This document provides instructions for nasogastric tube insertion and feeding. Key points include:
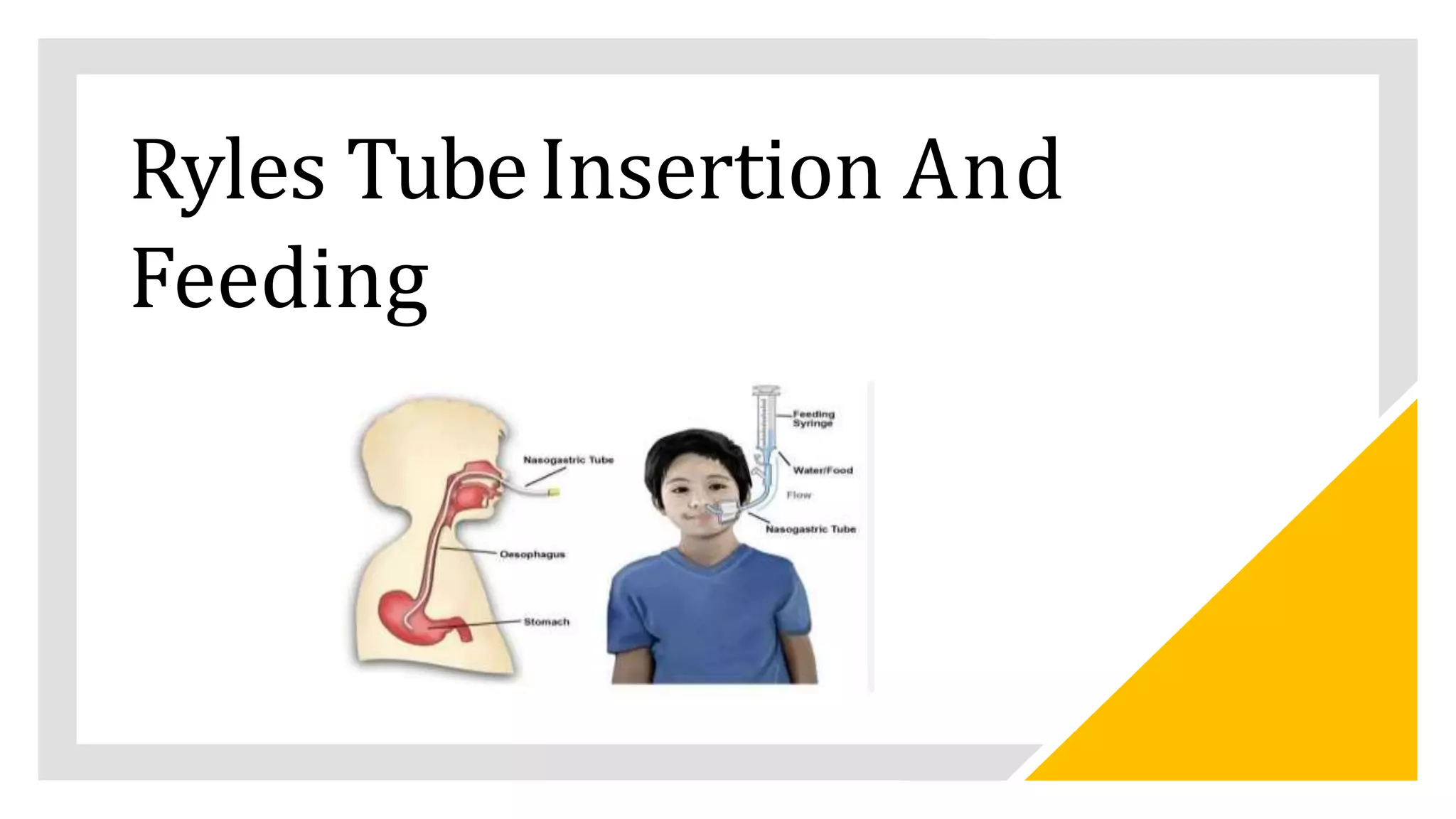
1. Nasogastric tubes are inserted through the nose into the stomach for various purposes such as administering medications or nutrition to patients unable to swallow.
2. The procedure involves measuring the tube length from the nose to earlobe to xiphoid process and lubricating and inserting the tube while the patient swallows. Placement is confirmed with an abdominal x-ray.
3. Feeding administration involves checking residual volumes, administering at a slow rate while elevating the head, and flushing the tube before and after with water or saline. Complications like diarrhea, aspiration, clogging and vomiting are