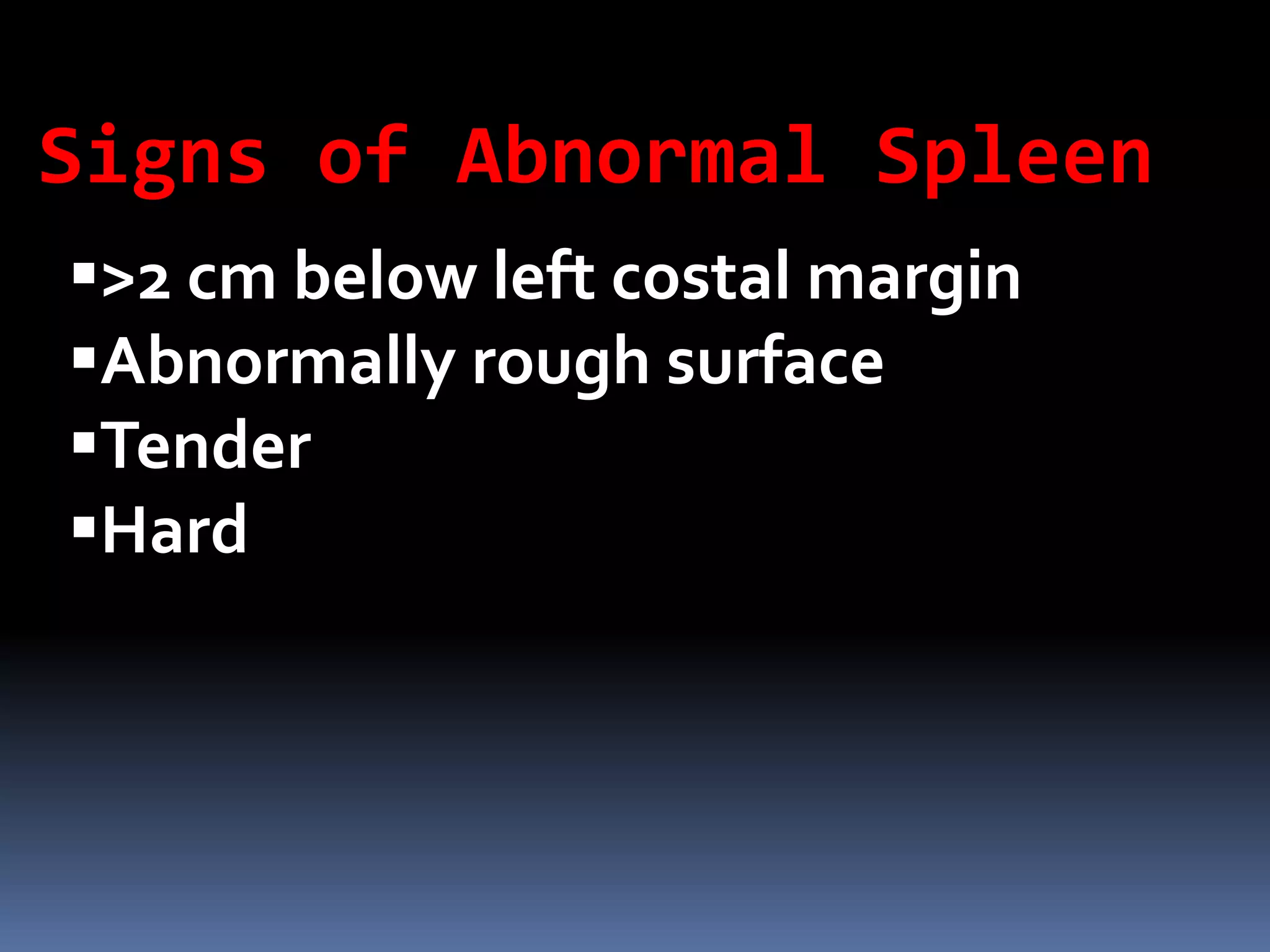
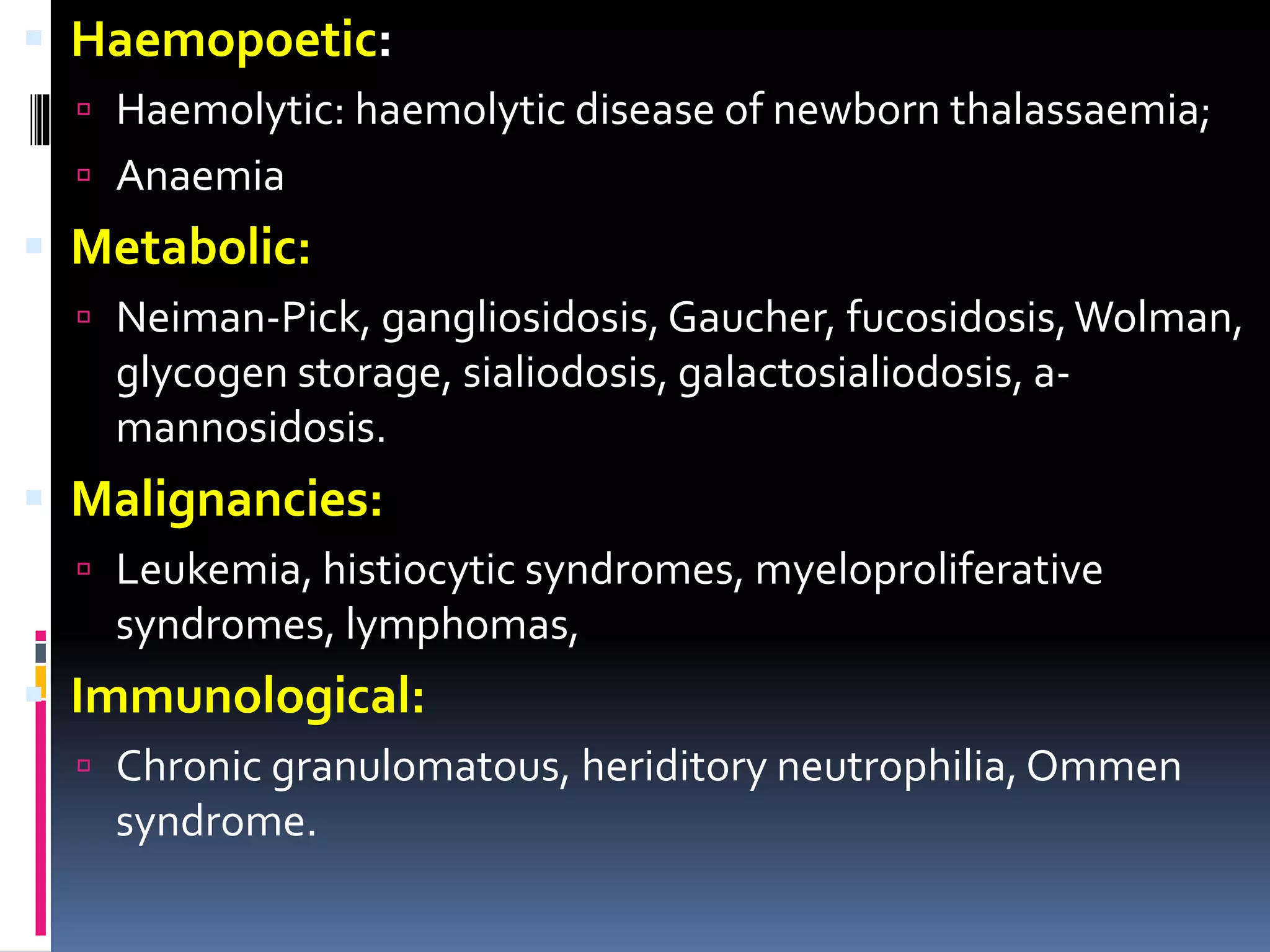
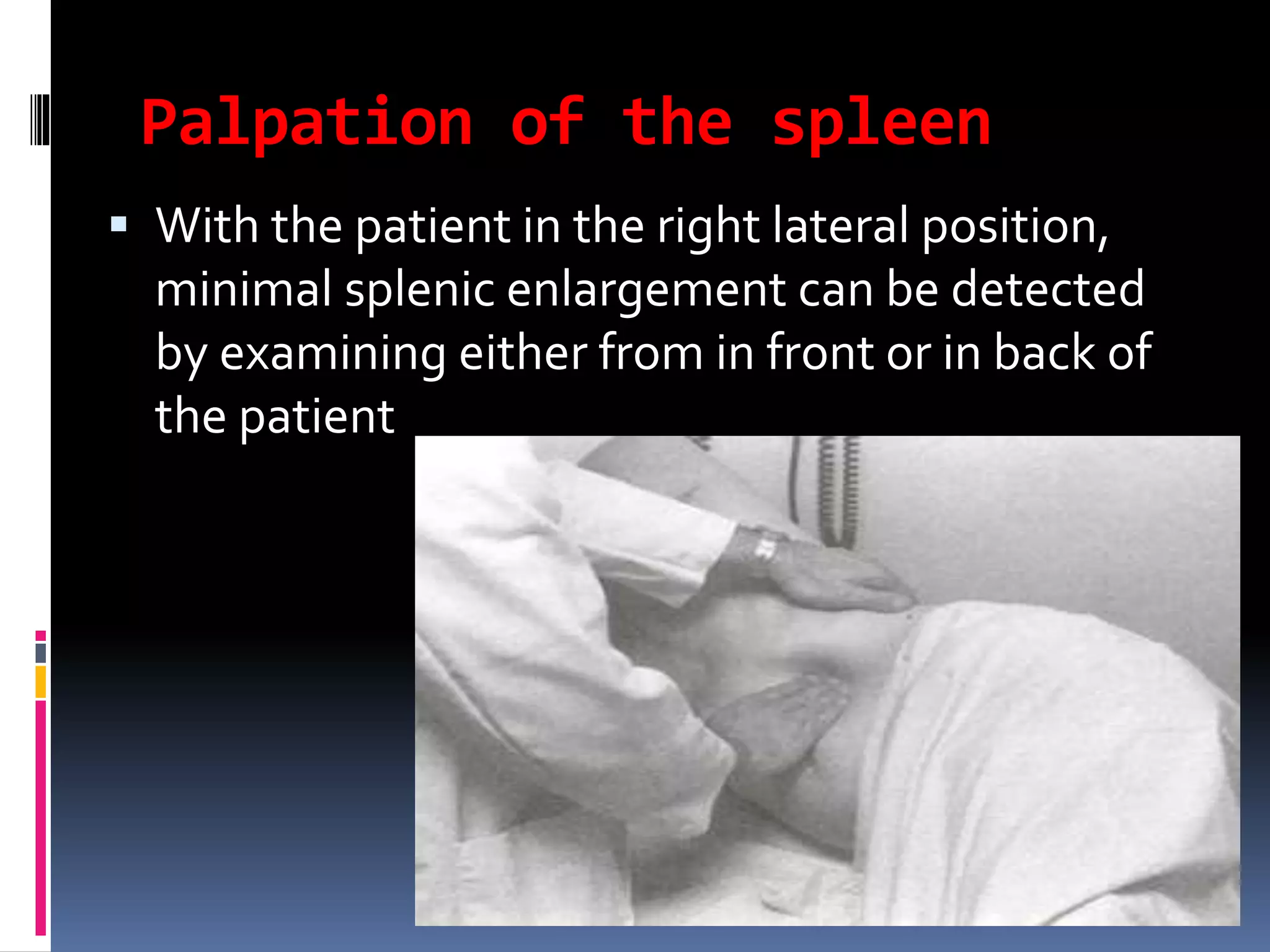
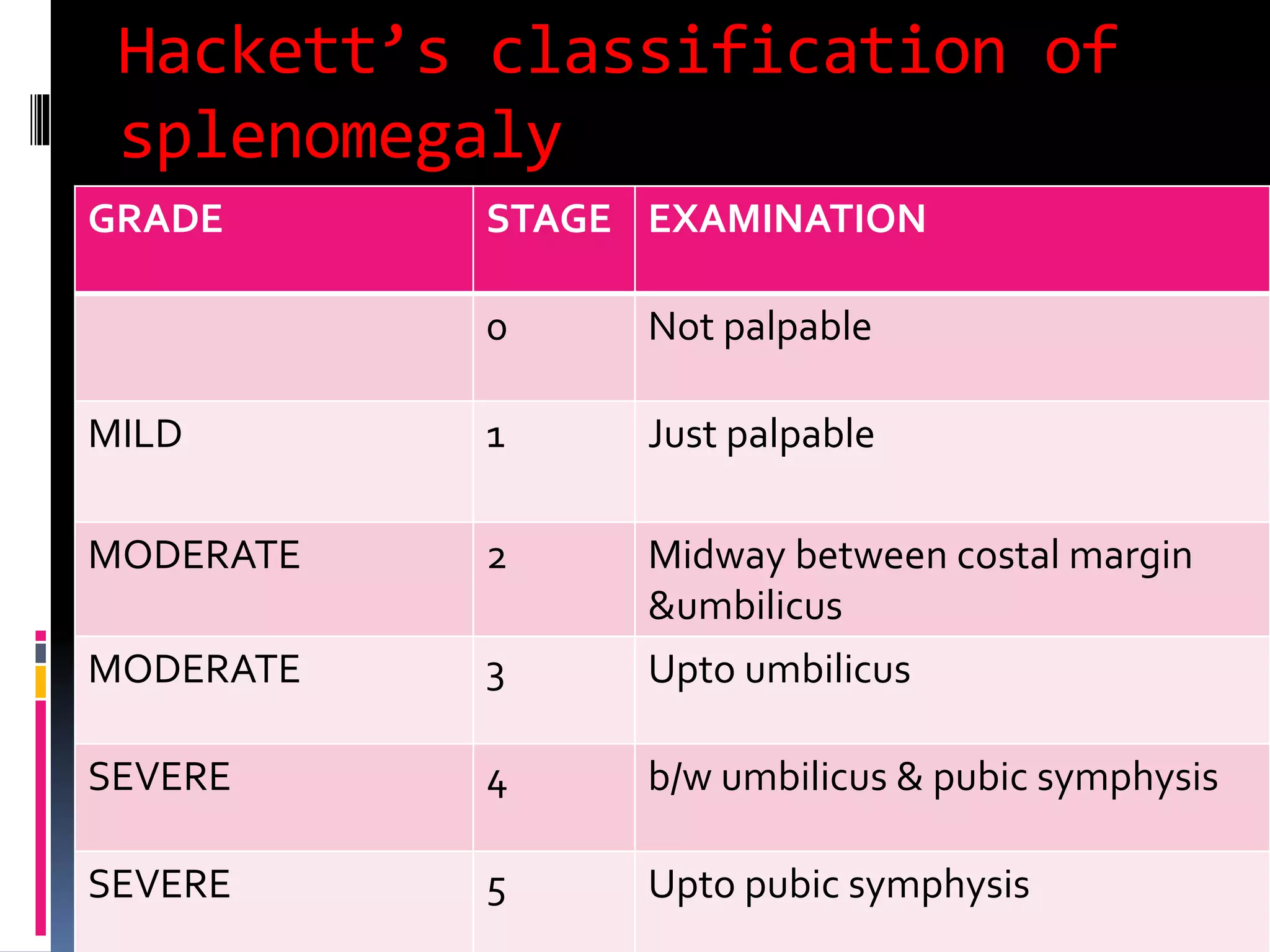
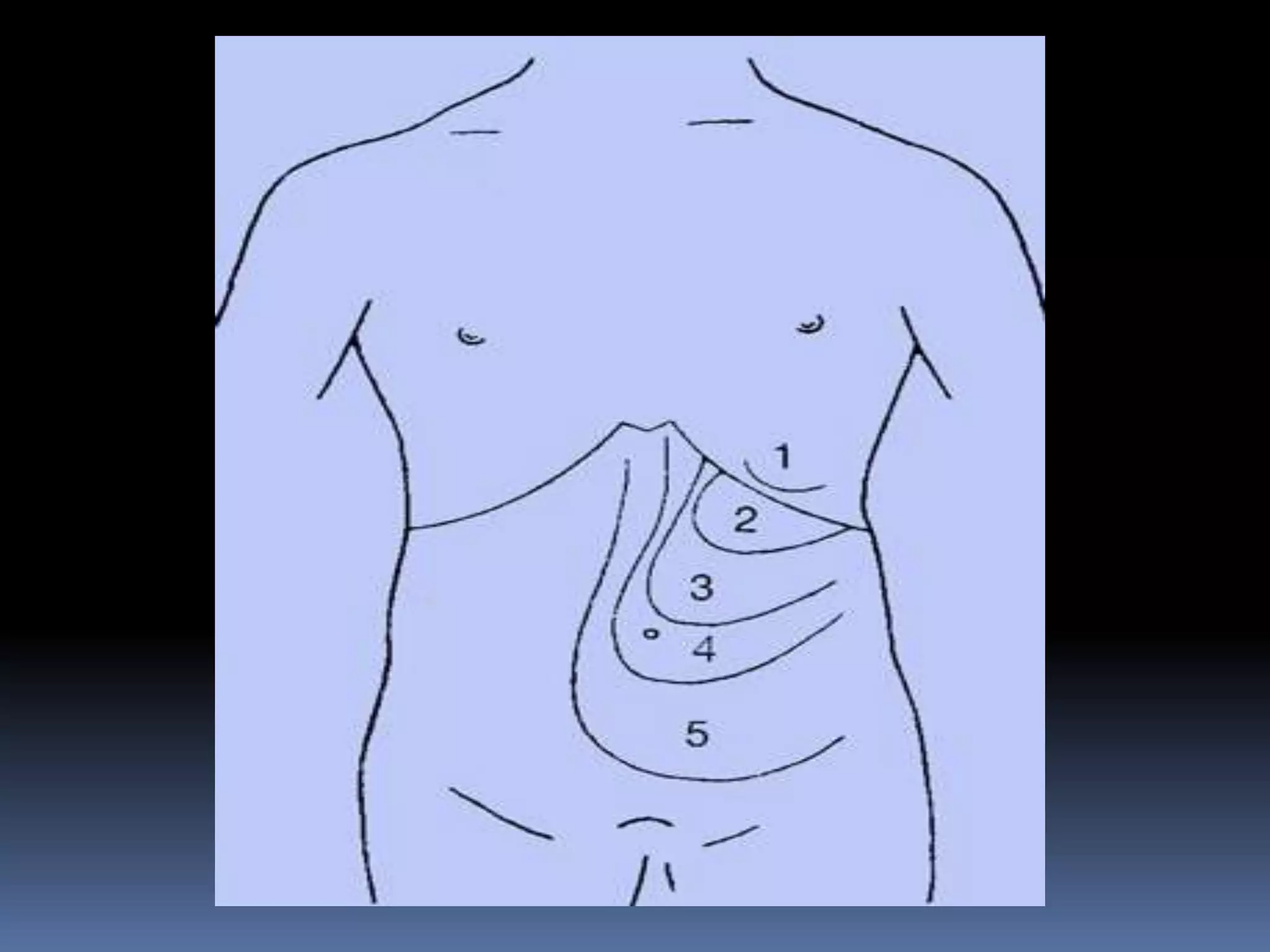
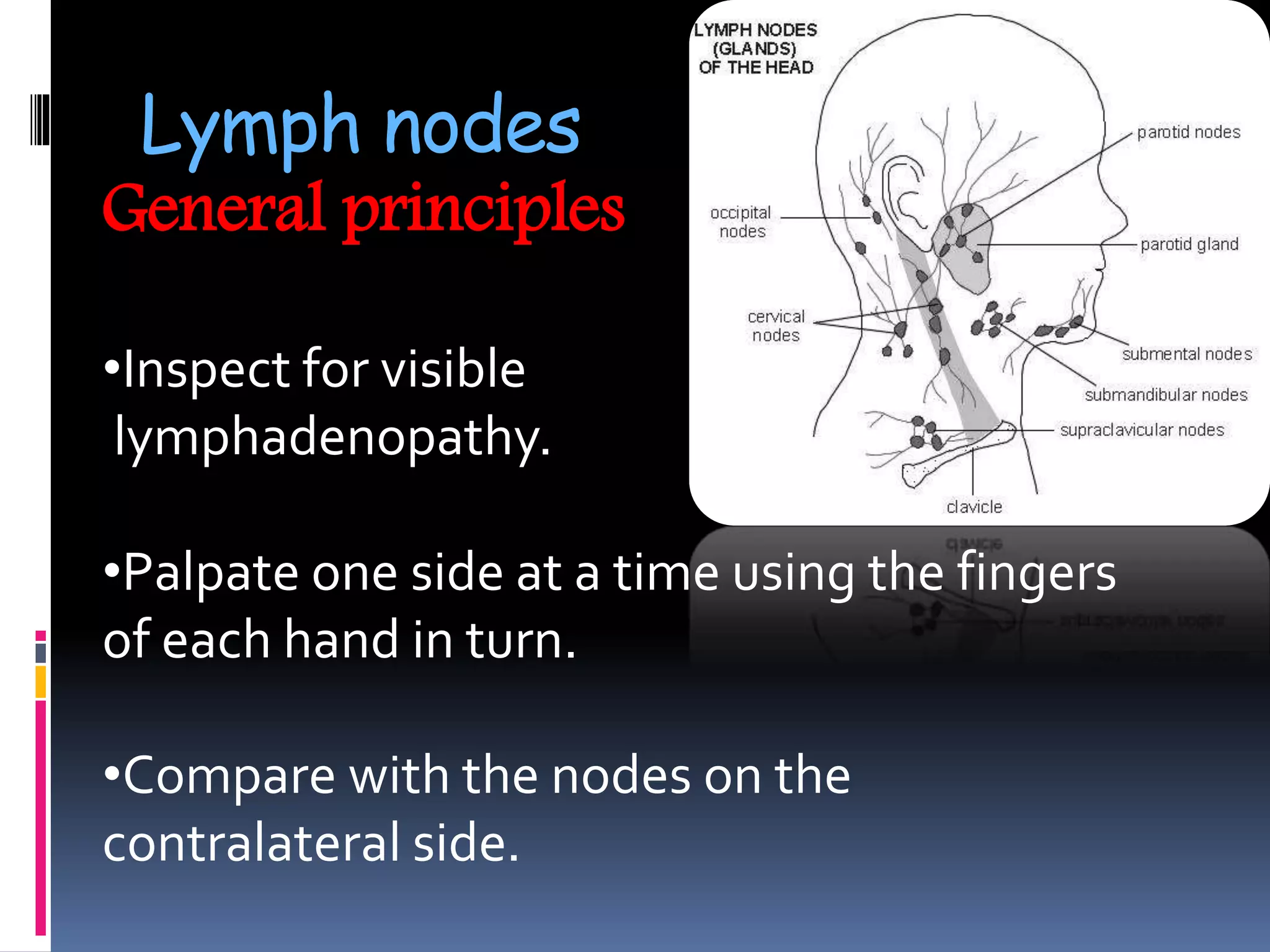
![Pathophysiology of splenomegaly
ANATOMIC
LESIONS
HYPERPLASIA
CAUSED BY
HEMATOLOGIC
DISORDERS
INFECTIONS[†]
IMMUNOLOGIC
AND
INFLAMMATORY
PROCESSES[*]
CONGESTIVE[*] STORAGE
DISEASES
MALIGNANCIES](https://image.slidesharecdn.com/anapproachtoachildwithhepatosplenomegalyandlymphadenopathy-180818120204/75/An-approach-to-a-child-with-hepatosplenomegaly-and-lymphadenopathy-15-2048.jpg)
