1. The document discusses support in complete denture prosthesis, including definitions, types, importance, anatomical considerations of supporting tissues, and factors affecting support.
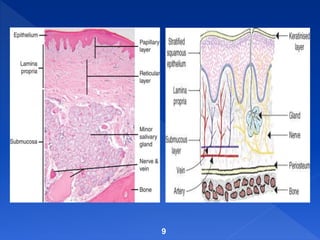
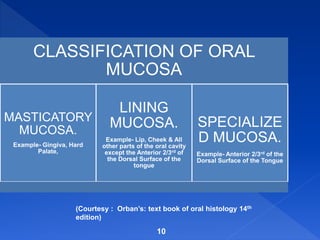
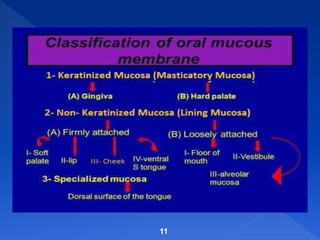
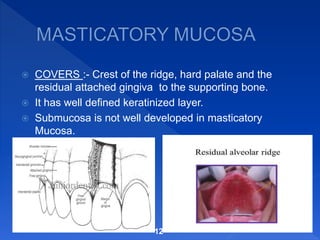
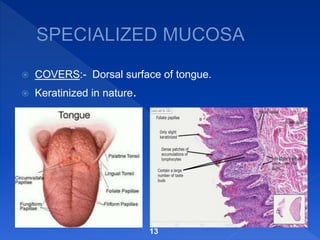
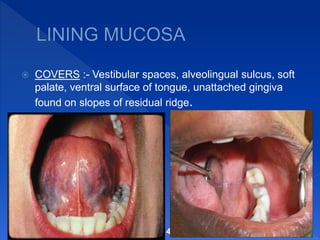
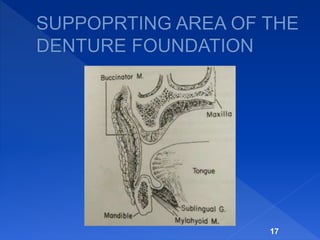
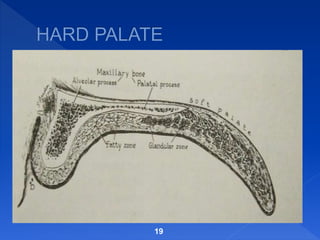
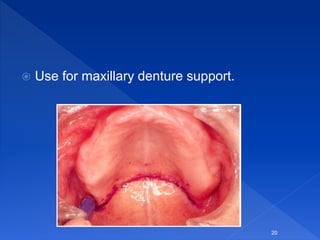
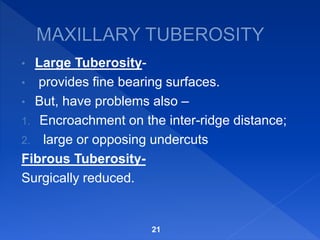
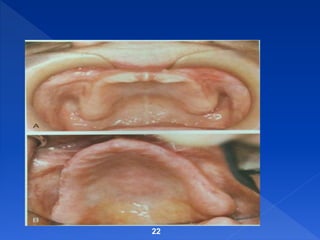
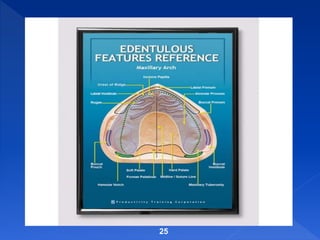
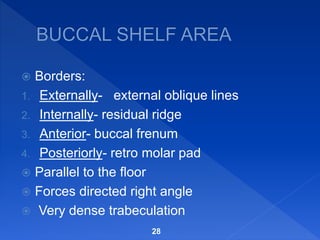
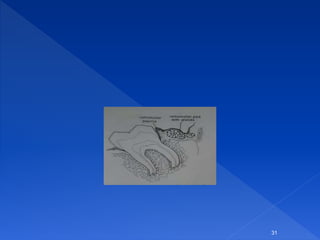
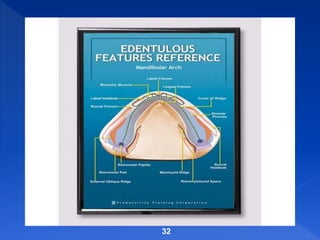
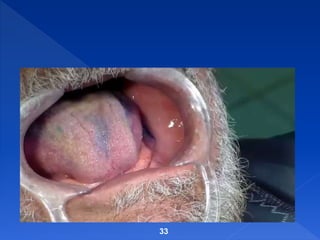
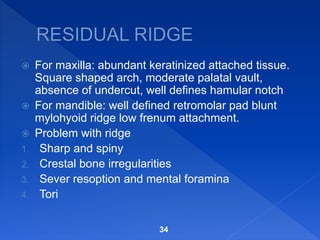
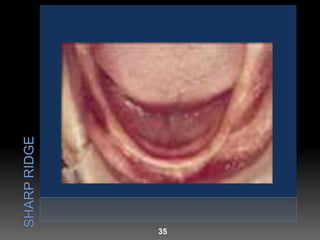
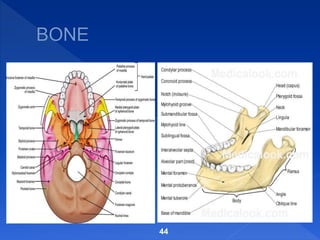
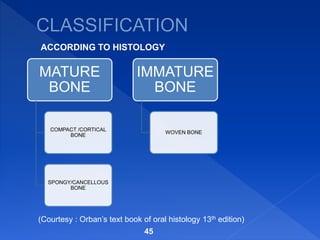
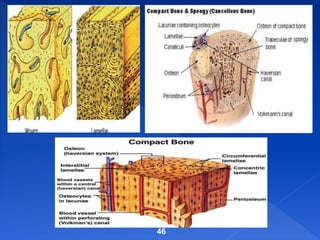
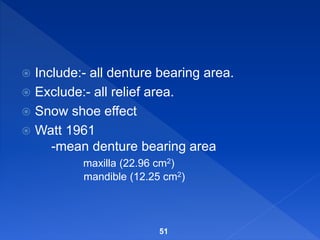
2. Key anatomical considerations for support include the oral mucosa, denture supporting areas in the maxilla and mandible, and bone. Primary stress bearing areas in the maxilla are the hard palate and tuberosities while in the mandible they are the buccal shelf and retromolar pad.
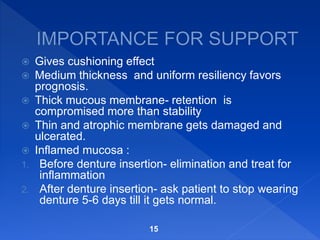
3. Factors affecting denture support include the health of the oral tissues, forces from occlusion and musculature, ridge resorption, and the quality of the impression and denture fit. Support can be improved by techniques that distribute forces






![ 1] Its original size and consistency;
2] the persons general health;
3] forces developed by the surrounding
musculature;
4] the severity the location of periodontal disease
(Hausman ; Hedegard)
5] forces accruing from the wearing of dental
prosthesis;
6] surgery at the time of removal of the tooth;
7] the relative length of the time different parts of
the jaws has been edentulous.
50](https://image.slidesharecdn.com/presentation1supportprostho-170816001956/85/Presentation1-support-for-complete-denture-50-320.jpg)
![1] Recording the tissue impression at their rest position.
2] Decreasing the size of food table.
3] Developing an occlusion that eliminates, as much as
possible, horizontal forces and those that produce torque.
4] Extending the denture base for maximum coverage
within physiologic limit.
5] Biting with the knife and fork, that is, placing small
masses of food over the posterior tooth where the
supporting bone is best suited to resist force.
6] Removing the denture for at least 8 of every 24 hours for
tissue to rest.
53](https://image.slidesharecdn.com/presentation1supportprostho-170816001956/85/Presentation1-support-for-complete-denture-53-320.jpg)