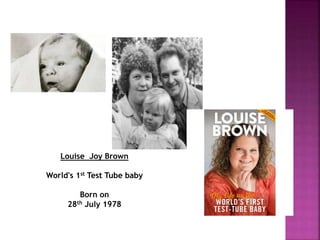
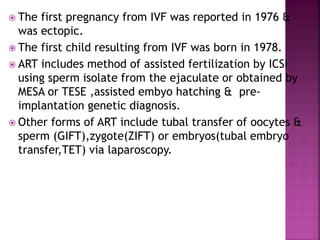
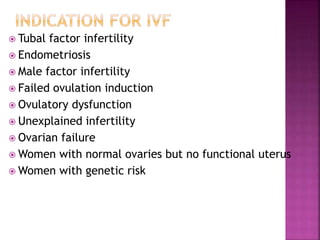
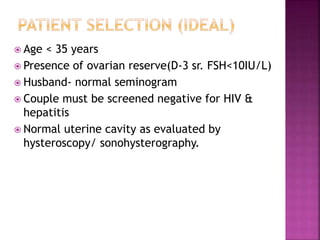
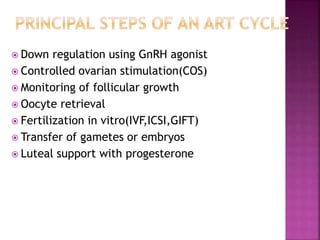
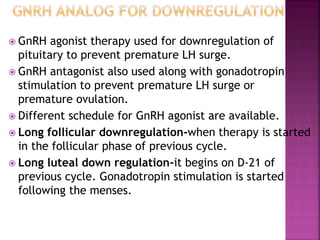
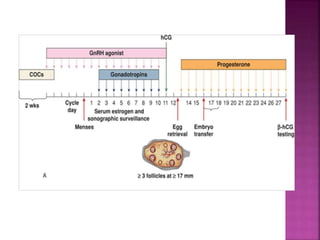
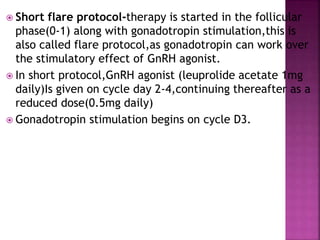
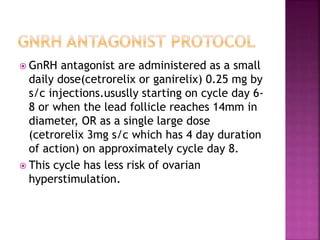
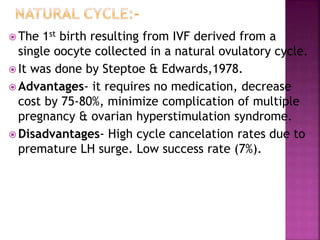
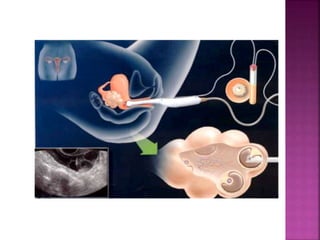
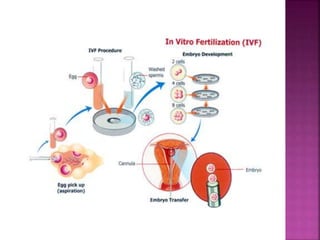
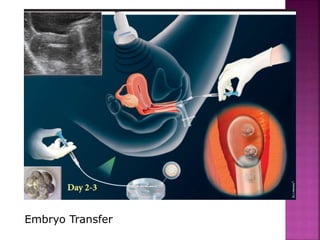
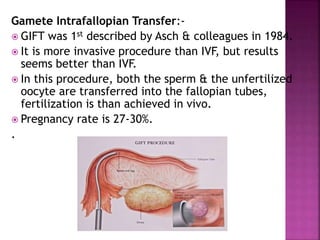
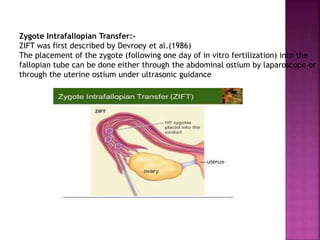
This document summarizes assisted reproductive technologies (ART) such as in vitro fertilization (IVF). It discusses the history and development of IVF, including key events like the birth of the first "test-tube baby" in 1978. It provides details on the IVF process including ovarian stimulation, oocyte retrieval, fertilization, embryo transfer, and luteal phase support. It also discusses other ART procedures and their indications, as well as factors that can influence ART outcomes.