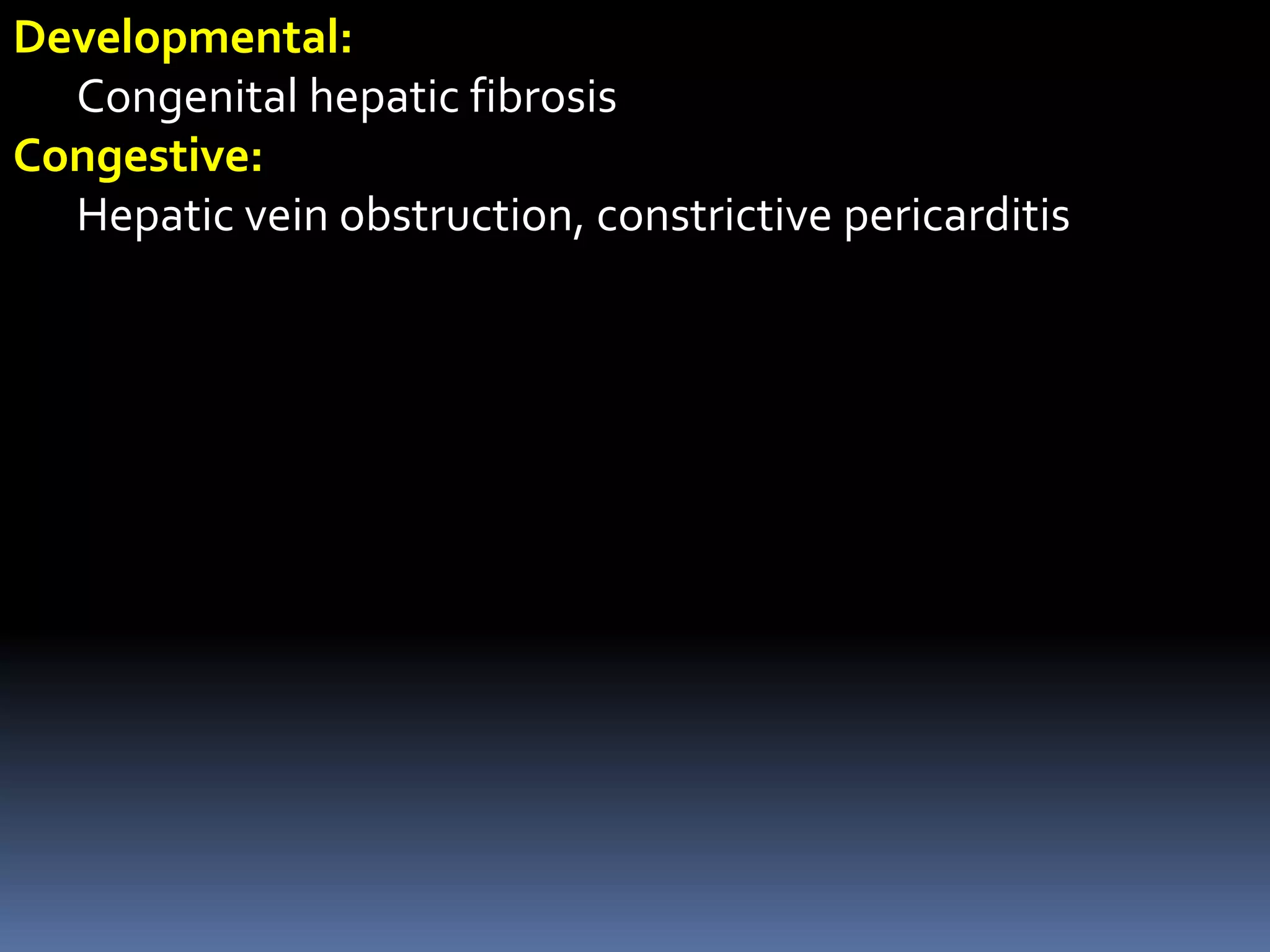
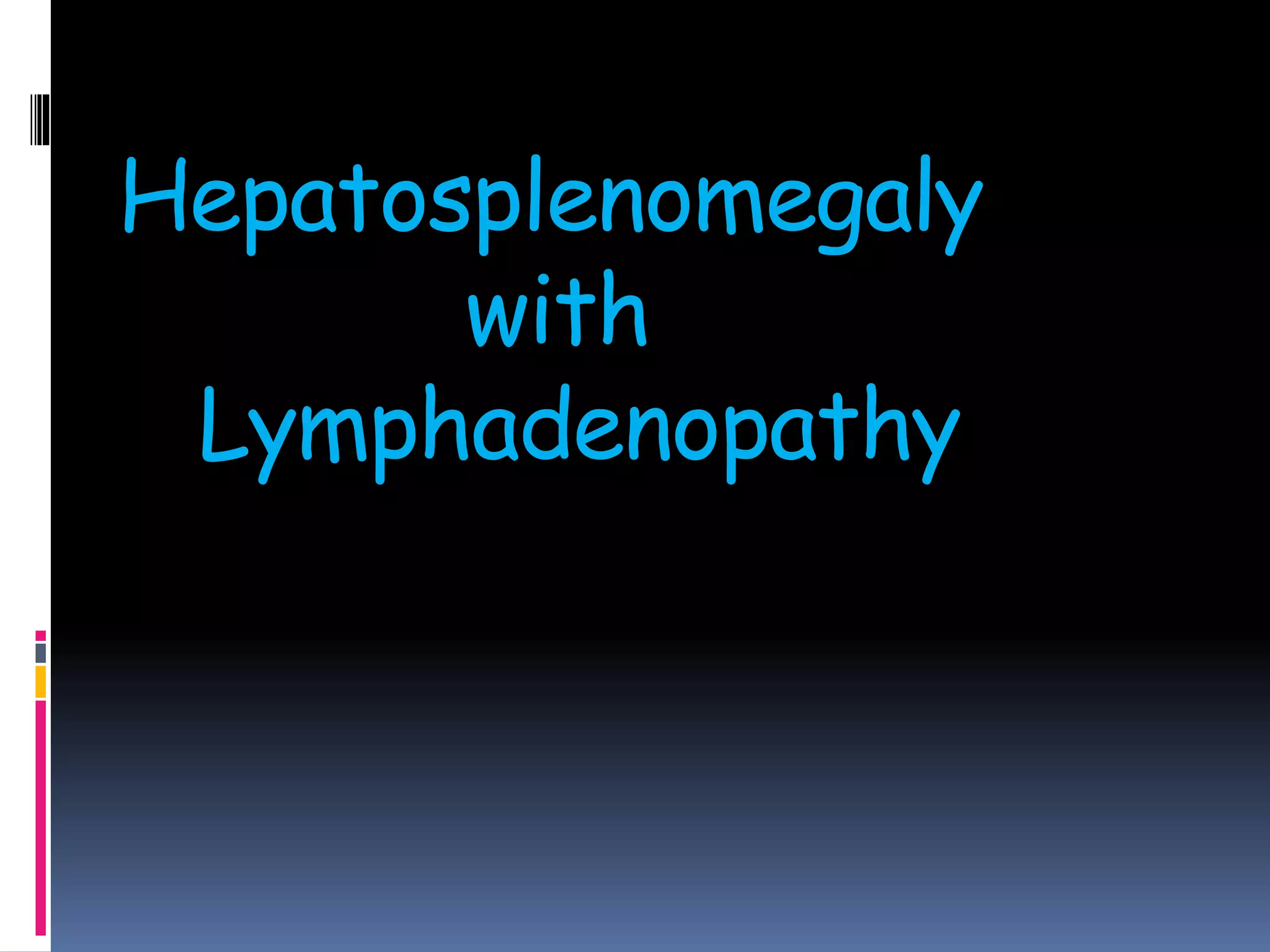
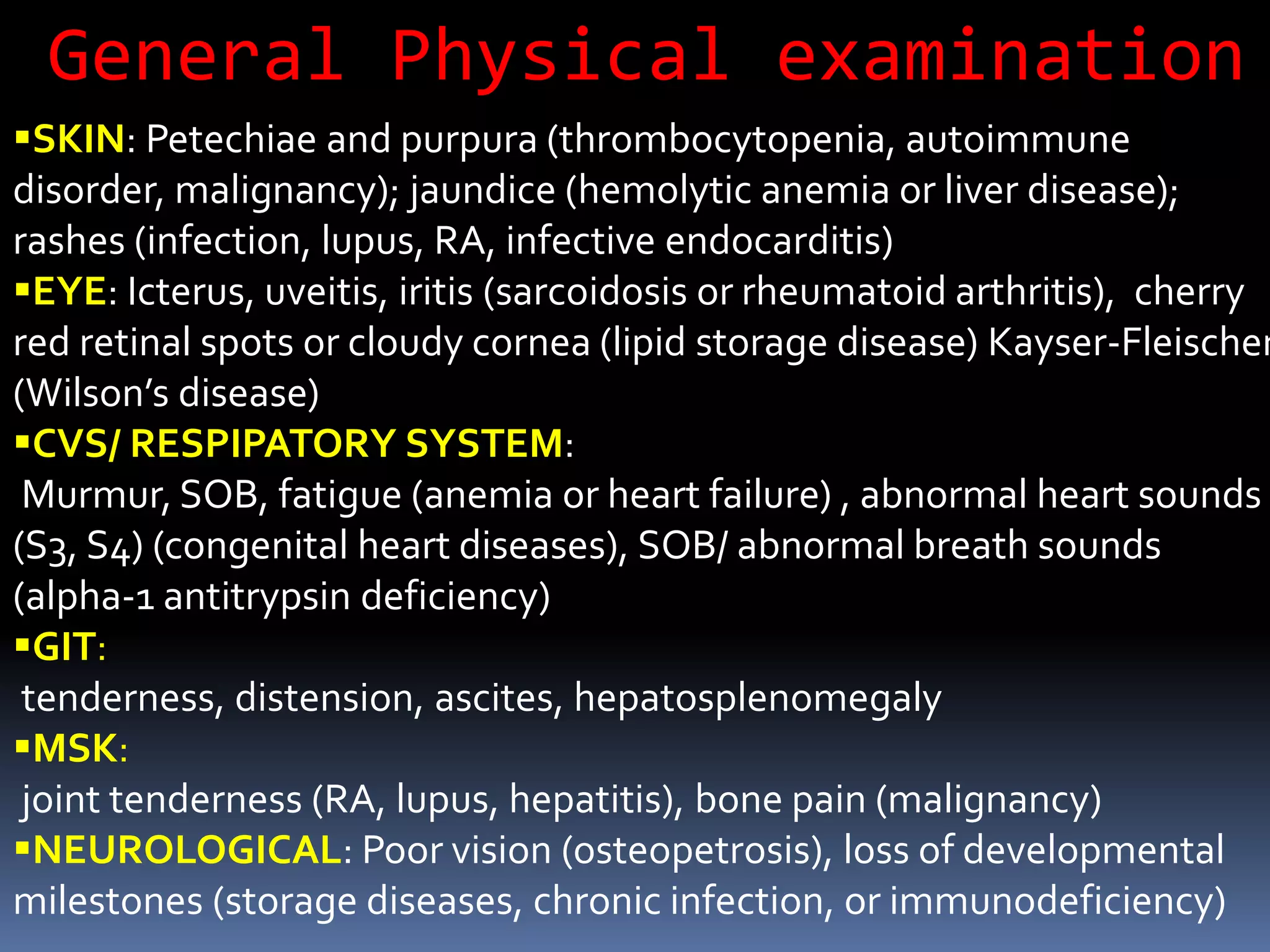
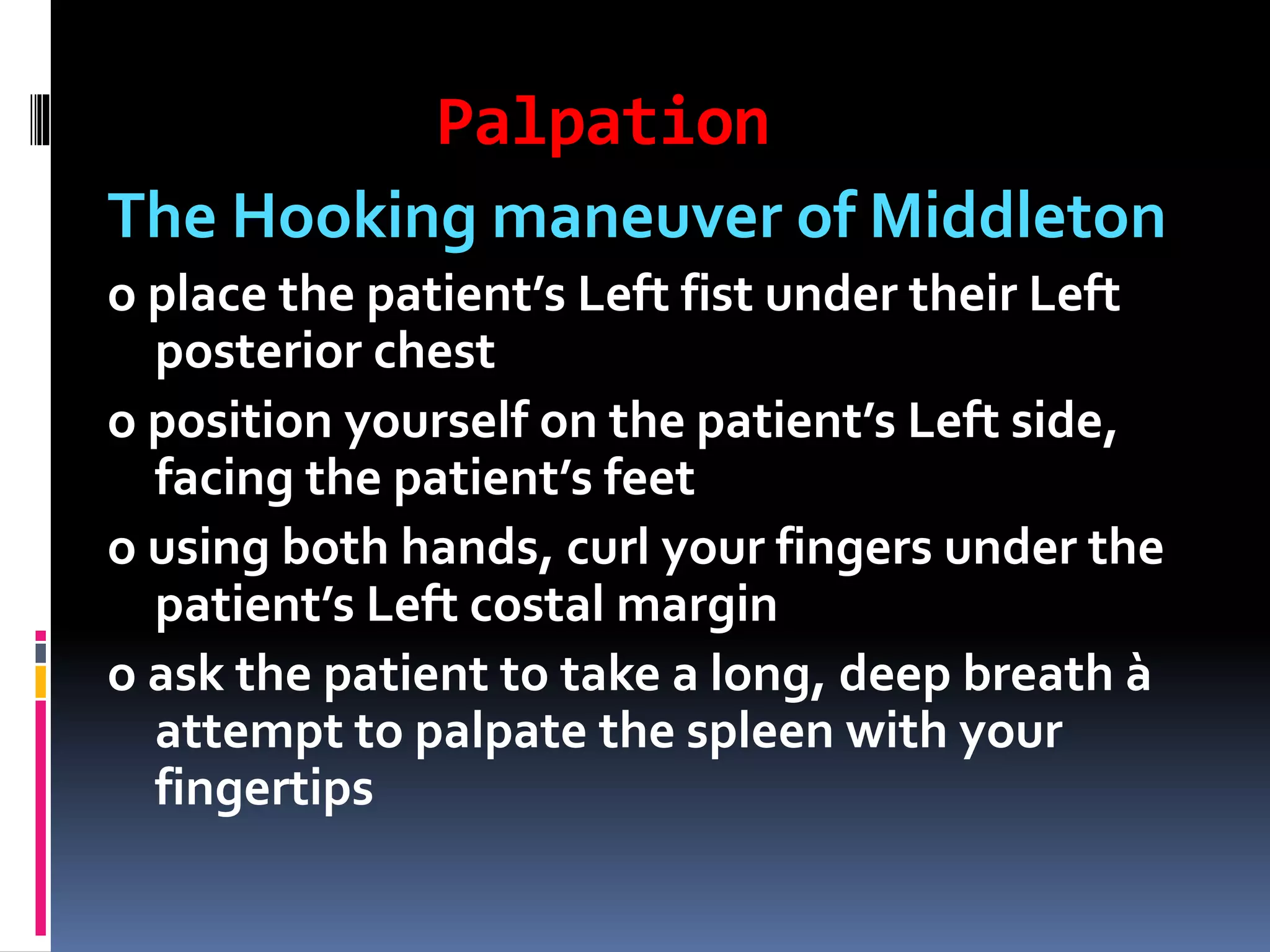
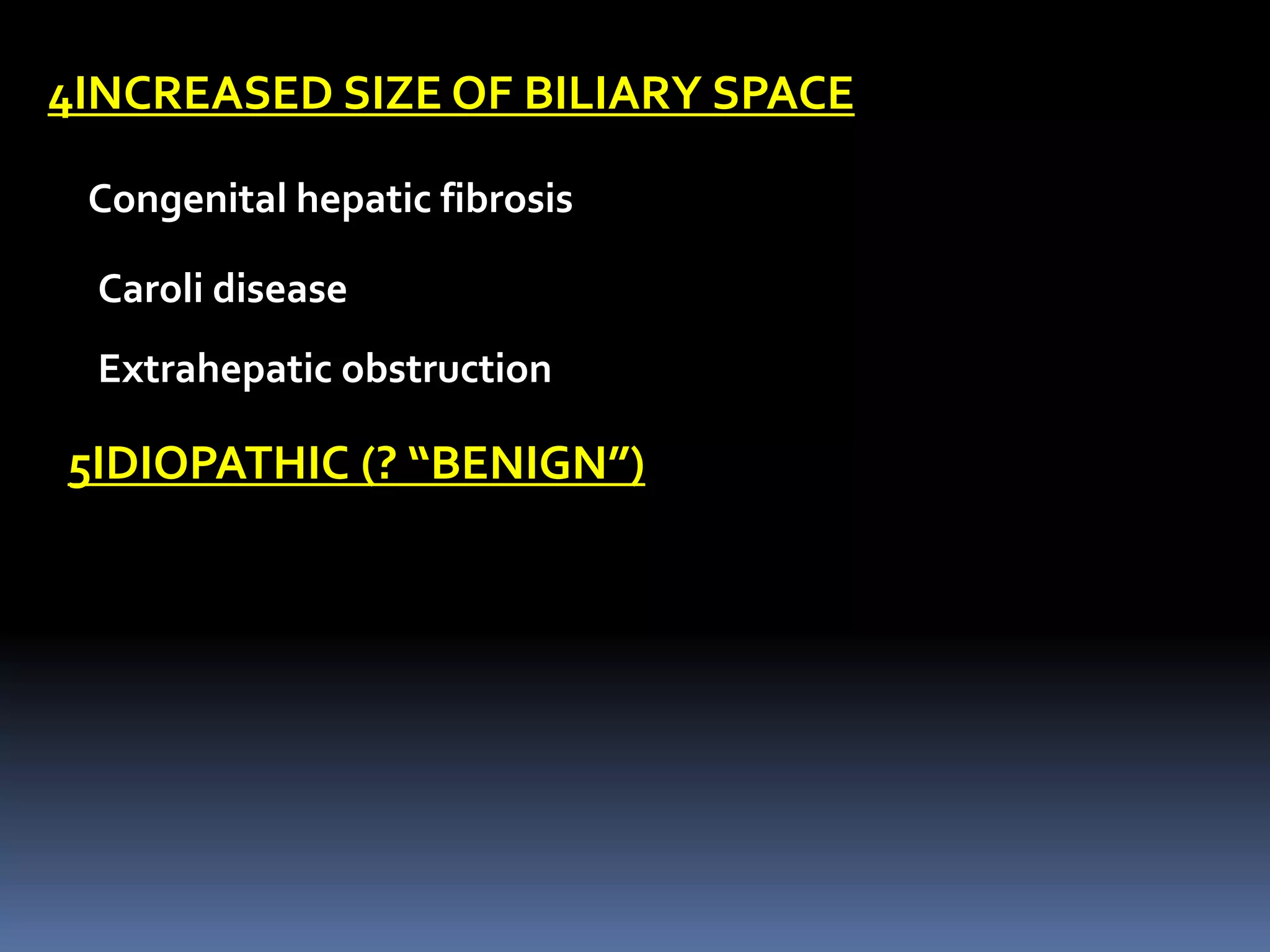
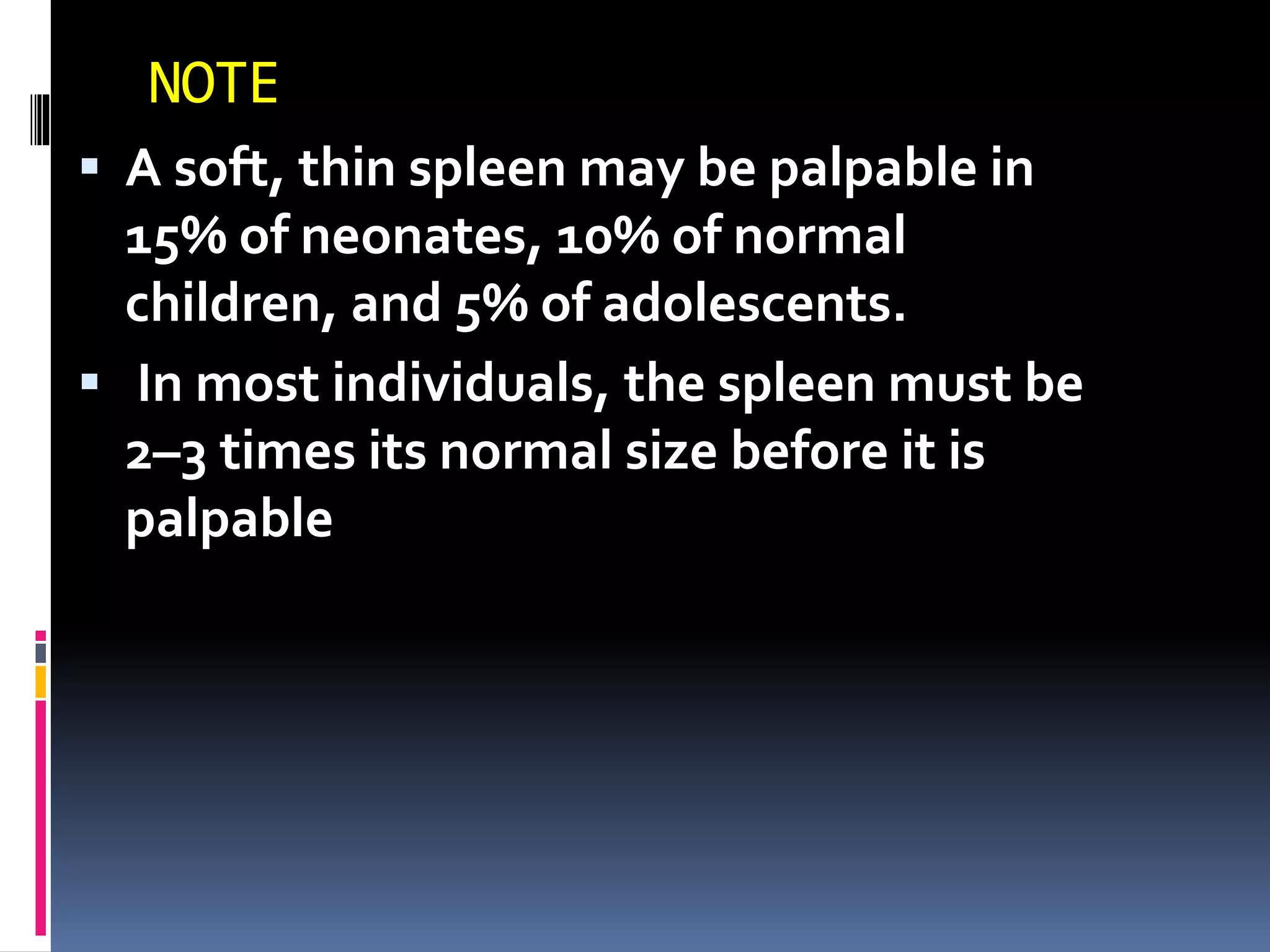
![Pathophysiology of
splenomegaly
1ANATOMIC LESIONS
Cysts, pseudocysts ,Hamartomas, Polysplenia
syndrome Hemangiomas and lymphangiomas
Hematoma or rupture (traumatic) Hamartoma
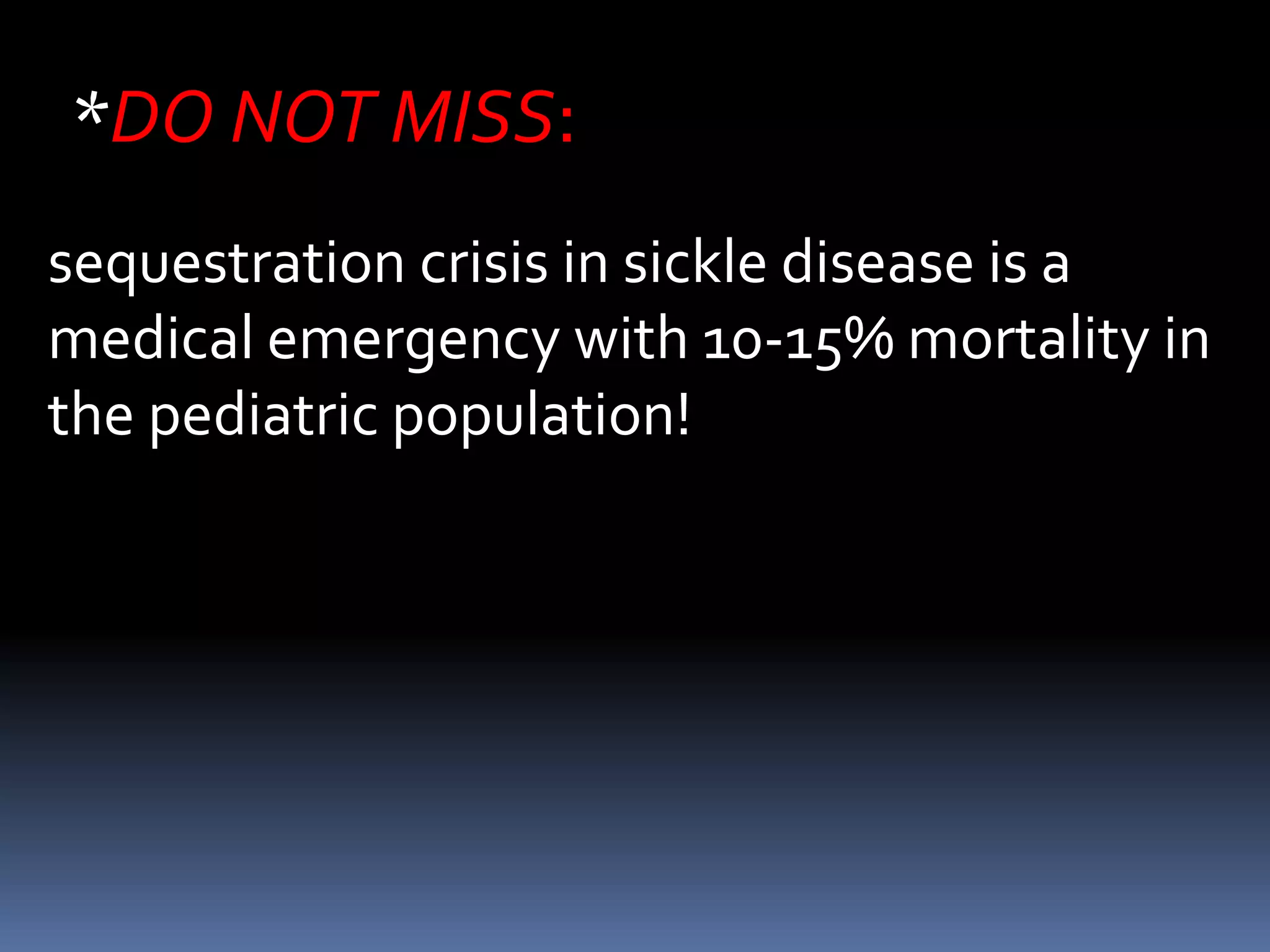
2HYPERPLASIA CAUSED BY HEMATOLOGIC
DISORDERS
Acute and Chronic Hemolysis[*]
Hemoglobinopathies (sickle cell disease in
