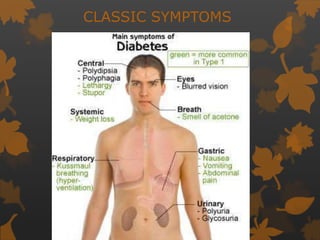
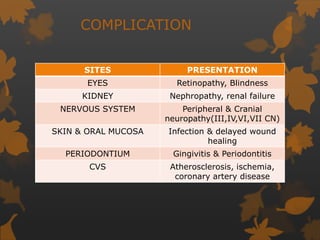
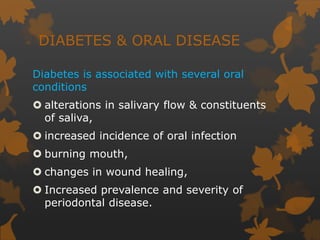
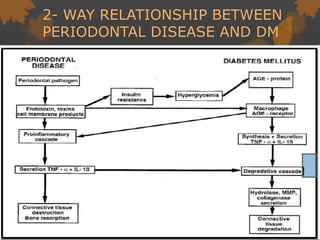
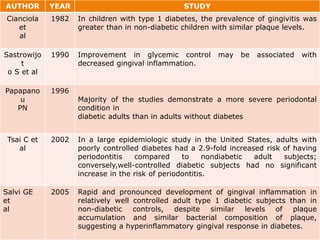
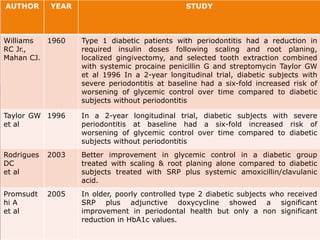
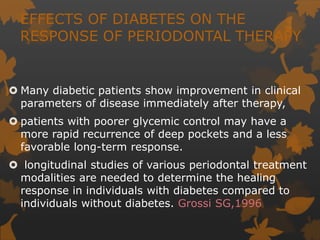
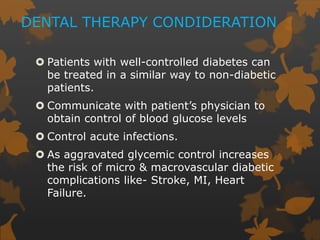
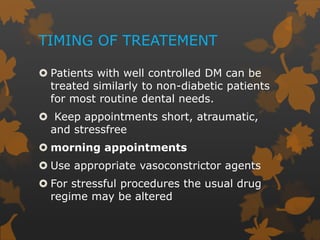
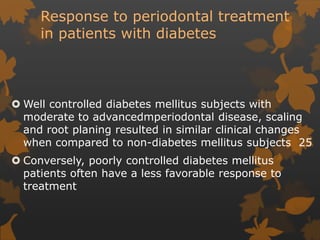
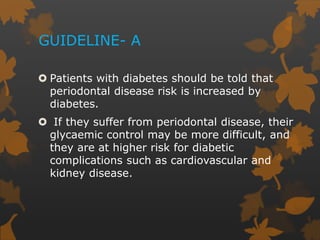
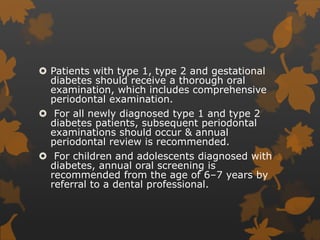
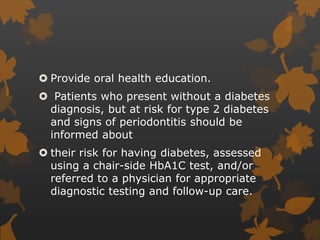
1. Diabetes is associated with increased risk and severity of periodontal disease like gingivitis and periodontitis. Poorly controlled diabetes is linked to worse periodontal inflammation and bone loss.
