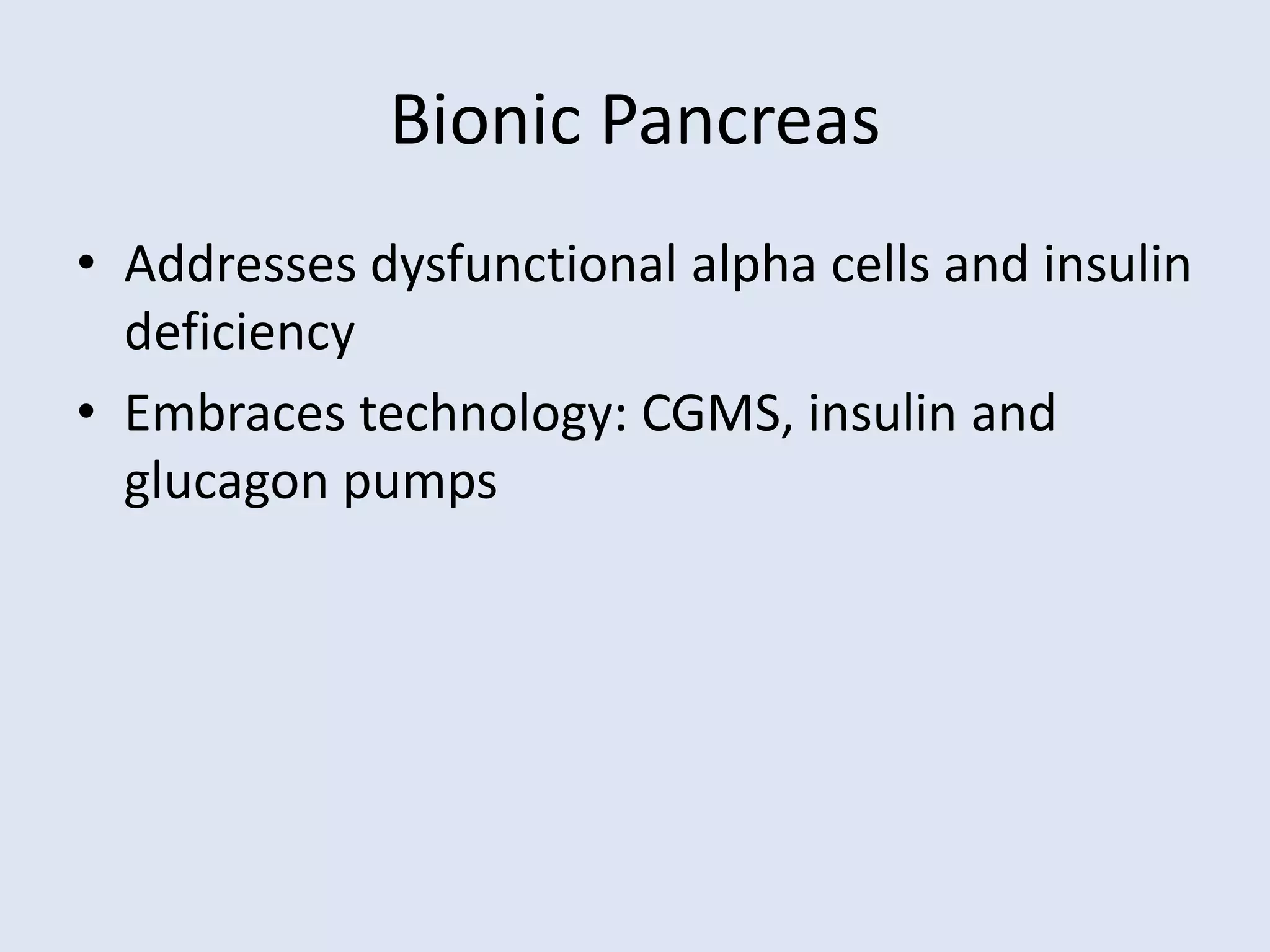
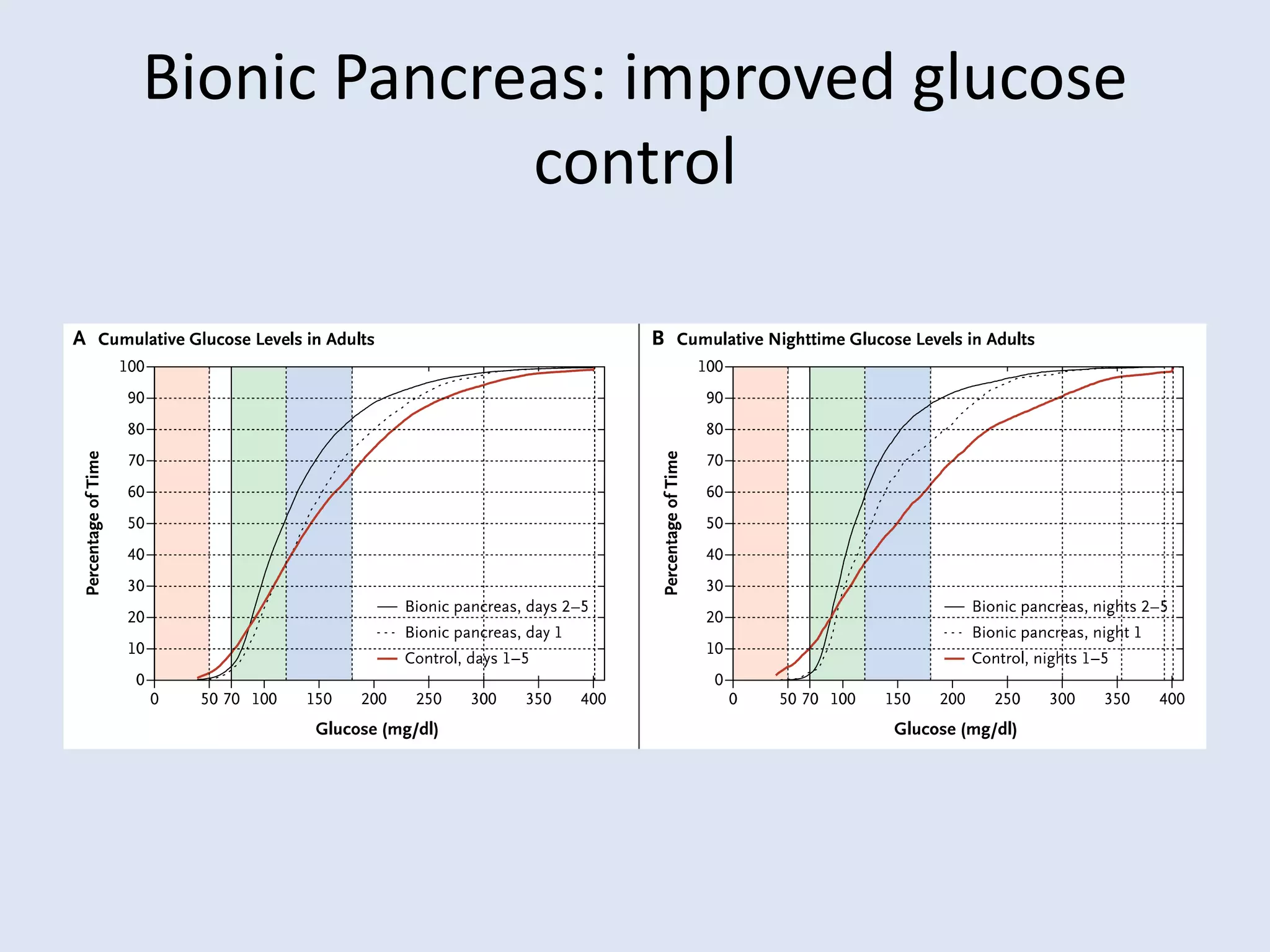
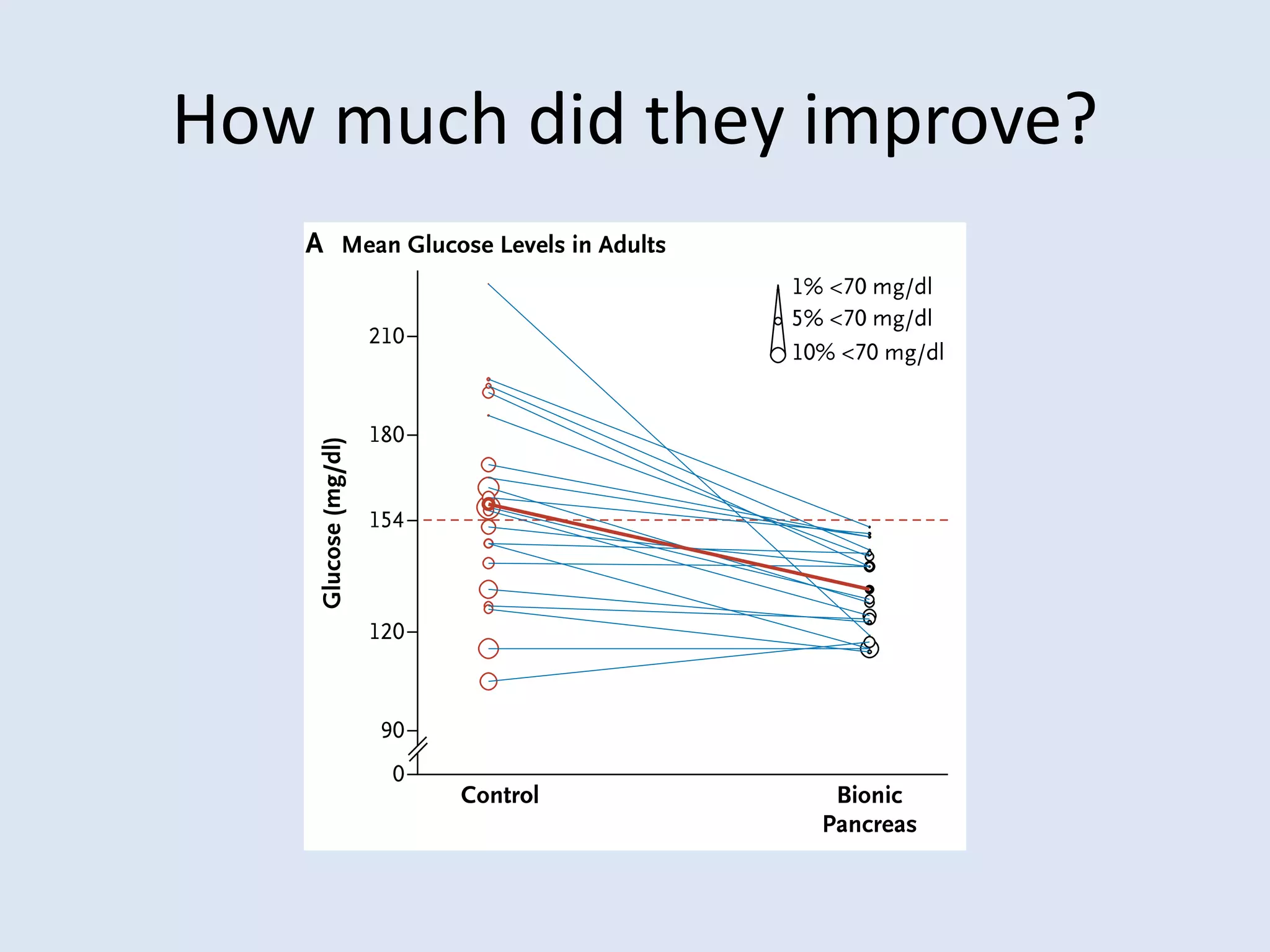