infancy with or without sequestration crisis](https://image.slidesharecdn.com/anapproachtoachildwithhepatosplenomegalyandlymphadenopathy-180818120204/75/An-approach-to-a-child-with-hepatosplenomegaly-and-lymphadenopathy-16-2048.jpg)
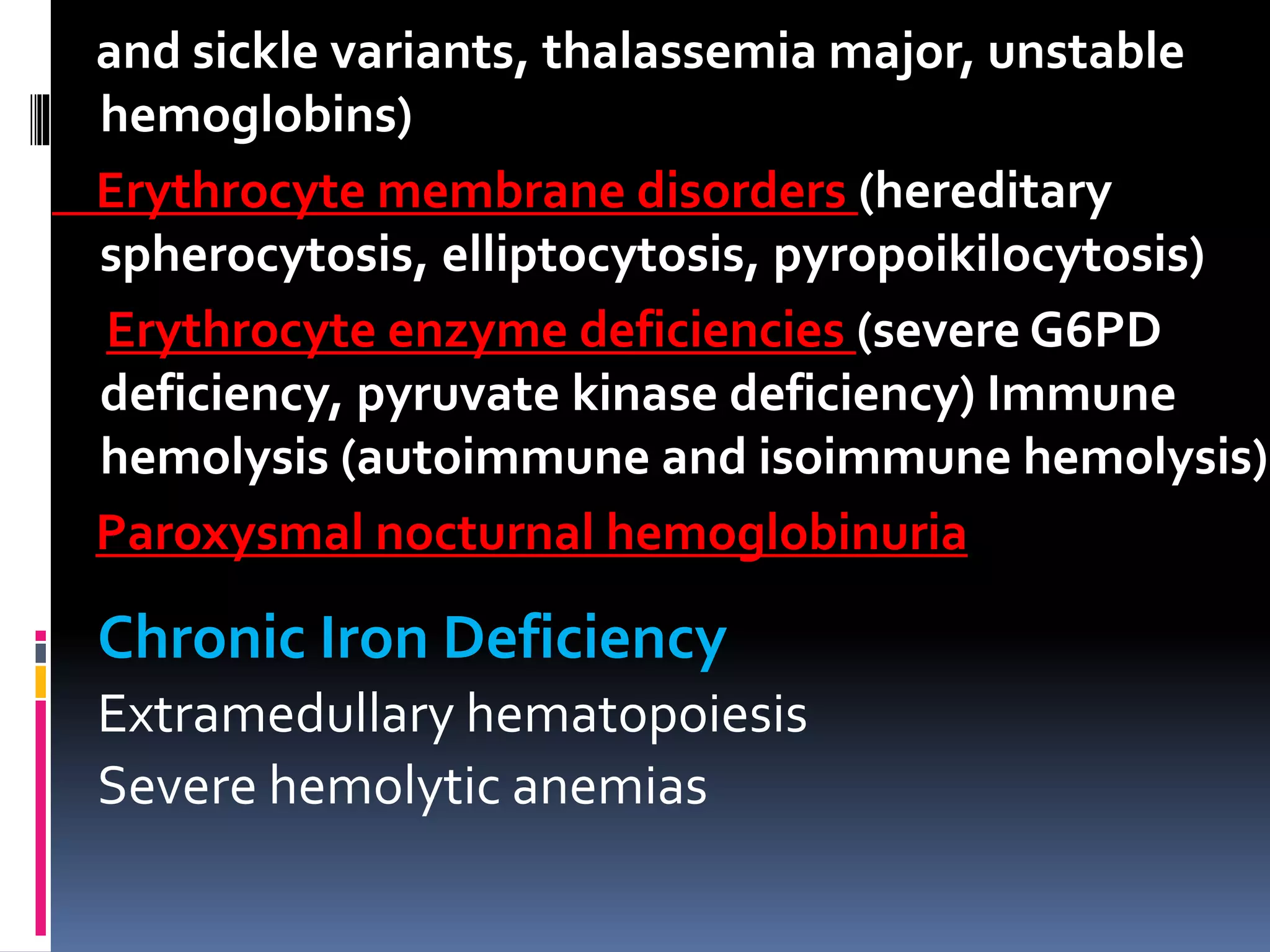
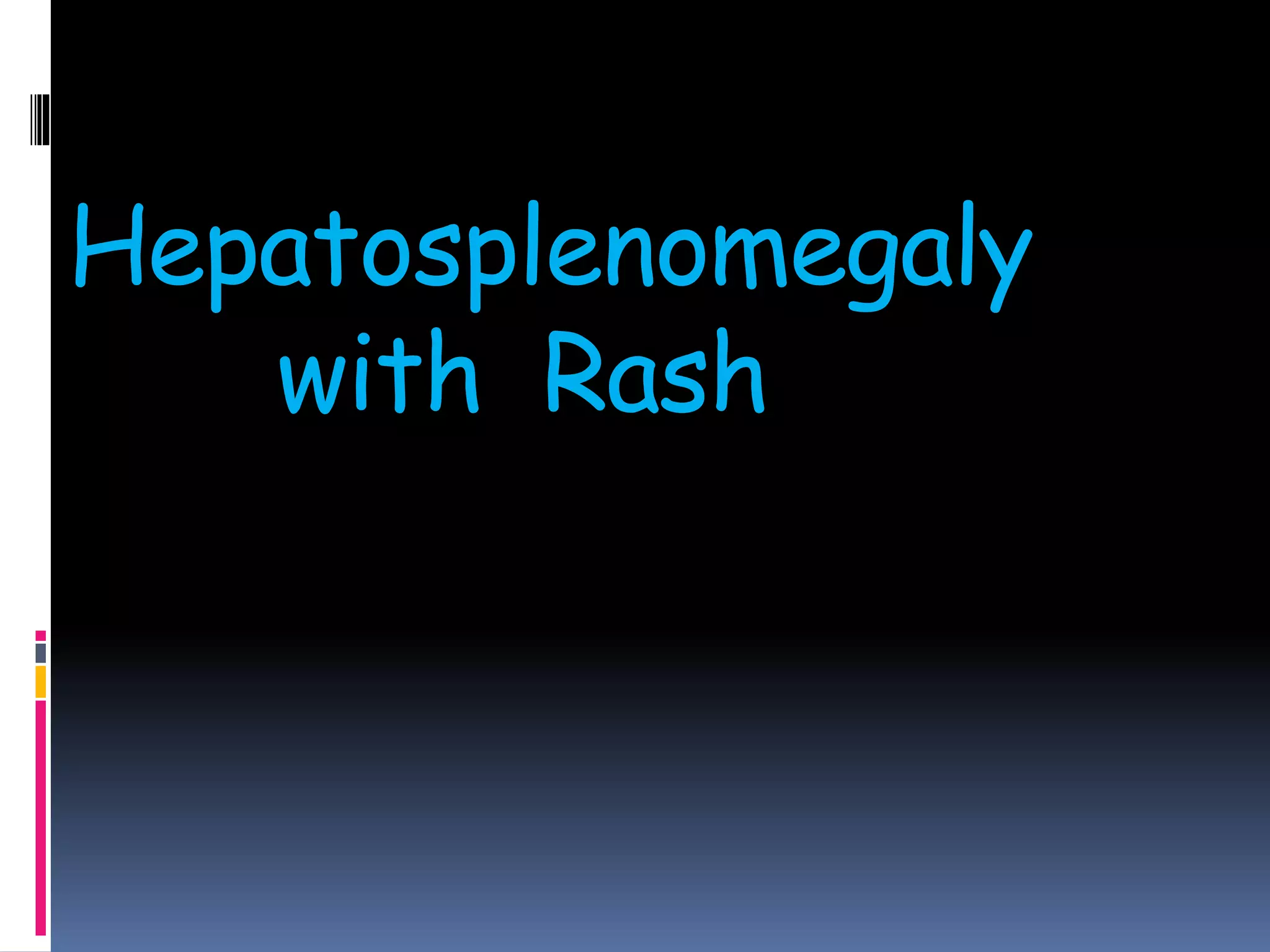
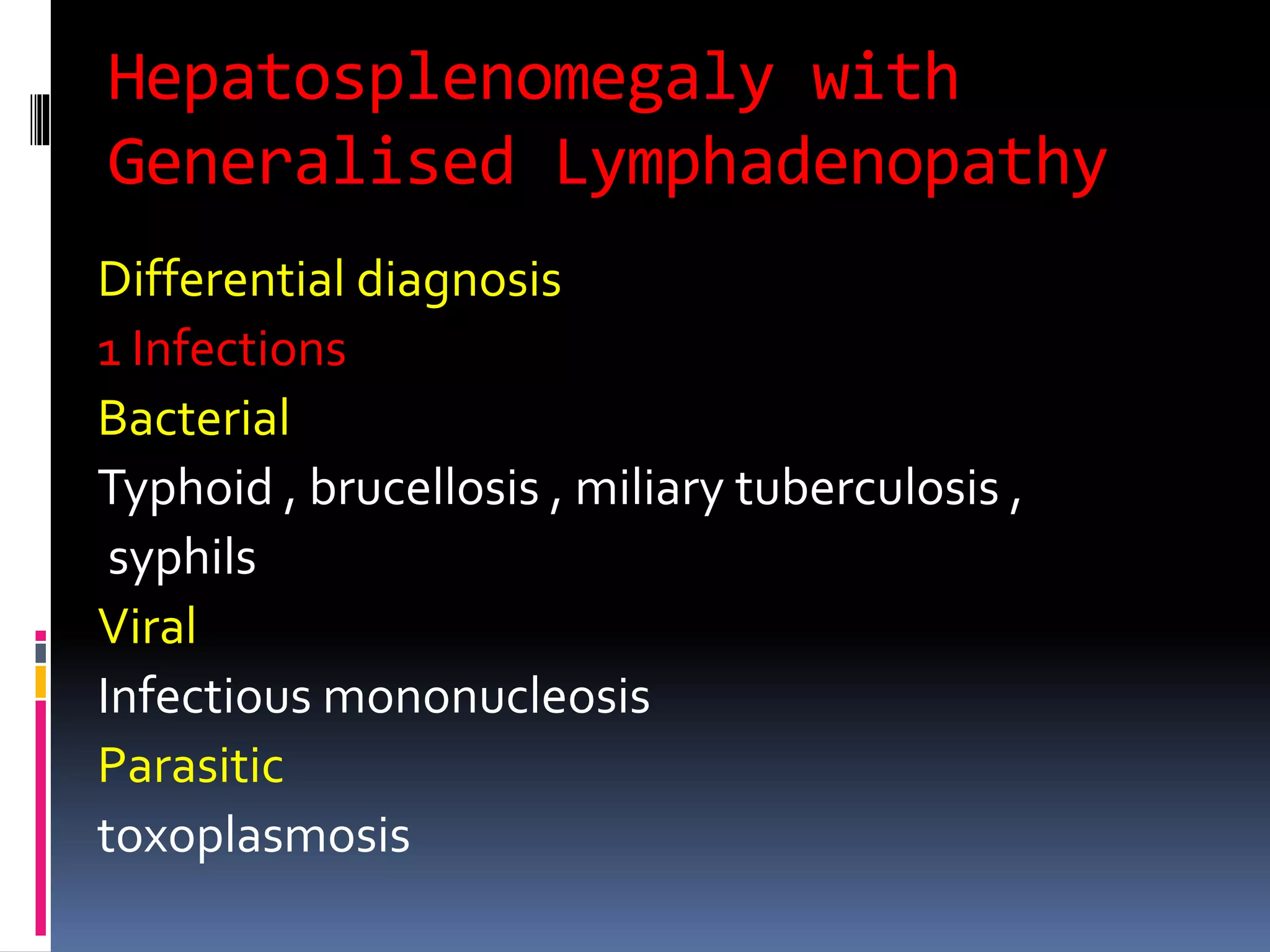
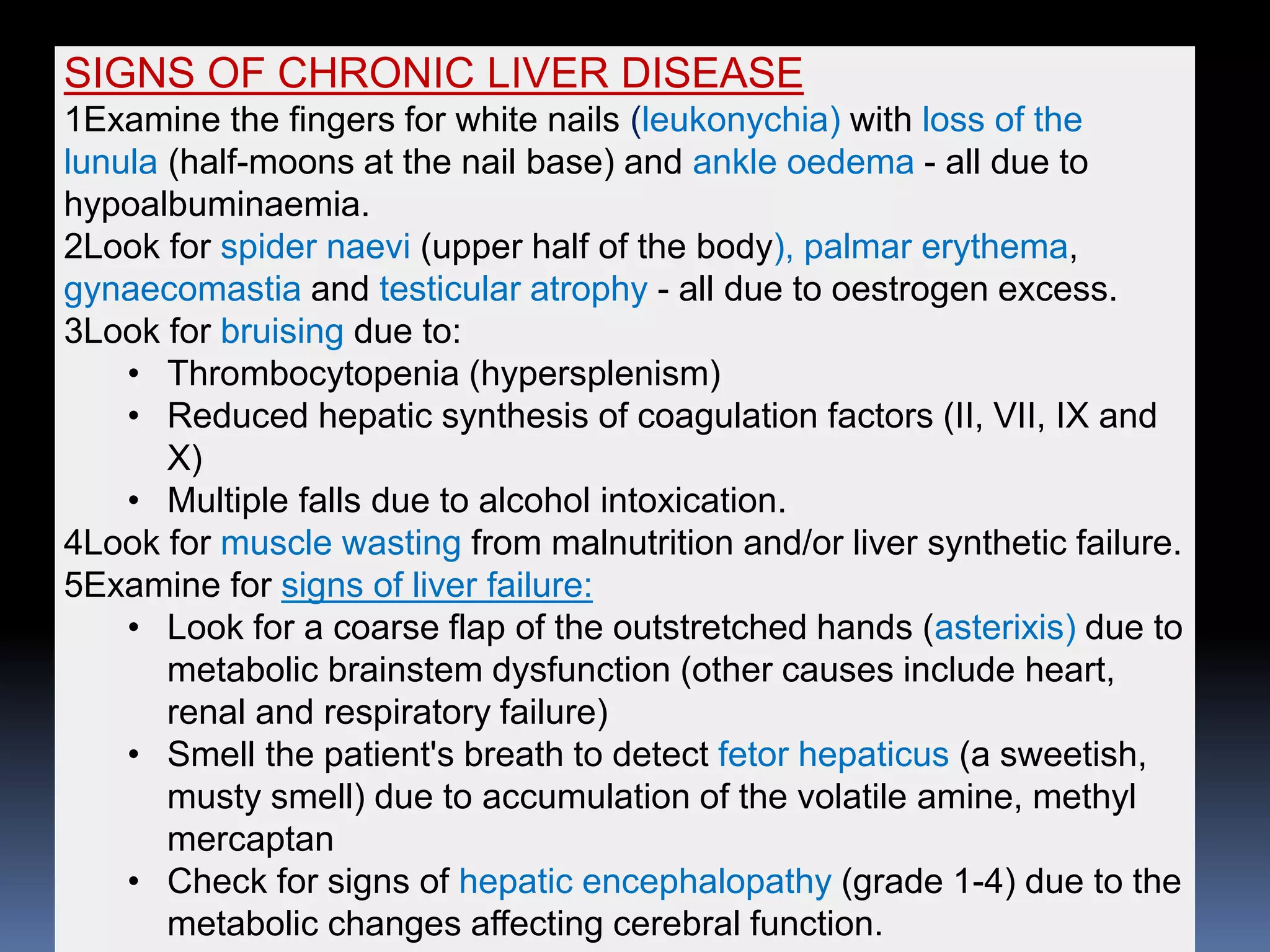
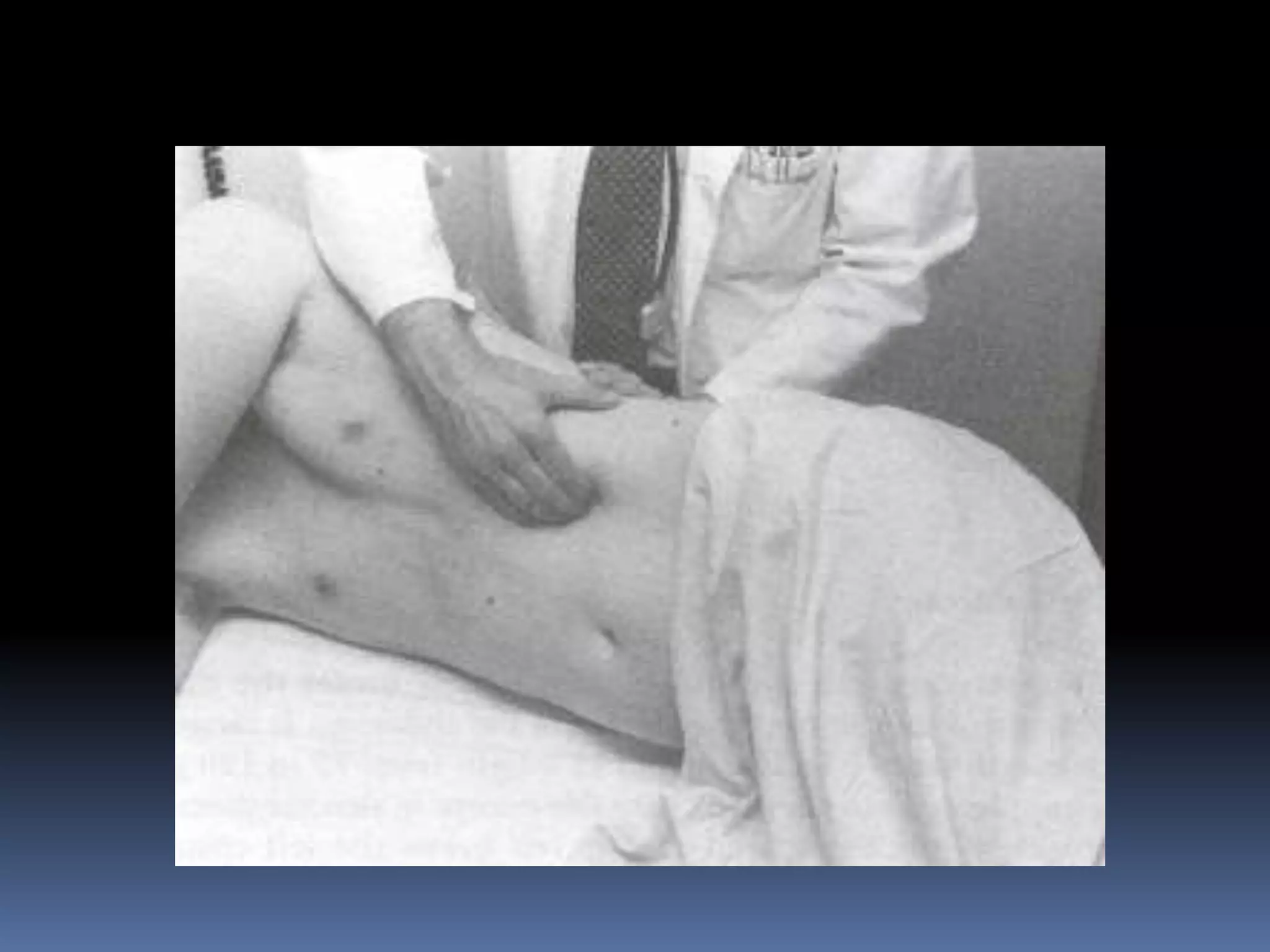
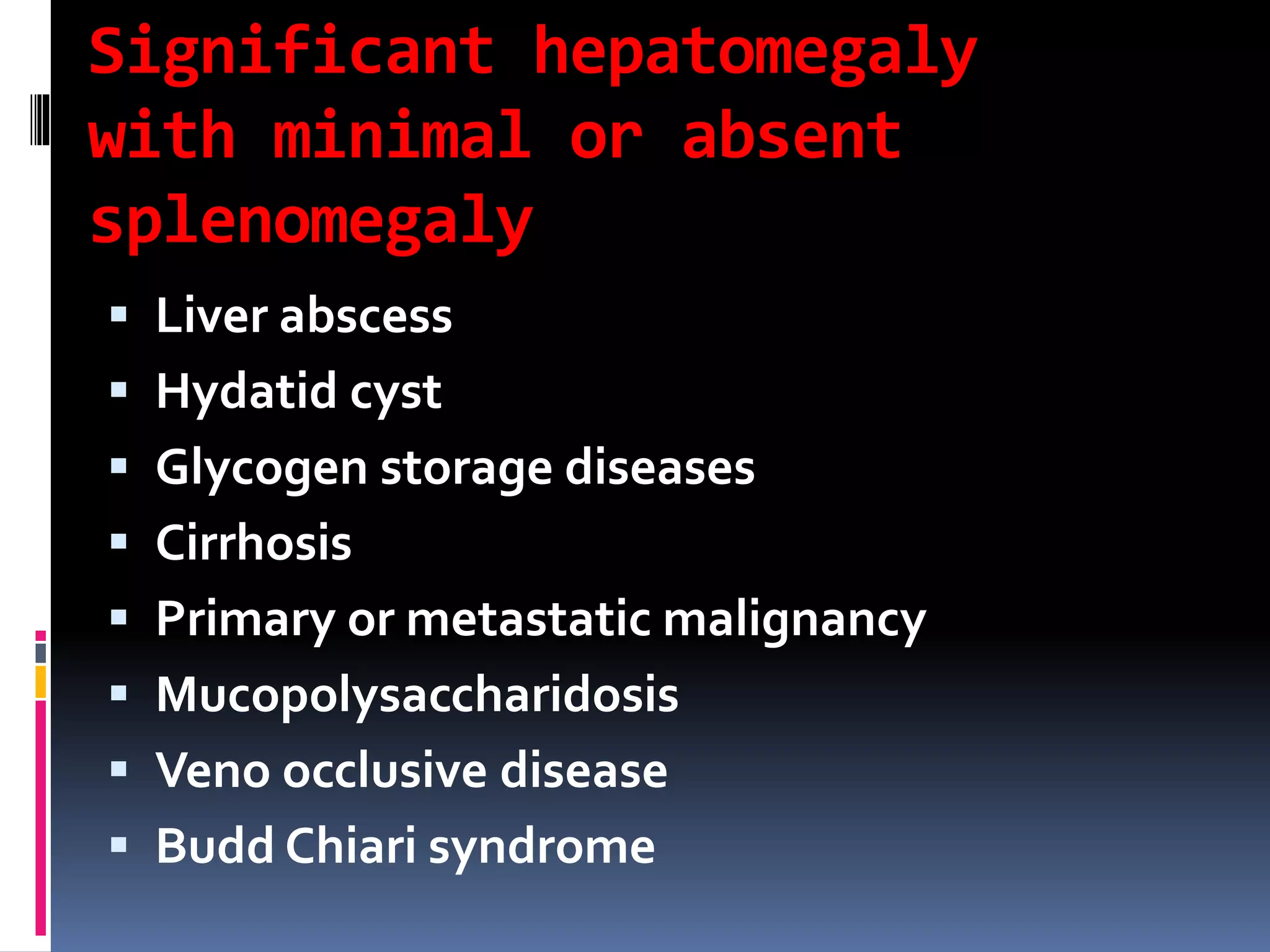
![ Myeloproliferative diseases:
chronic myelogenous leukemia (CML), juvenile CML,
