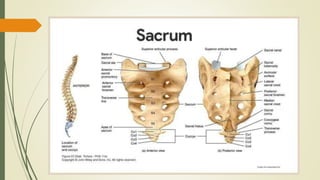
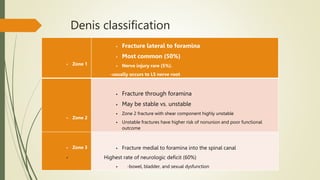
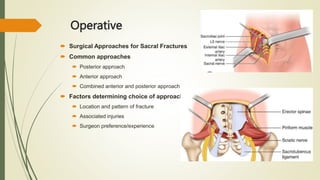
Sacral fractures are common injuries associated with the pelvic ring, often under-diagnosed and linked to neurological issues. Diagnosis typically involves pelvic radiographs supplemented by CT scans for comprehensive evaluation. Treatment options vary from nonoperative to surgical, based on factors such as fracture displacement and associated injuries.