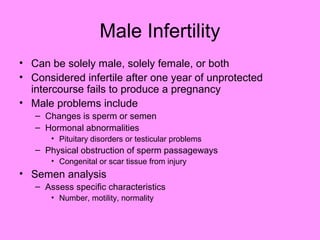
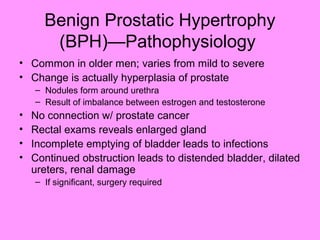
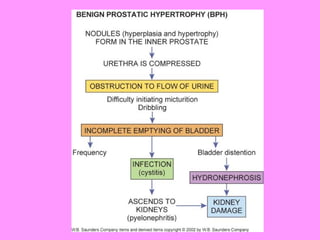
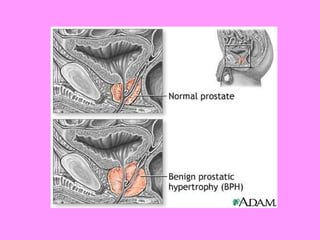
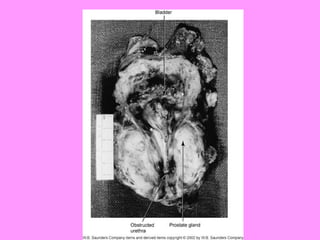
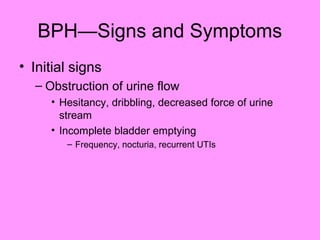
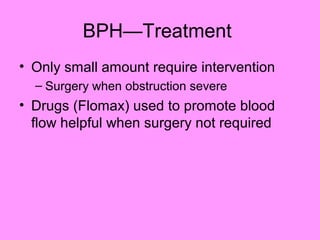
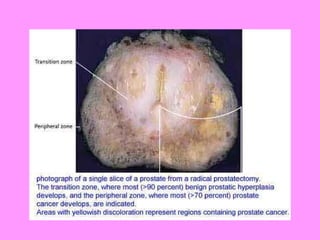
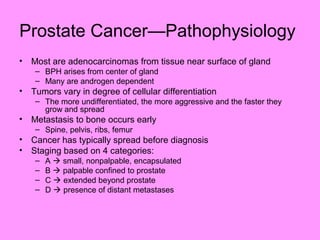
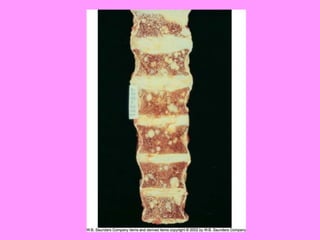
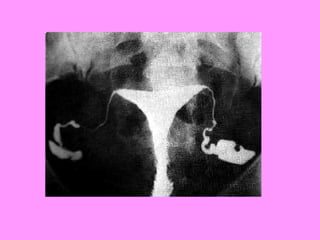
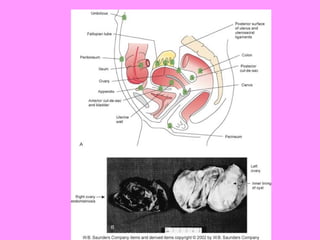
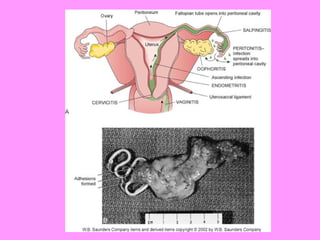
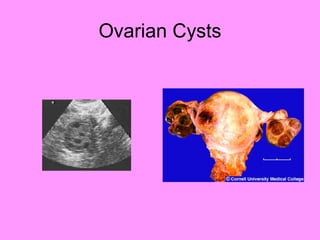
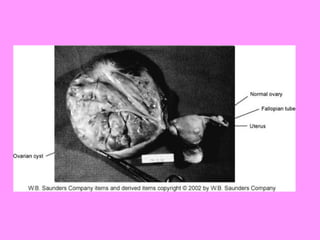
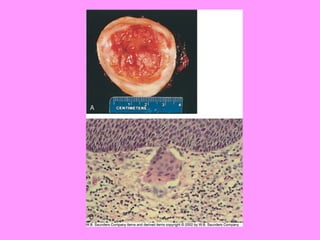
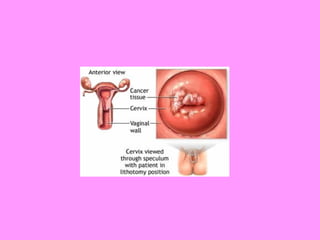
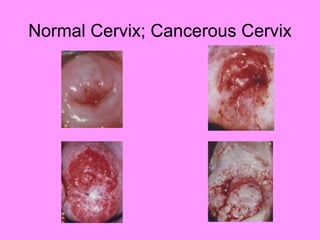
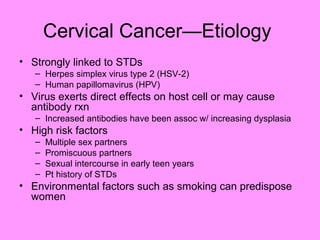
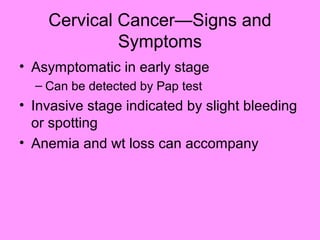
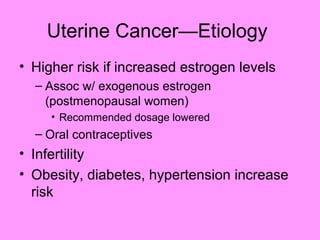
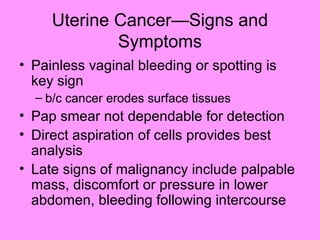
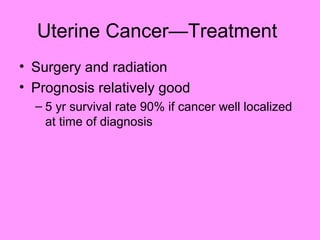
The document provides an overview of various reproductive system disorders, including male and female infertility, benign prostatic hypertrophy (BPH), and different types of cancers such as prostate, breast, cervical, and uterine cancer. Each condition is described in terms of pathophysiology, etiology, signs and symptoms, diagnostic tests, and treatment options. The document emphasizes the importance of early detection and the correlation between hormonal imbalances and reproductive disorders.