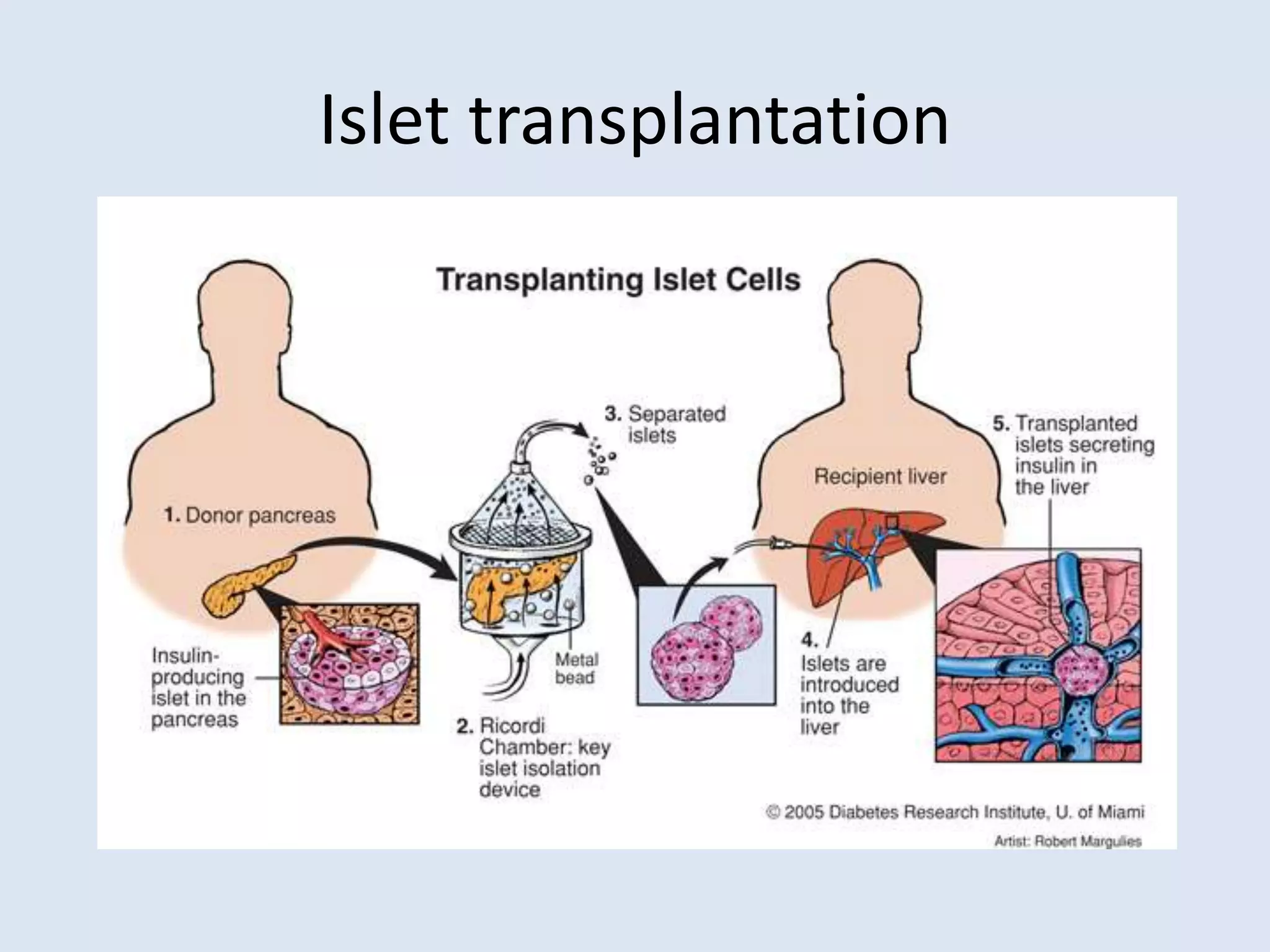
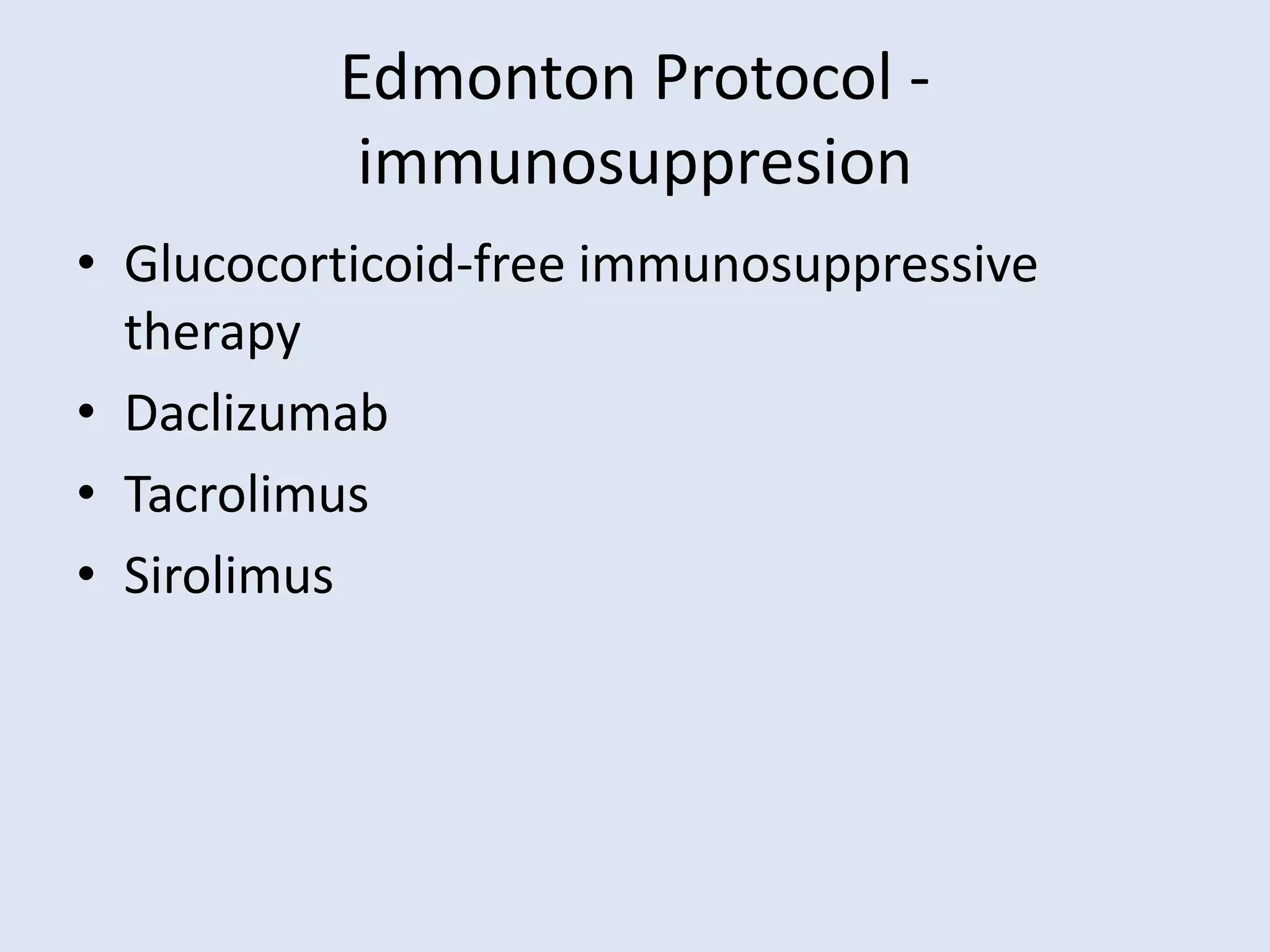
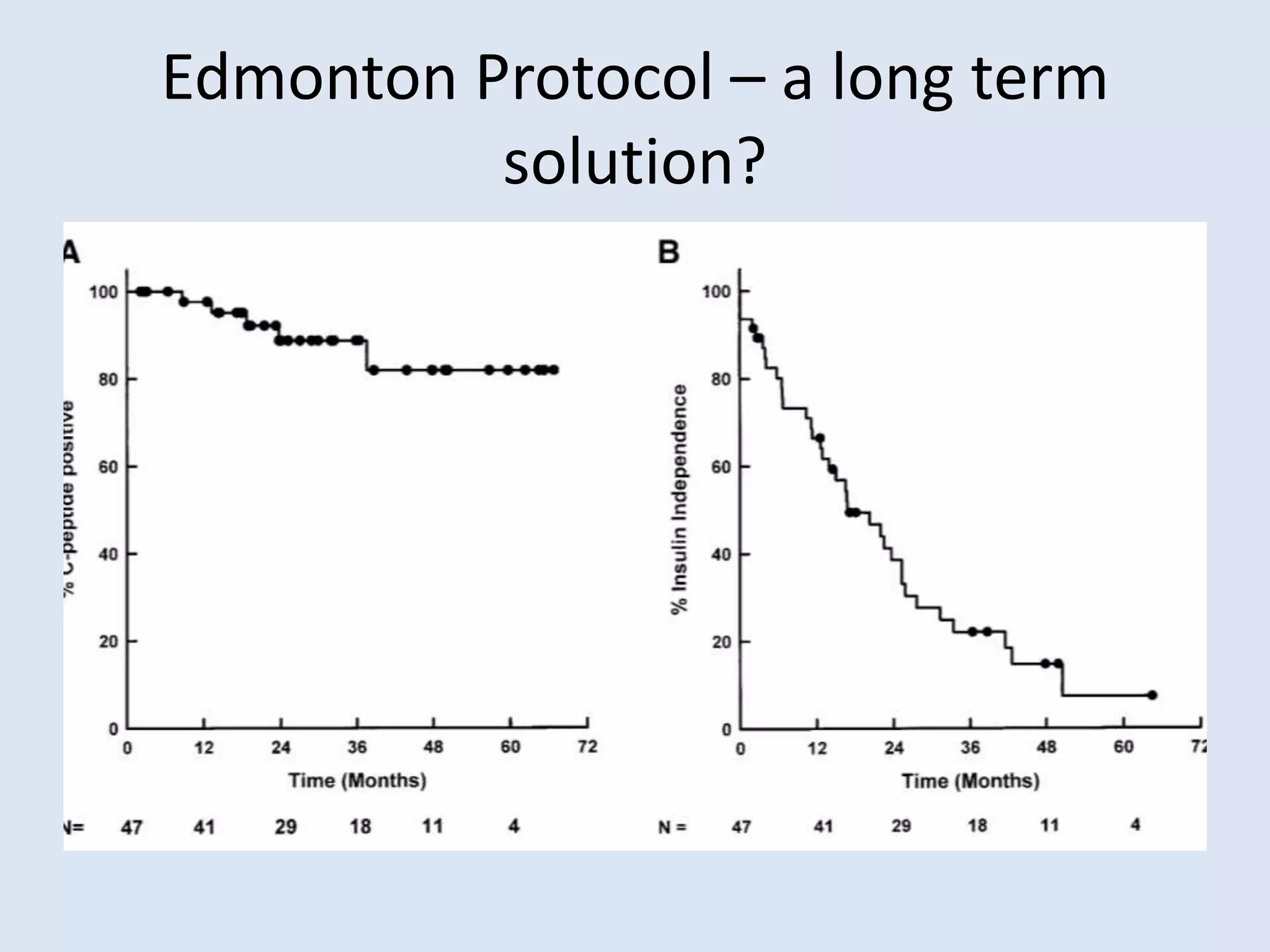
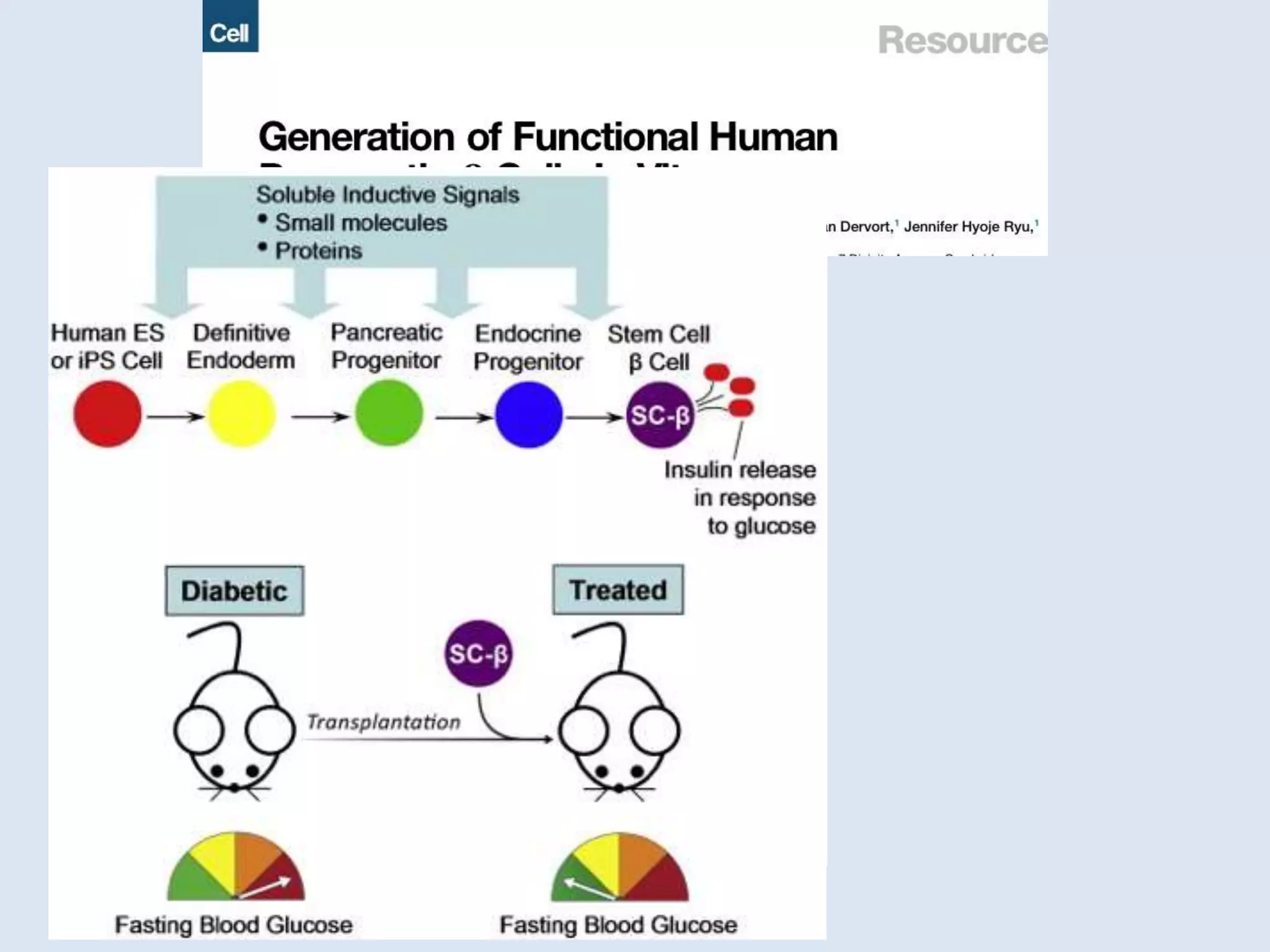
