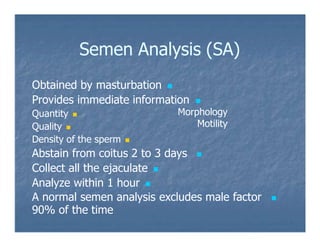
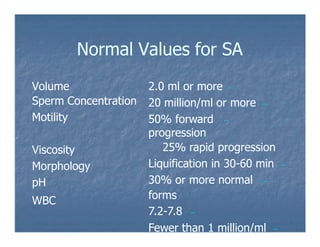
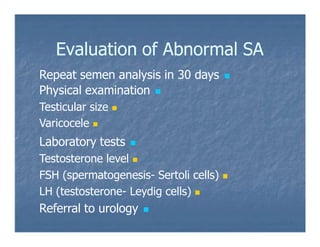
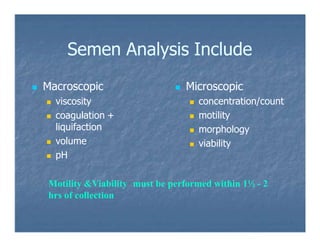
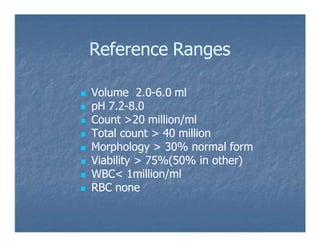
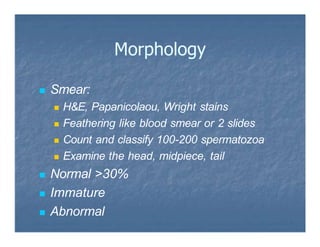
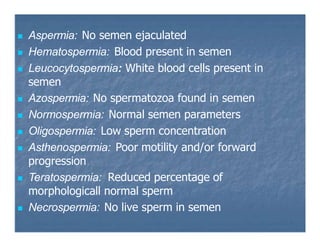
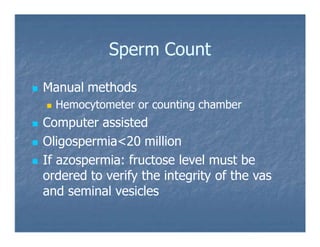
The document discusses male factor infertility, which accounts for 40% of infertility cases, focusing on abnormalities in spermatogenesis and sperm analysis metrics. It outlines causes of male infertility, such as varicocele and genetic factors, and provides detailed criteria for semen analysis including parameters for volume, motility, morphology, and overall viability. Additionally, it emphasizes the importance of proper semen collection and analysis timing to ensure accurate results in assessing male fertility.