myelofibrosis with myeloid metaplasia, polycythemia vera
Osteopetrosis
Patients receiving granulocyte and granulocyte-macrophage
colony-stimulating factors
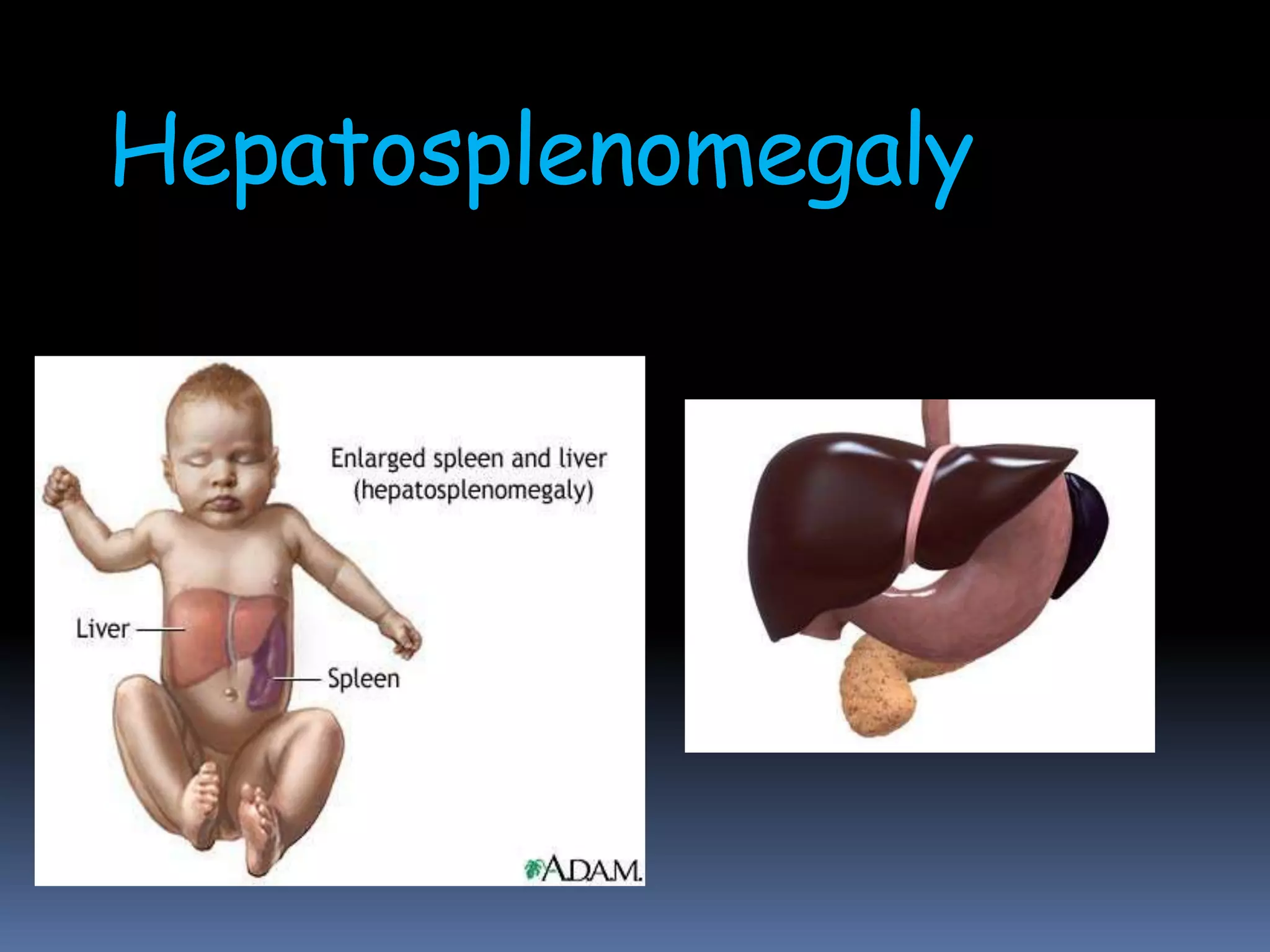
3 INFECTIONS[†]
Bacterial
Acute sepsis: Salmonella typhi, Streptococcus pneumoniae,
Haemophilus influenzae type b, Staphylococcus aureus
Chronic infections: infective endocarditis, chronic
meningococcemia, brucellosis, tularemia, cat-scratch disease
Local infections: splenic abscess (S. aureus, streptococci,
less often Salmonella species, polymicrobial species),
pyogenic liver abscess (anaerobic bacteria, gram-negative
