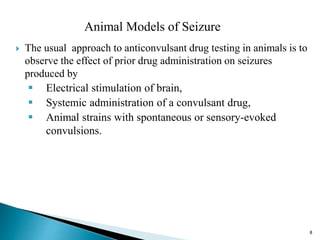
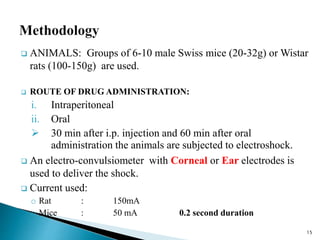
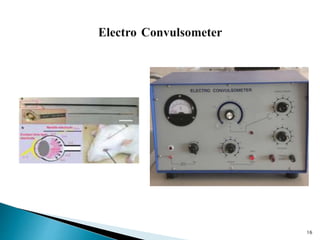
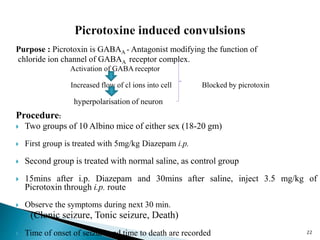
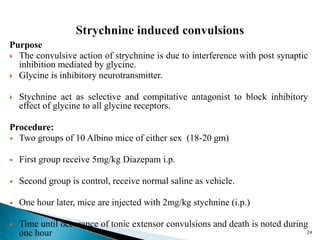
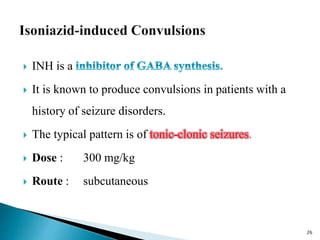
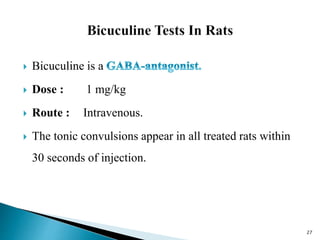
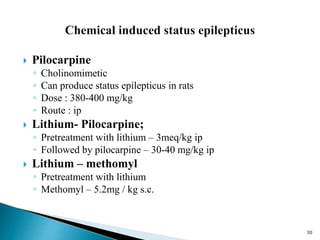
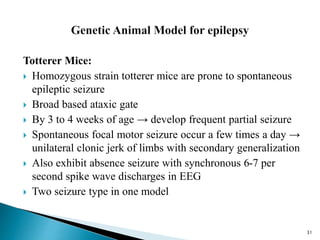
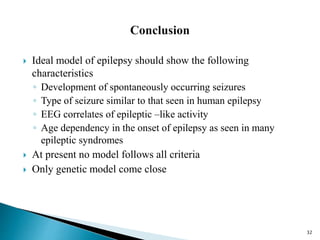
This document summarizes various preclinical screening methods used to evaluate potential anti-epileptic drugs. It describes several animal models of induced seizures including electroshock seizures, chemical-induced seizures using pentylenetetrazol or picrotoxin. It also discusses genetic models like the totterer mouse that is prone to spontaneous seizures. The key methods are maximal electroshock in mice/rats to test generalized tonic-clonic seizure protection and the pentylenetetrazol test in mice to assess anticonvulsant effects against petit mal-like seizures. These preclinical tests aim to predict potential efficacy of new compounds before clinical trials in humans.