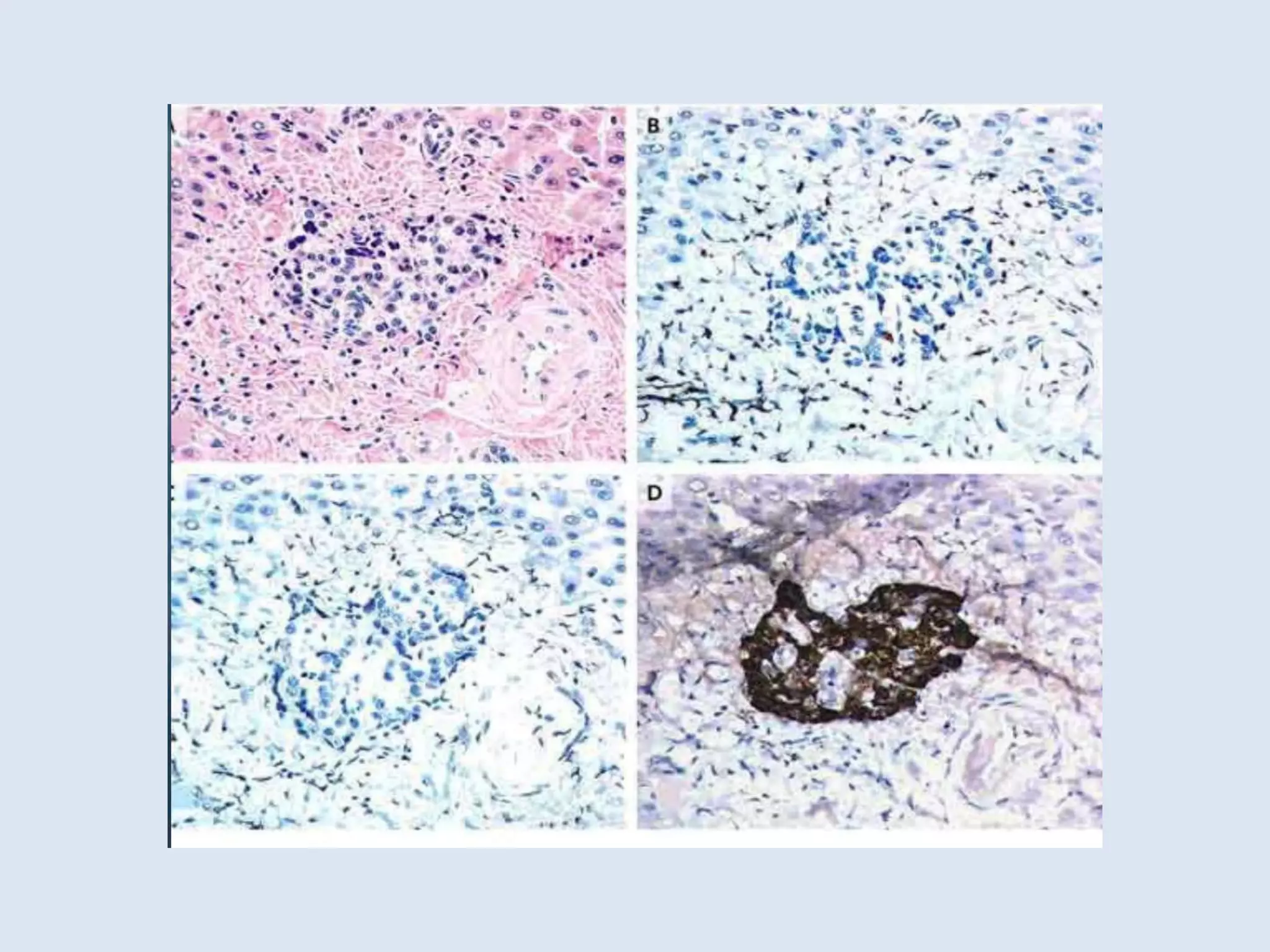
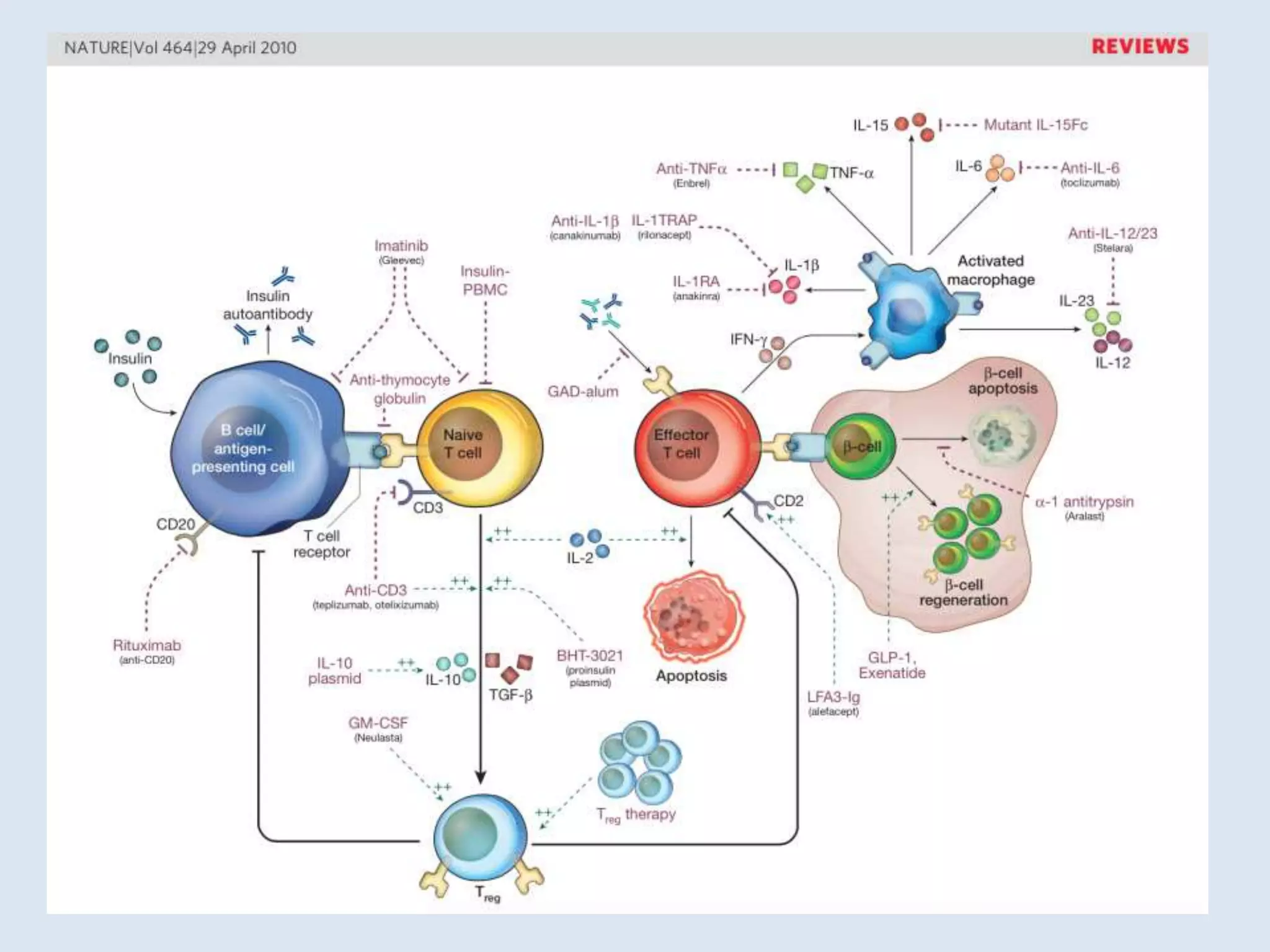
This document summarizes various approaches for managing type 1 diabetes, including the bionic pancreas, islet transplantation, and stem cell therapy. It notes that the bionic pancreas can help improve glucose control but has limitations like being invasive and not physiological. Islet transplantation via the Edmonton protocol can cure diabetes, but challenges remain in expanding the donor supply and improving techniques. Stem cell therapy shows promise if stem cells can be encapsulated to both differentiate into insulin-producing cells and avoid immune rejection. Overall, a cure exists on the horizon, but further progress is still needed to overcome immune issues and increase donor availability.