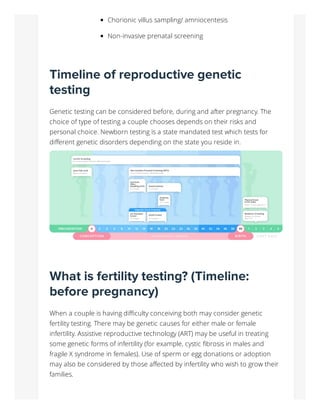
Reproductive genetic testing offers valuable options for couples considering conception or pregnancy, addressing genetic risks and disorders that affect approximately 6% of live births. Key testing types include fertility testing, carrier testing, pre-implantation genetic testing, and various prenatal tests, each tailored to a couple's specific circumstances and timelines. As genetic testing technology evolves, it allows for more informed reproductive health decisions and risk management for future children.