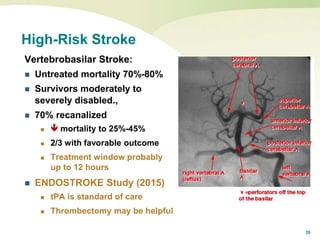
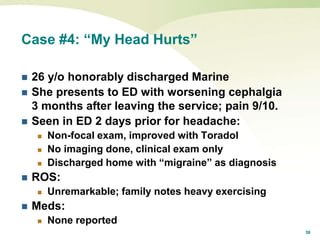
This document presents 4 case studies to discuss barriers to correct diagnosis in neurology. Case 1 describes a woman misdiagnosed with back pain who later presented with spinal epidural abscesses. Case 2 involves a man diagnosed with labyrinthitis who later had a cerebellar infarct. Case 3 is about a woman discharged with headaches who returned with a cerebellar infarct. The document emphasizes considering alternative diagnoses and thorough neurological exams to avoid missed diagnoses.
![6
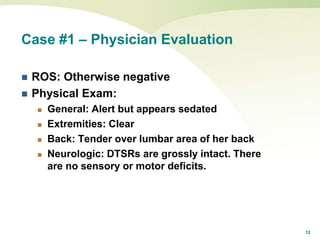
Case #1 – Physician PE
Vitals: T 98.7°F (37.1°C); P 105; R 18; BP 117/77
General: Alert and responsive. Not toxic
appearing. Does not appear to be in severe
pain. Rates pain 10/10.
HEENT: Normal
Neck: [no documented exam]
Chest: Clear, no distress, nl breath sounds
Abdomen: Soft, NT; no guarding or rebound](https://image.slidesharecdn.com/doublejeopardyneuro2016final-161020173854/85/Double-Jeopardy-Risk-in-Neurology-6-320.jpg)
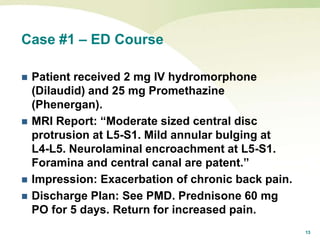
![7
Case #1 – PE Continued
Back: Diffuse pain to palpation, mid back, low
back, sciatic grooves, posterior thighs. No
point tenderness. SLR negative.
Gait: Ambulates without difficulty.
Neurologic: [There was no documented
neurologic exam].](https://image.slidesharecdn.com/doublejeopardyneuro2016final-161020173854/85/Double-Jeopardy-Risk-in-Neurology-7-320.jpg)