enteric bacteria), cholangitis](https://image.slidesharecdn.com/anapproachtoachildwithhepatosplenomegalyandlymphadenopathy-180818120204/75/An-approach-to-a-child-with-hepatosplenomegaly-and-lymphadenopathy-18-2048.jpg)
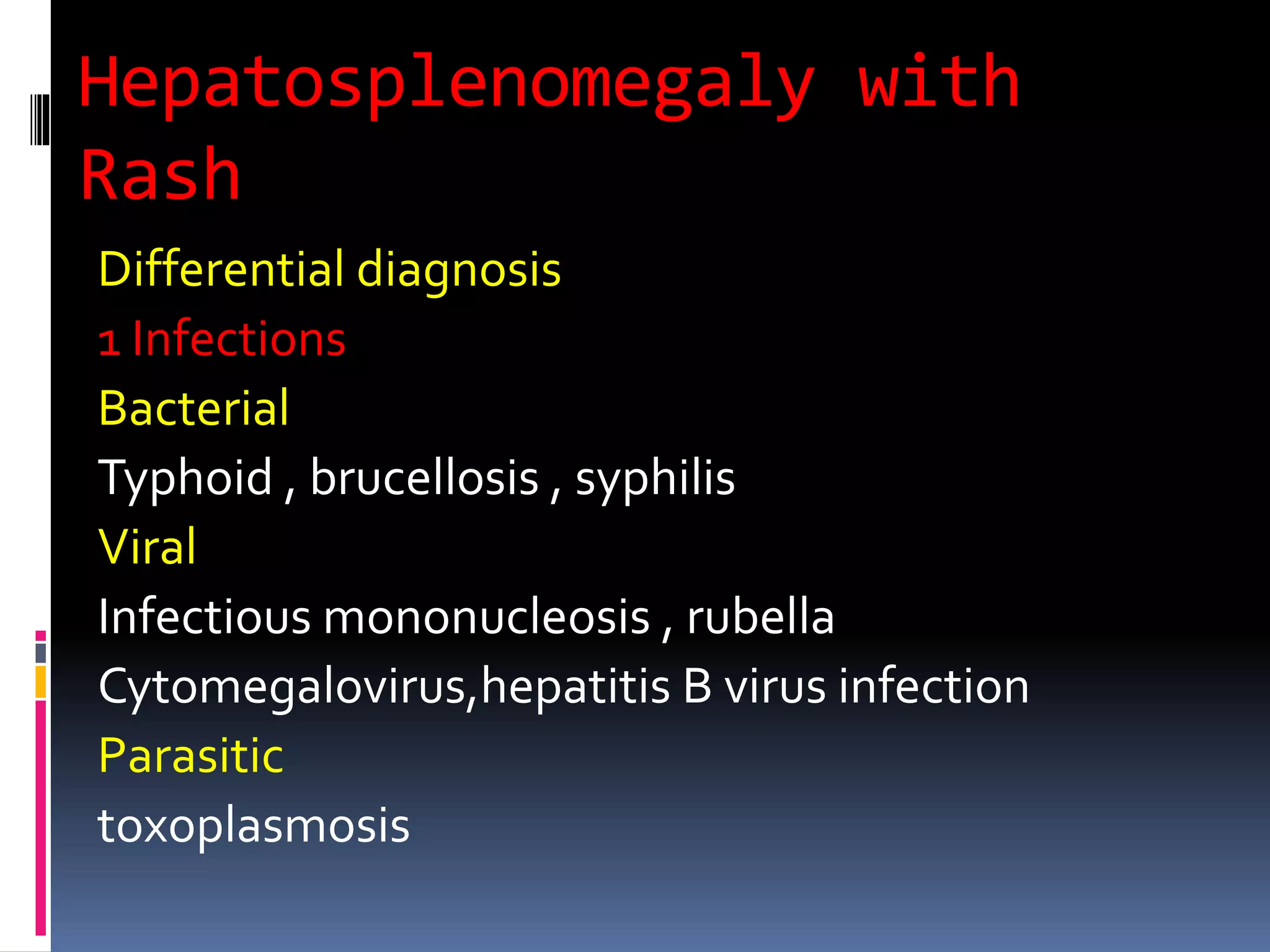
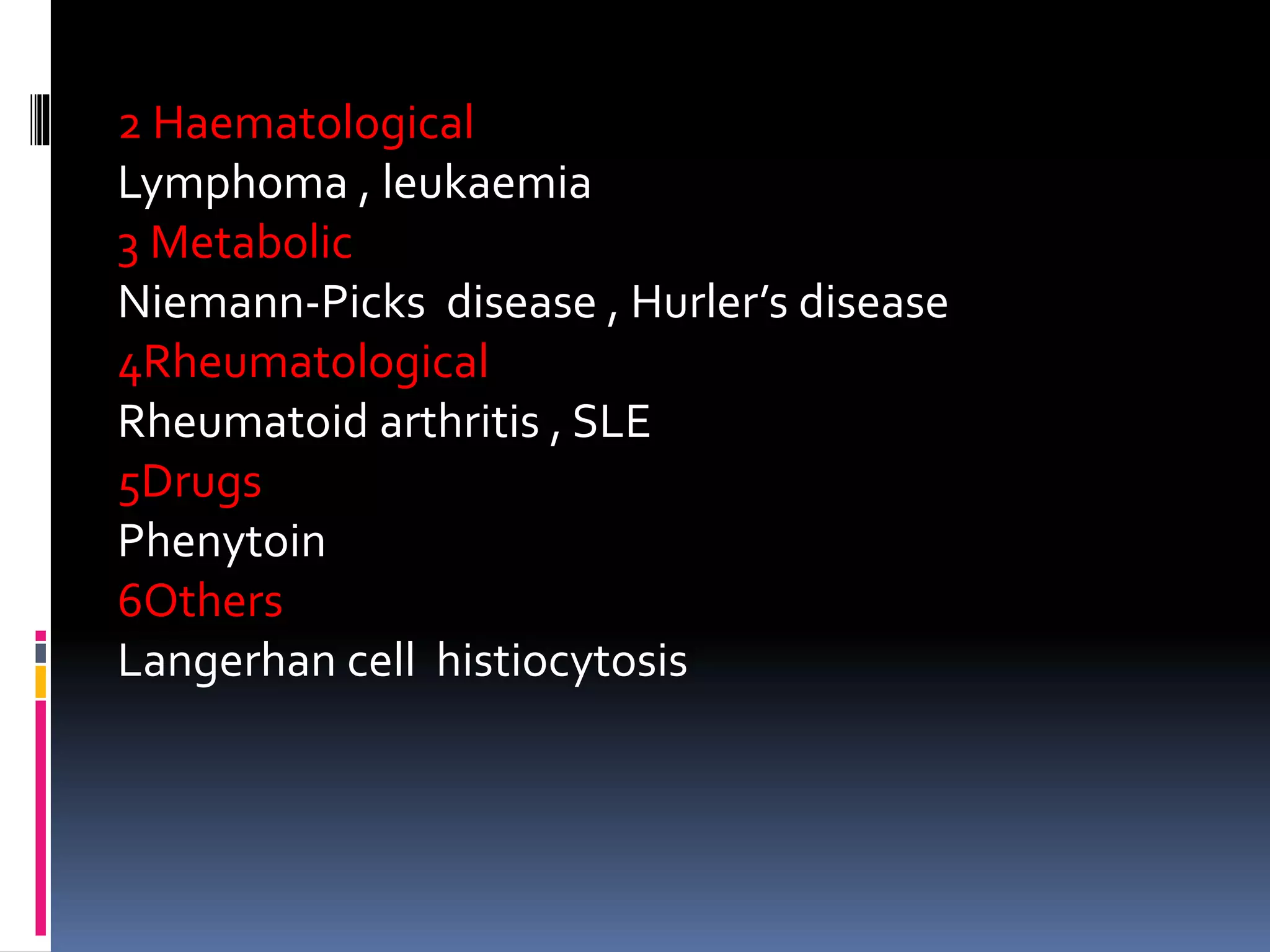
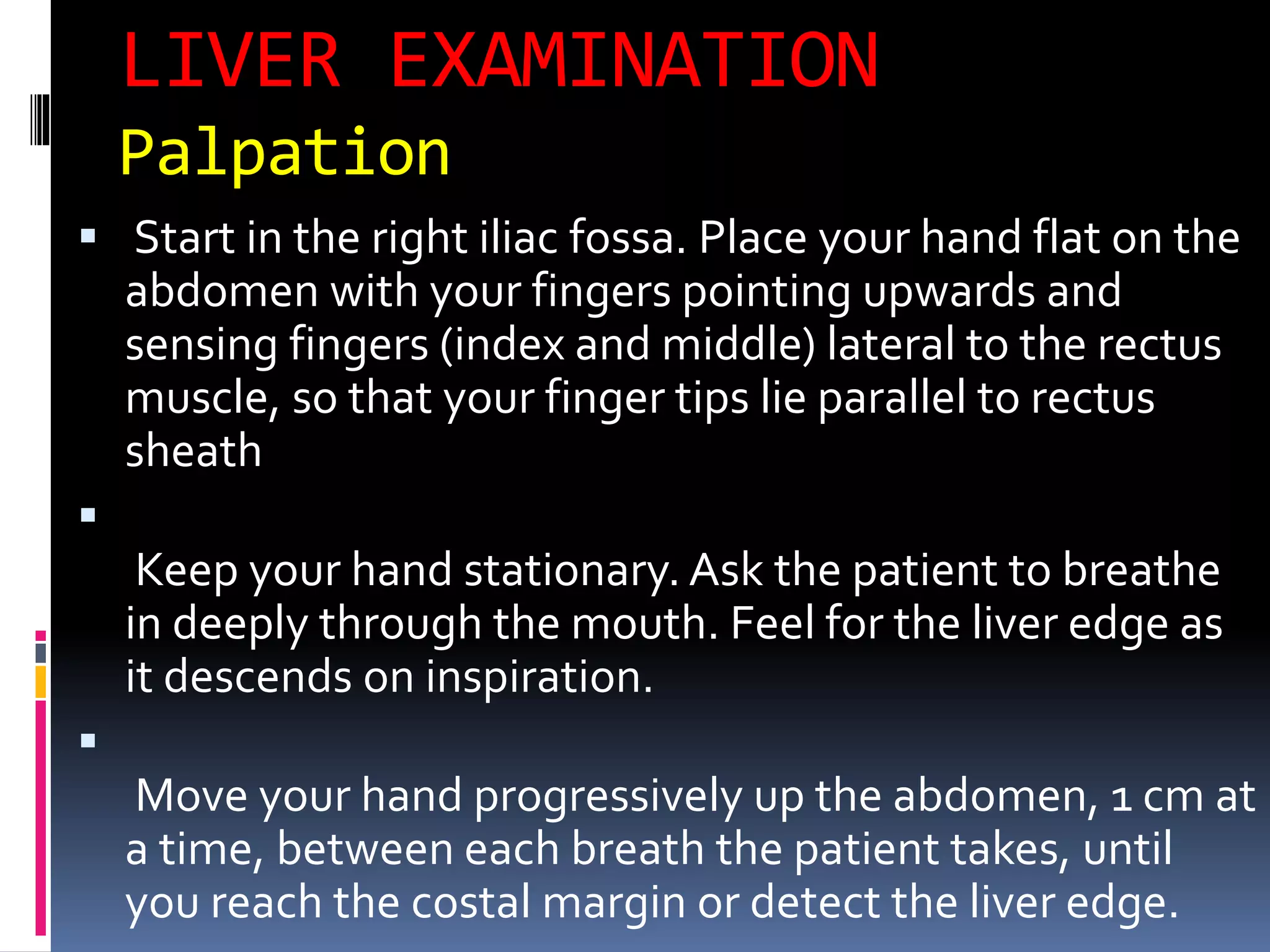
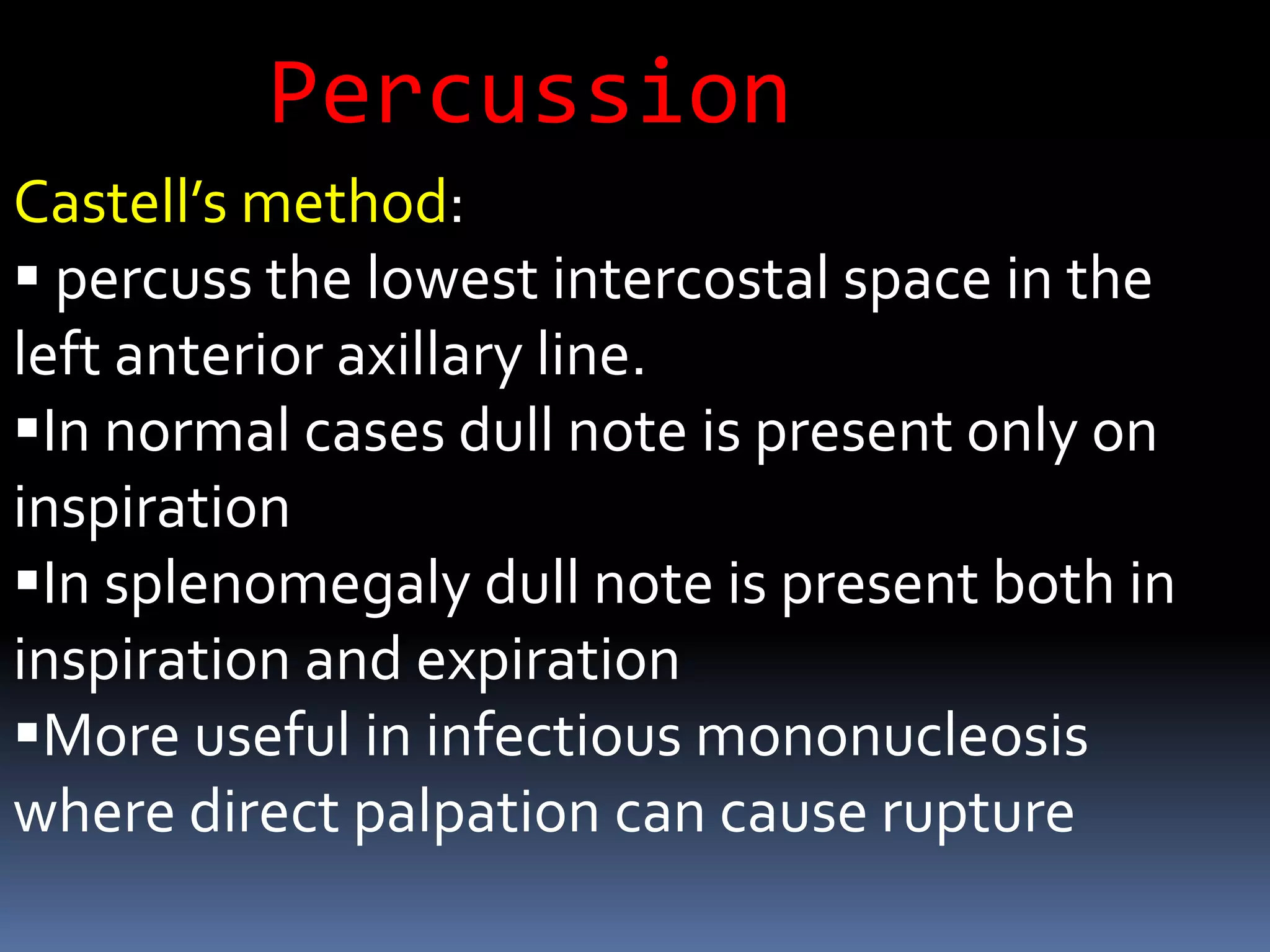
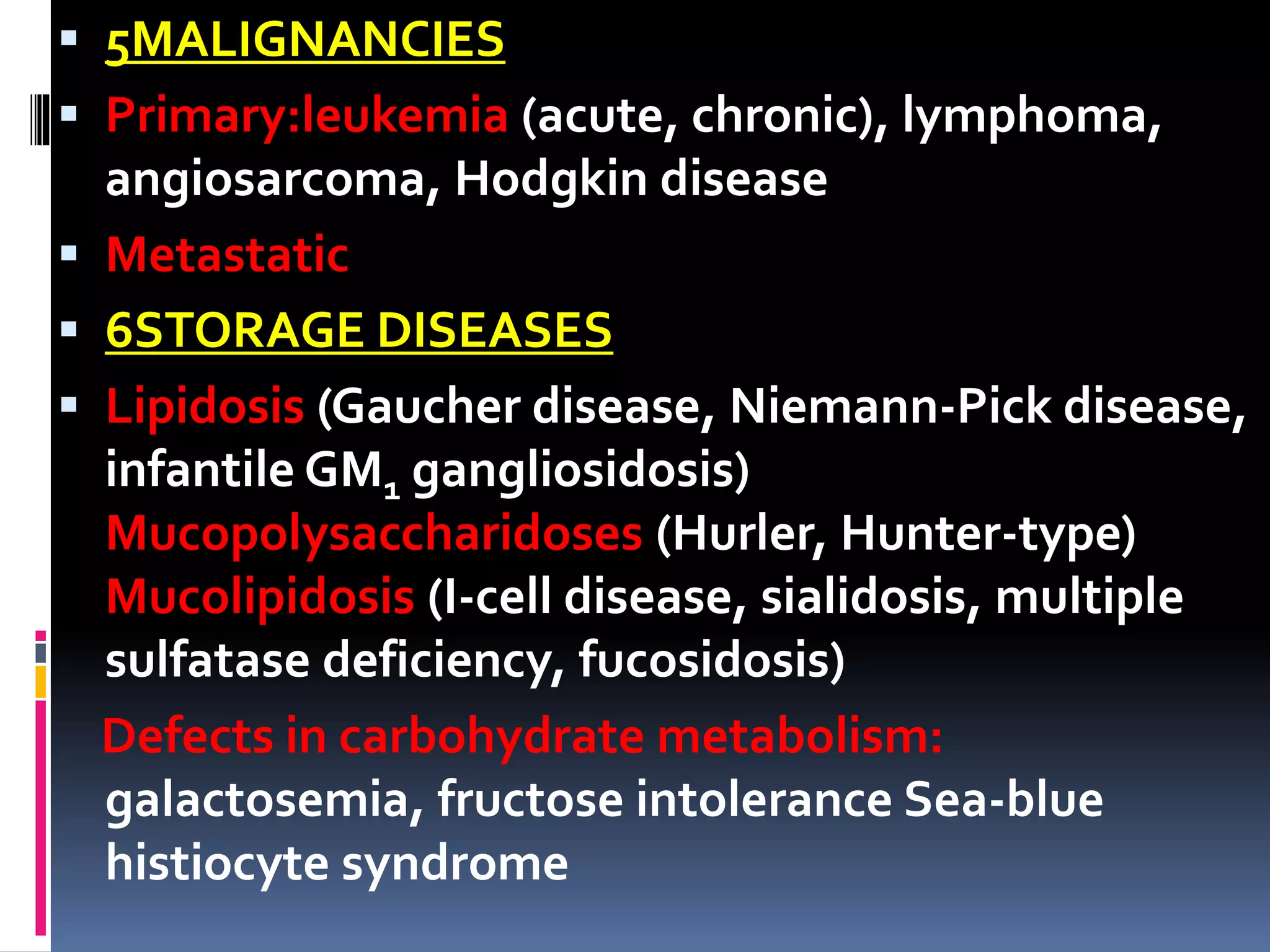
![ Viral[*]
Acute viral infections, especially in children
Congenital cytomegalovirus (CMV), herpes simplex,
rubella Hepatitis, A, B, and C;CMV Epstein-Barr virus
