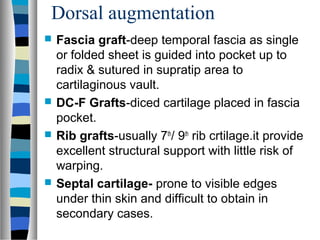
This document discusses external rhinoplasty techniques presented by Dr. Abhineet. It covers indications for external rhinoplasty including reduction/augmentation and trauma/deformities. Pre-op assessment involves standardized photographs. Key anatomical points are defined. Ideal measurements and angles are provided. Techniques for hump reduction, tip work, grafts, and modifications to narrow the base are outlined. Potential complications like hemorrhage, infection and deformities are reviewed. The presentation compares open vs closed approaches and emphasizes achieving symmetry and natural appearance tailored to each patient.