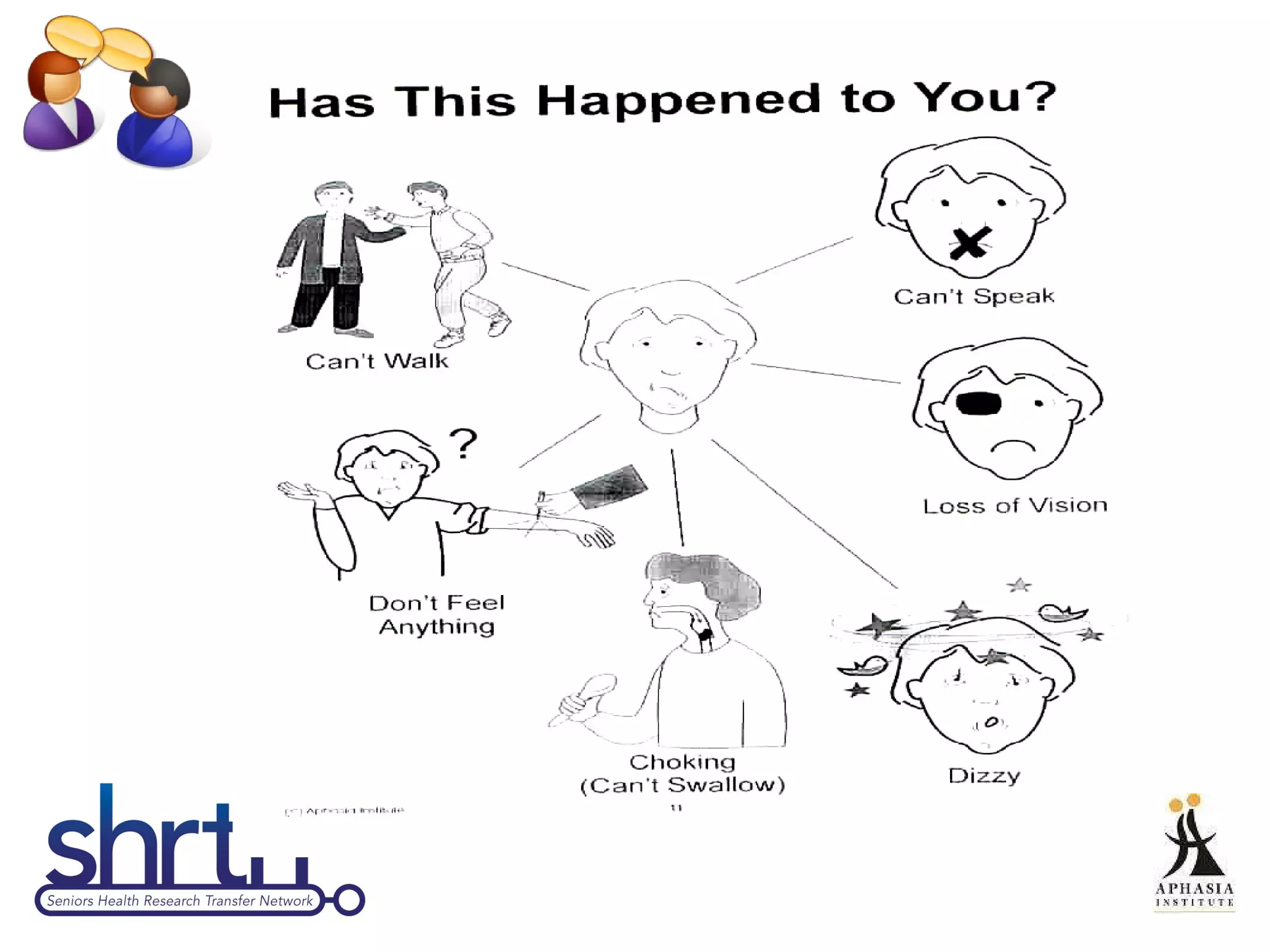
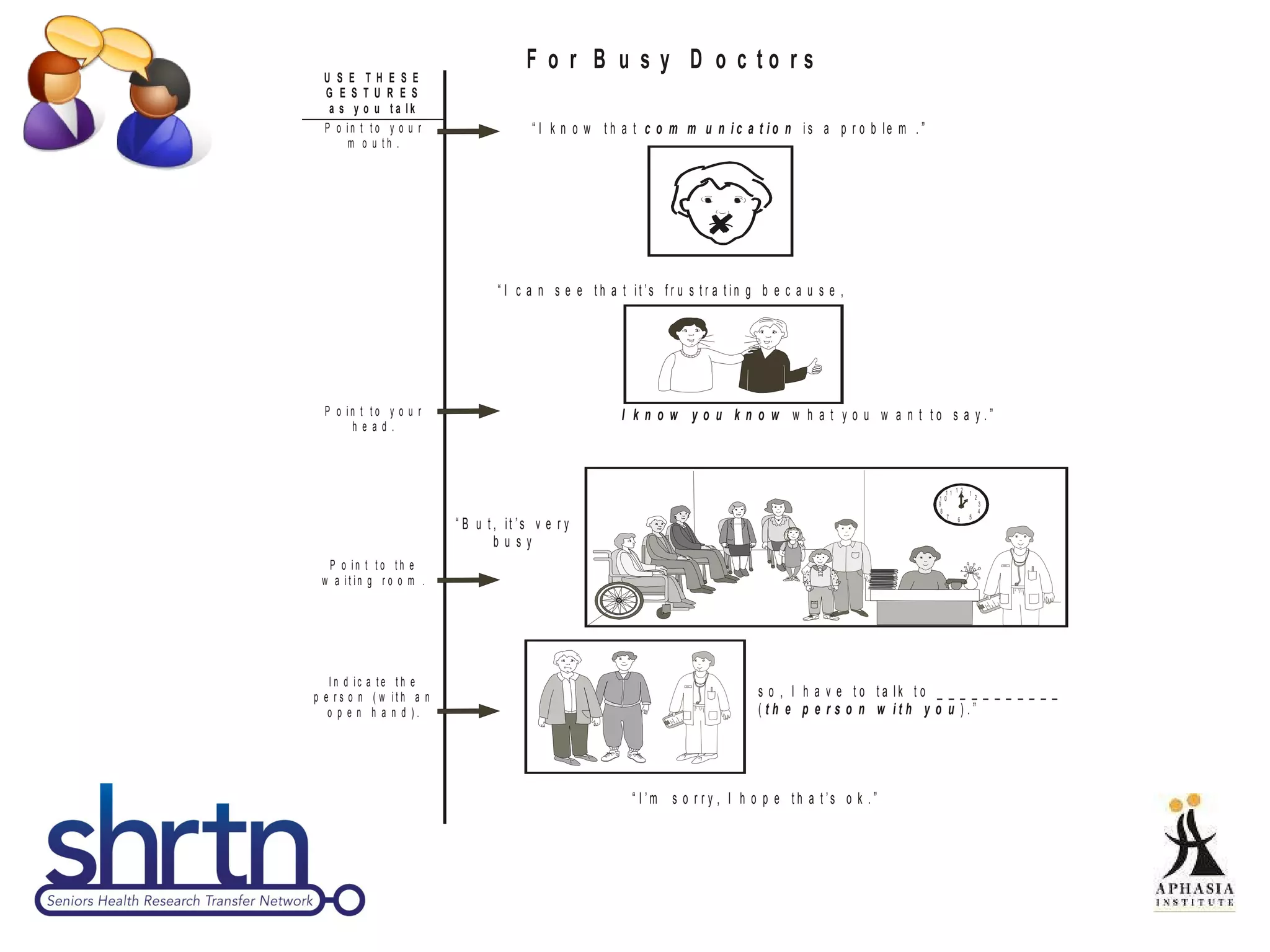
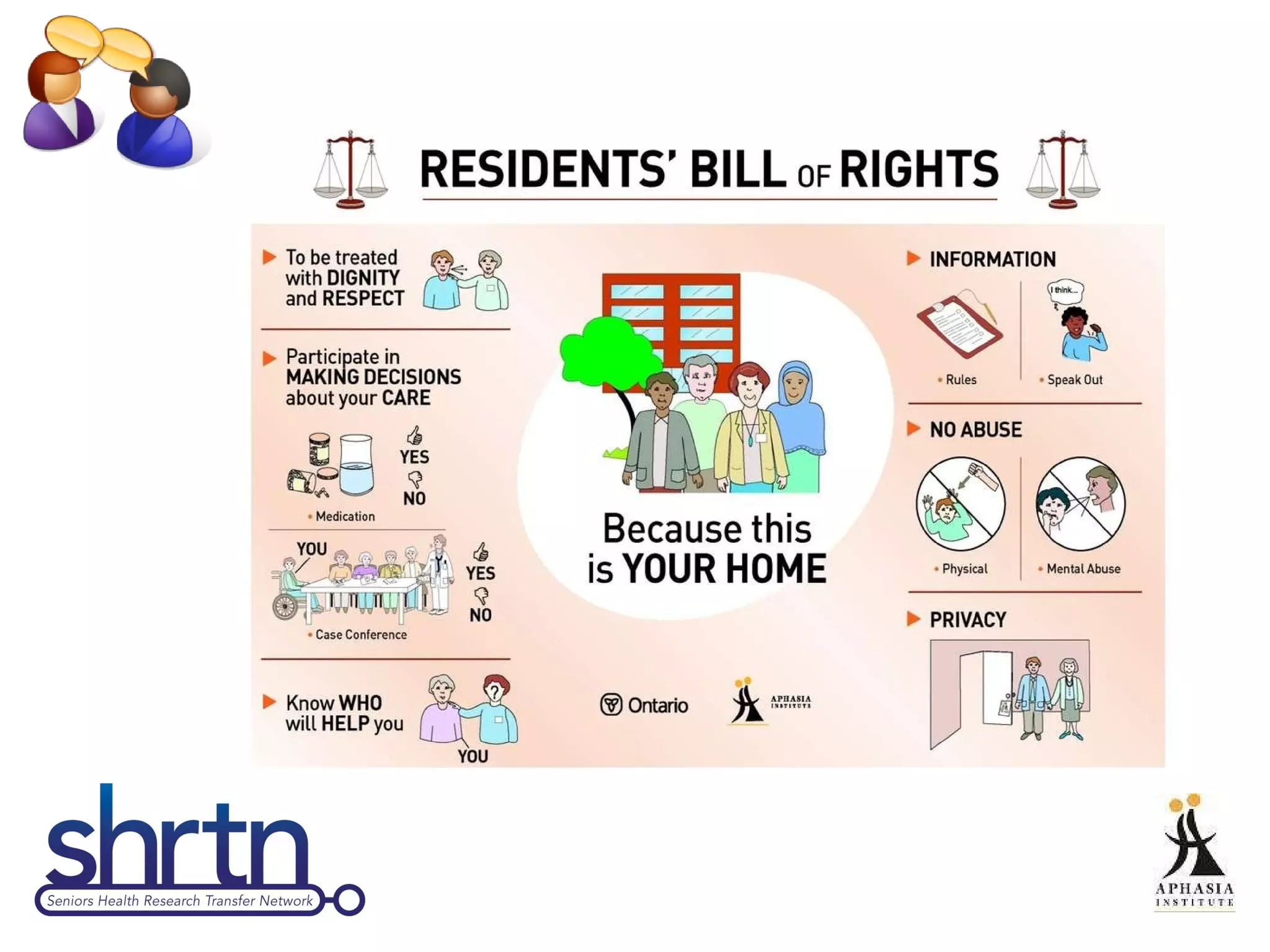
This document provides an introduction and overview of Supported Conversation for Adults with Aphasia (SCATM), a communication method that allows conversation with individuals who have difficulty expressing themselves or understanding verbal messages. It discusses what aphasia is, barriers people with aphasia face in healthcare settings, and how SCATM can be used to provide communicative access. The document includes videos, discussion questions, and prompts for interactive role plays to help users learn and practice using SCATM techniques.
![Welcome to SCA TM Self-Directed Learning Module If at any point you have questions or technical difficulties, please contact our Knowledge Broker, Terry Kirkpatrick, at [email_address] Let’s get started!](https://image.slidesharecdn.com/scasdlm3-120113112335-phpapp02/75/Supported-Conversation-for-Adults-with-Aphasia-SCA-4-2048.jpg)