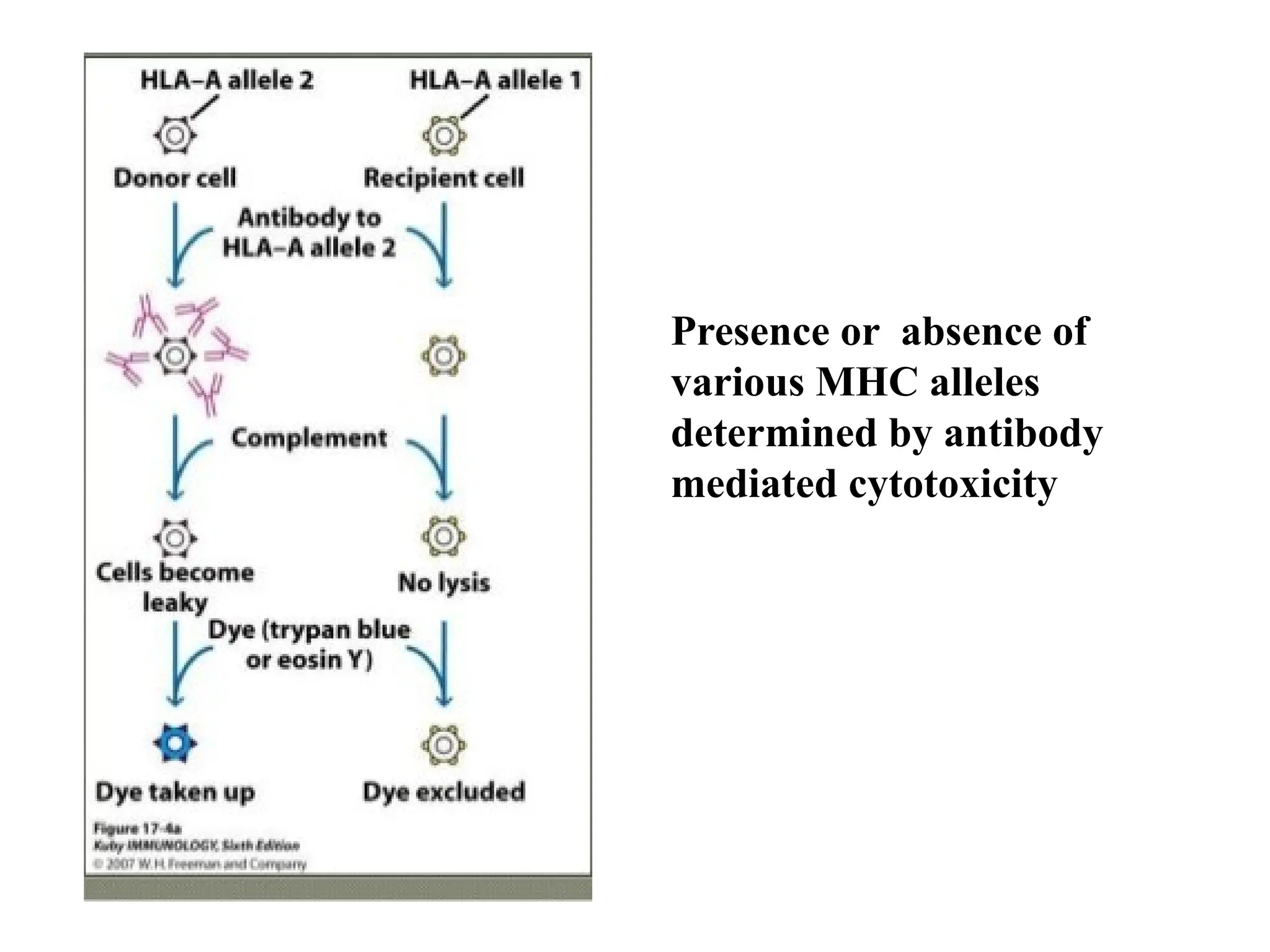
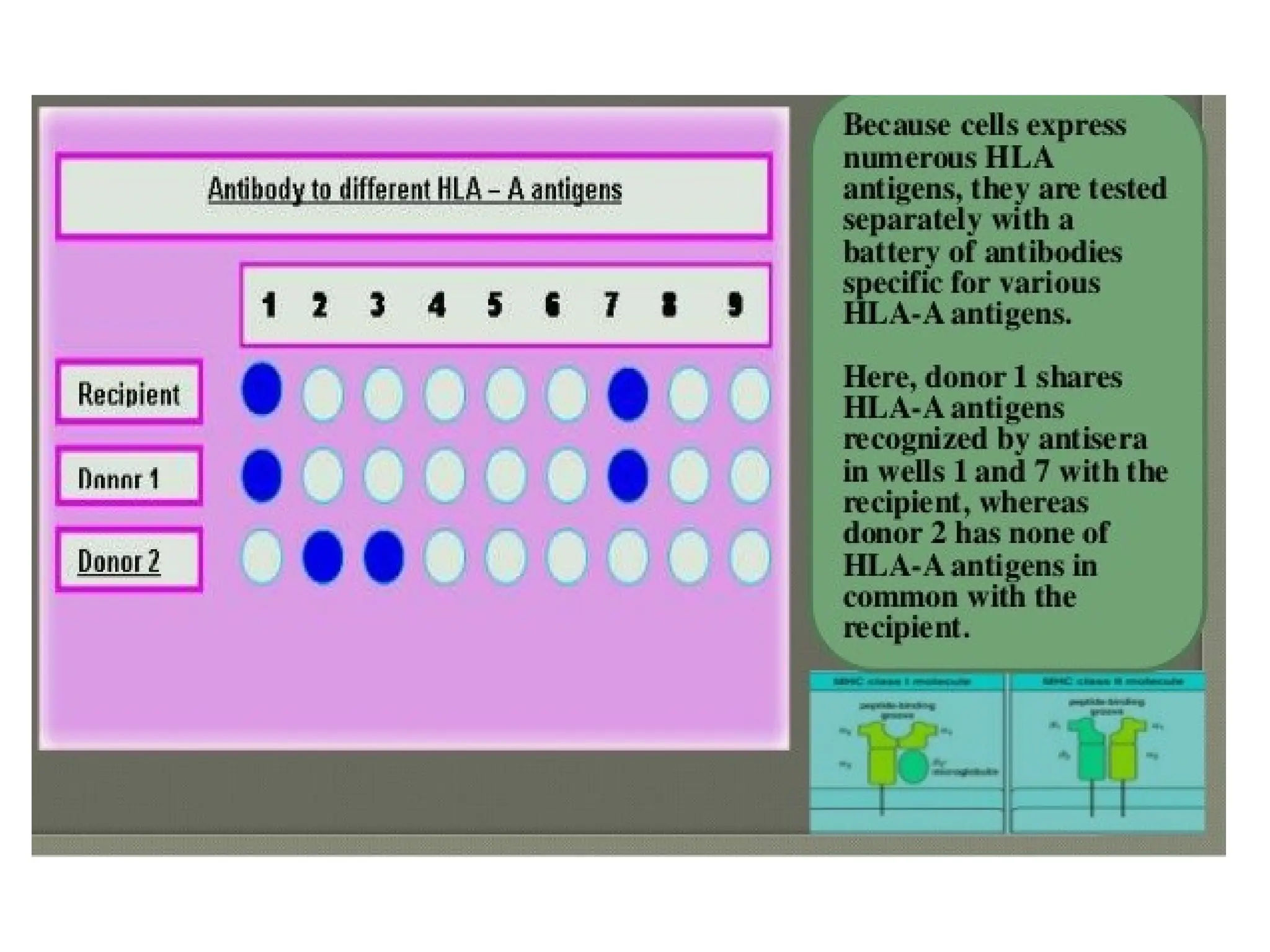
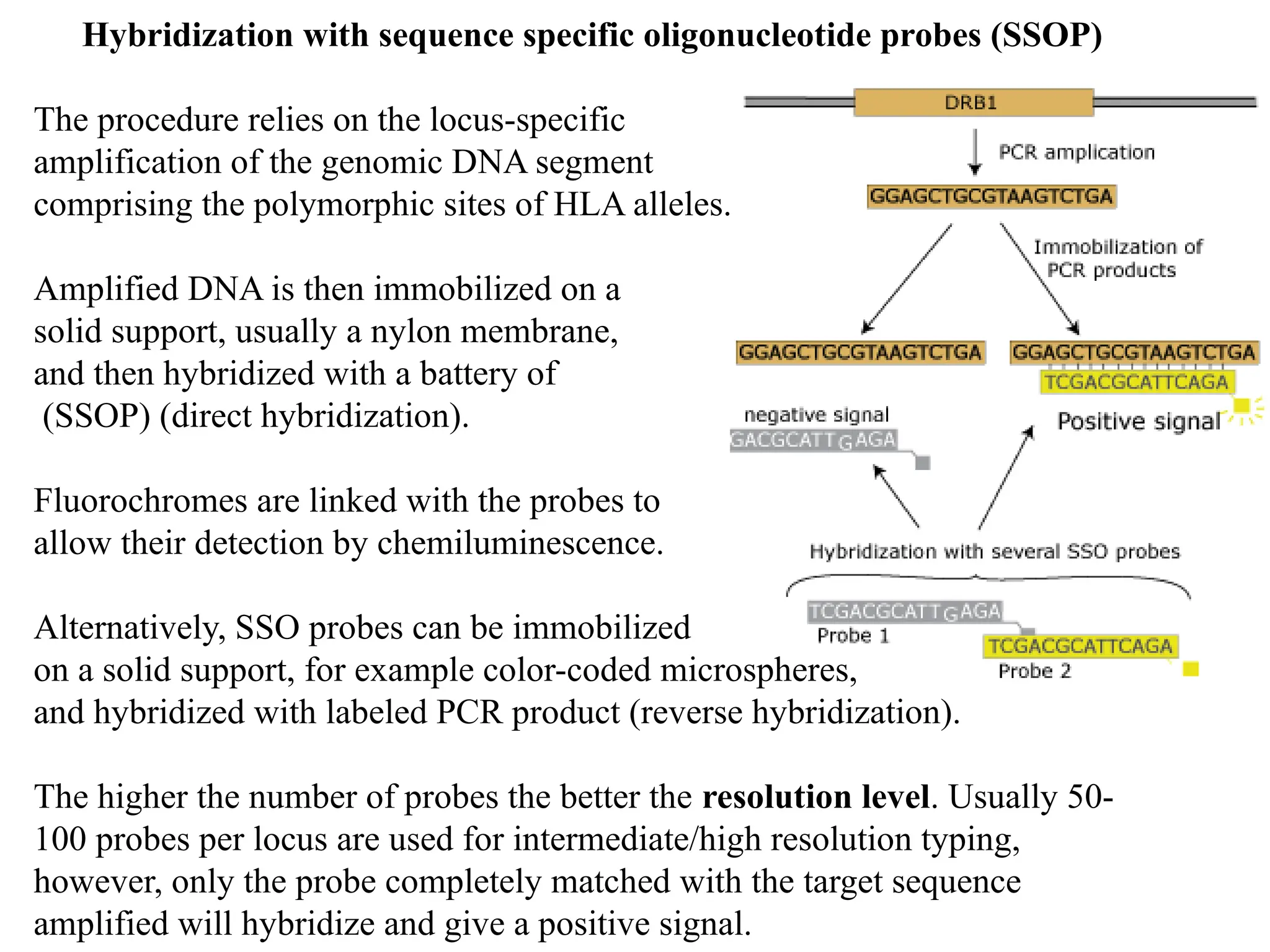
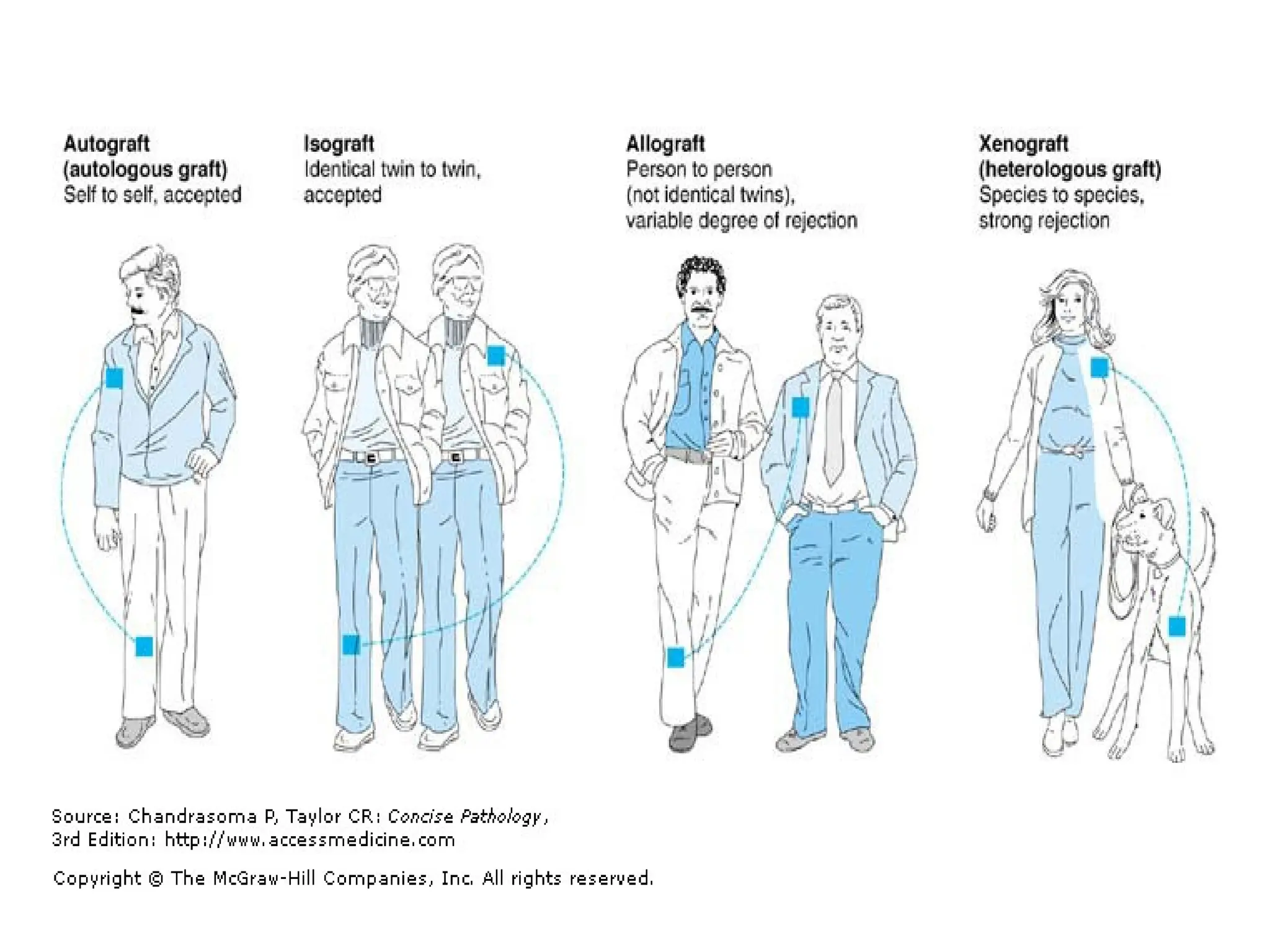
The HLA system comprises a group of genes crucial for the immune system, forming the major histocompatibility complex (MHC) on nearly all cells except red blood cells. HLA typing is essential for identifying compatible tissue and organ donors, particularly for transplants, as it helps ensure a close match between donor and recipient, thereby reducing the risk of transplant rejection. Techniques for HLA typing include serological methods and DNA-based procedures that enhance the accuracy of matching in transplantation scenarios.