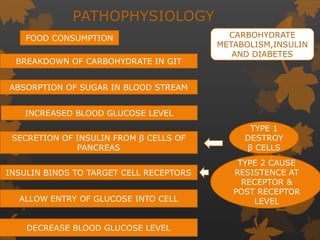
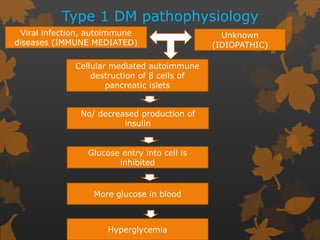
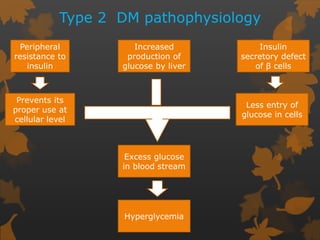
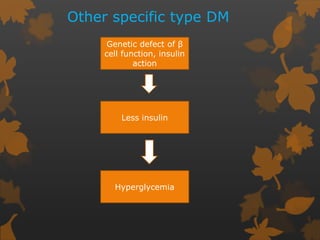
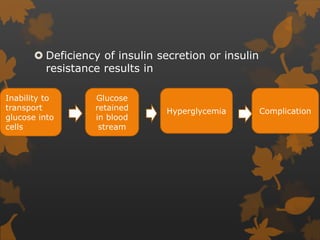
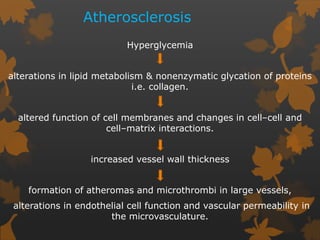
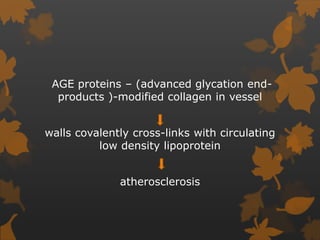
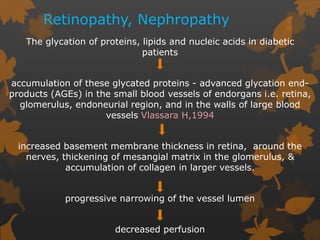
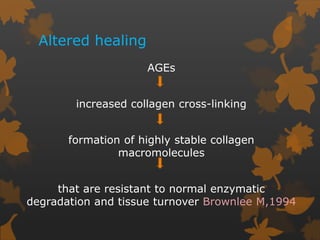
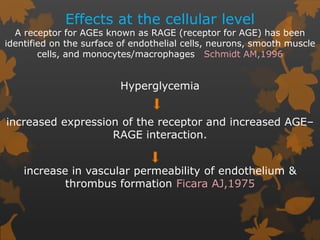
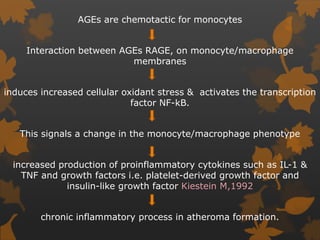
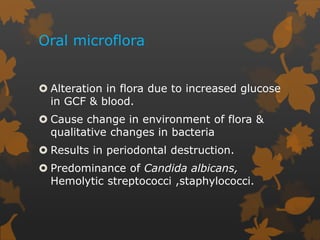
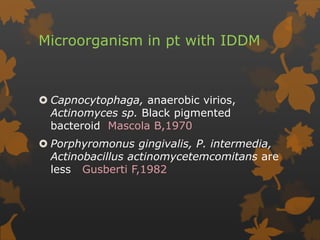
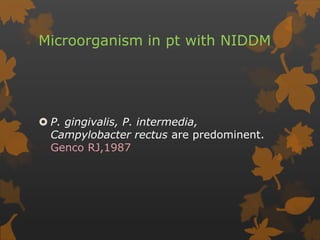
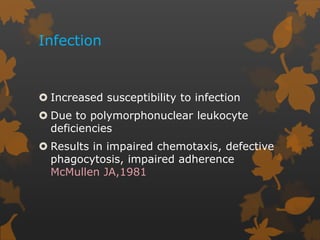
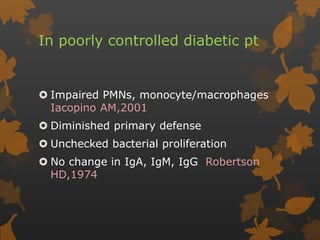
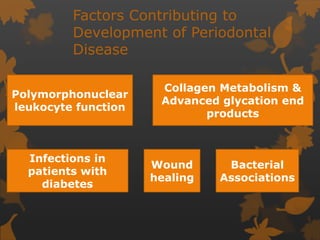
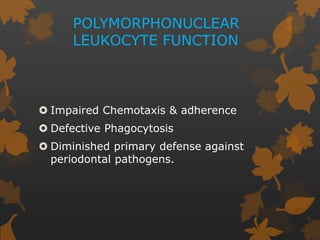
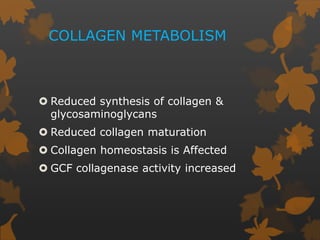
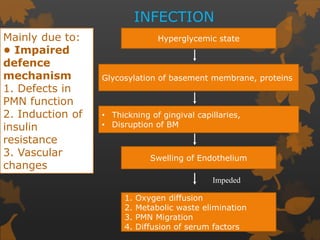
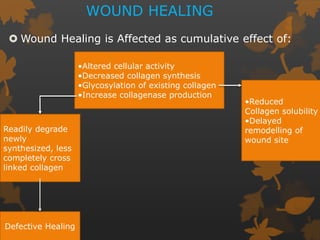
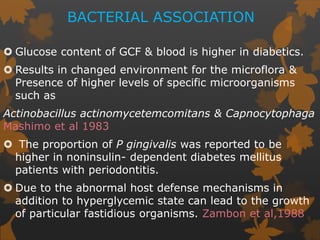
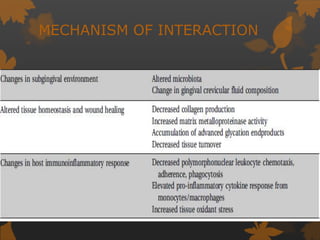
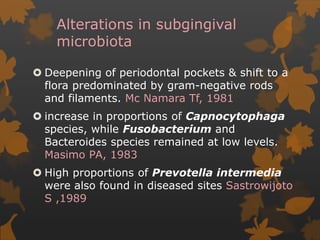
