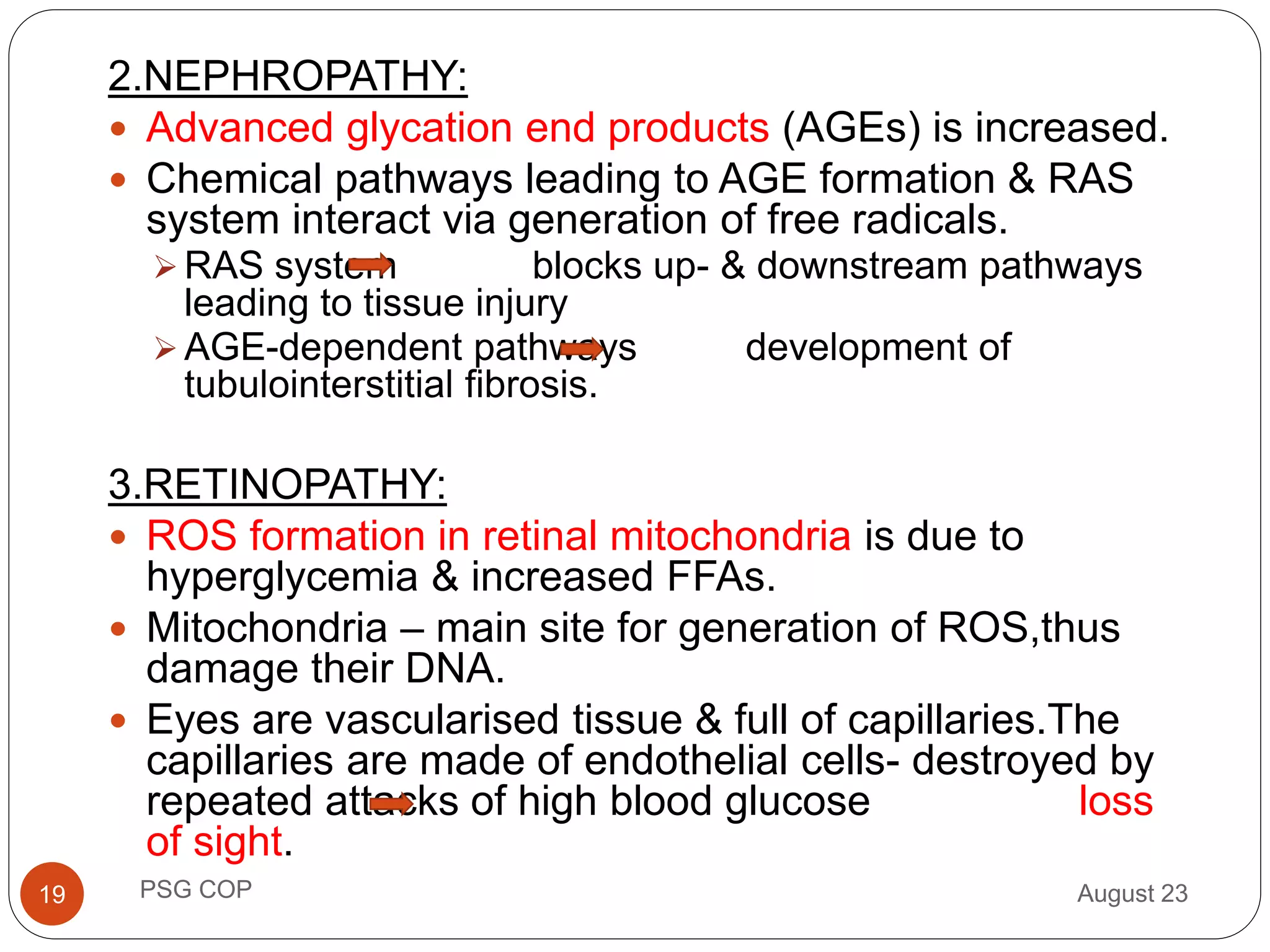
Diabetes is linked to increased oxidative stress which damages cells. High blood glucose in diabetes leads to free radical production through several mechanisms like glucose auto-oxidation and protein glycation. This oxidative stress damages biomolecules like DNA, proteins and lipids in cells like pancreatic beta cells and tissues like retina, nerves and kidneys. It also decreases the body's antioxidant defenses. This cellular damage underlies diabetes and its complications like retinopathy, neuropathy and nephropathy through multiple pathways involving nuclear factor kappa B and protein kinase C activation. Chronic hyperglycemia continuously increases oxidative stress in diabetes and its complications.