(EBV)Viral hemophagocytic syndromes: CMV, EBV,
HHV-6 Human immunodeficiency virus (HIV)
Spirochetal
Syphilis, especially congenital syphilis Leptospirosis
Rickettsial
Rocky Mountain spotted fever Q feverTyphus
Fungal/Mycobacterial Miliary tuberculosis
Disseminated histoplasmosis South American
blastomycosis Systemic candidiasis (in
immunosuppressed patients)](https://image.slidesharecdn.com/anapproachtoachildwithhepatosplenomegalyandlymphadenopathy-180818120204/75/An-approach-to-a-child-with-hepatosplenomegaly-and-lymphadenopathy-19-2048.jpg)
![ Parasitic
MalariaToxoplasmosis, especially congenital
Toxocara canis,Toxocara cati (visceral larva migrans)
Leishmaniasis (kala-azar) Schistosomiasis (hepatic-
portal involvement)Trypanosomiasis Fascioliasis
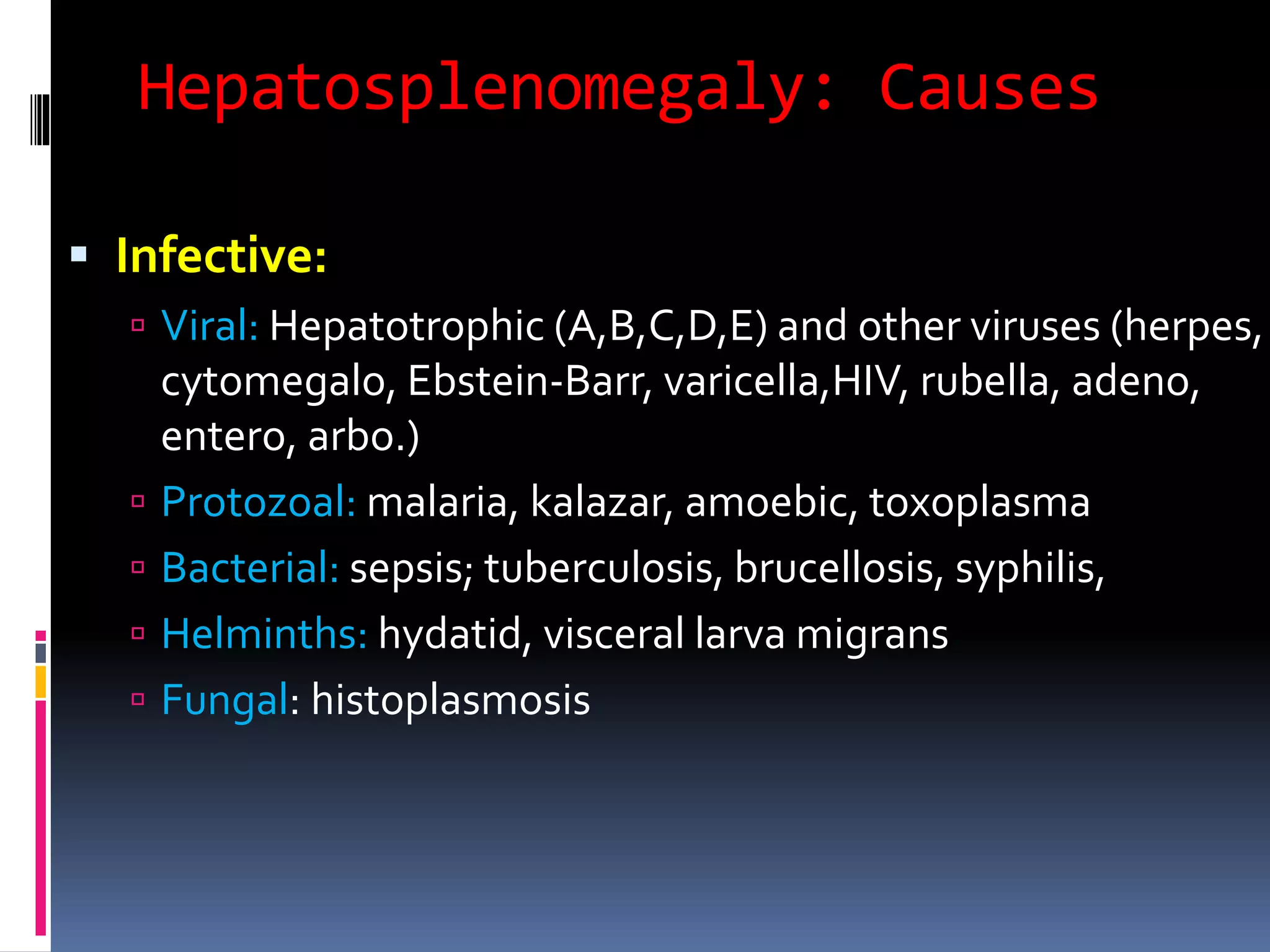
4IMMUNOLOGICAND INFLAMMATORY
PROCESSES[*]
Systemic lupus erythematosus Rheumatoid arthritis,
Mixed connective tissue disease Systemic vasculitis
,Serum sickness, Drug hypersensitivity, especially to
phenytoin ,Graft vs host disease, Sjögren syndrome,
Cryoglobulinemia ,Amyloidosis ,Sarcoidosis, Large
granular lymphocytosis and neutropenia
,Histiocytosis syndromes, Hemophagocytic