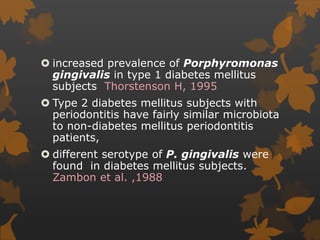
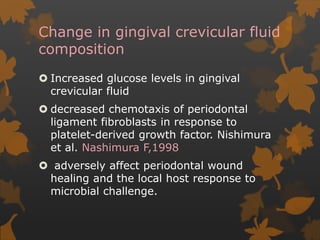
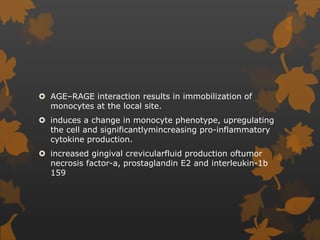
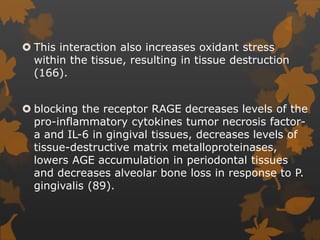
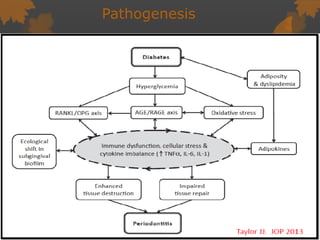
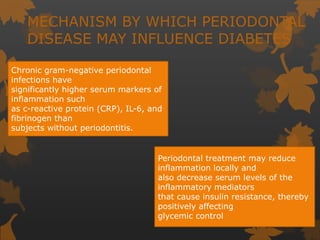
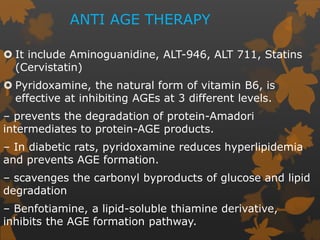
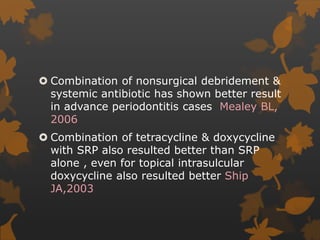
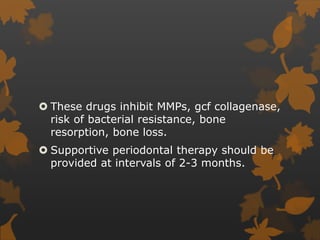
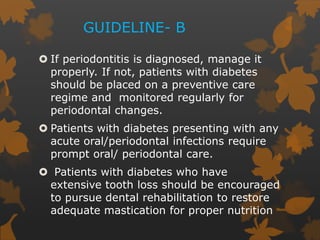
2. The mechanisms involve altered immune response in diabetes that impairs wound healing and increases susceptibility to oral infections. Hyperglycemia also influences the subgingival microbiome and increases non-enzymatic glycation end-products in tissues.
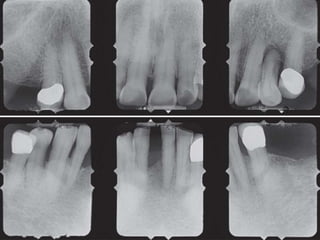
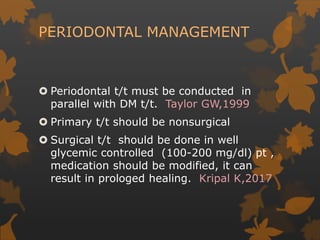
3. Studies found greater gingival bleeding, deeper pockets, more clinical attachment loss, and alveolar bone loss in people with diabetes compared to those without diabetes. Improving blood glucose control can help reduce periodontal inflammation in many cases.