syndromes (nonviral, familial)](https://image.slidesharecdn.com/anapproachtoachildwithhepatosplenomegalyandlymphadenopathy-180818120204/75/An-approach-to-a-child-with-hepatosplenomegaly-and-lymphadenopathy-20-2048.jpg)
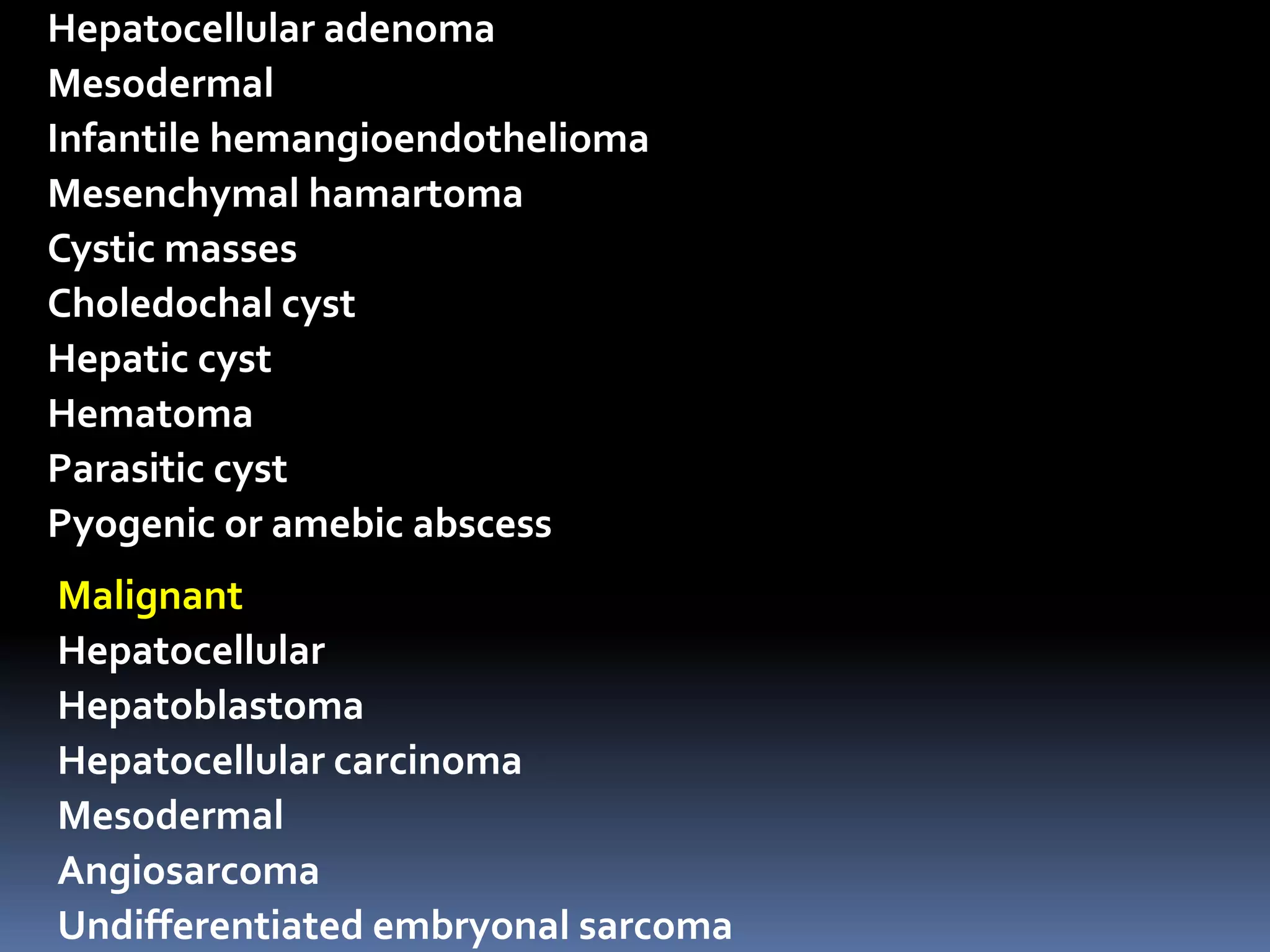
![ 7CONGESTIVE[*]
Heart failure
Intrahepatic cirrhosis or fibrosis
Extrahepatic portal (thrombosis), splenic,
and hepatic vein obstruction (thrombosis,
Budd-Chiari syndrome](https://image.slidesharecdn.com/anapproachtoachildwithhepatosplenomegalyandlymphadenopathy-180818120204/75/An-approach-to-a-child-with-hepatosplenomegaly-and-lymphadenopathy-22-2048.jpg)