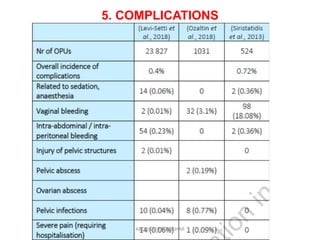
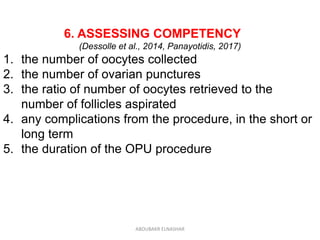
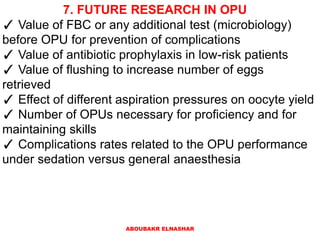
This document discusses the technique of oocyte pickup (OPU). It begins by outlining the basic principles of the OPU technique, including proper patient and operator positioning, transducer handling techniques, and needle guidance. It then provides checklists for ensuring equipment is properly prepared and functioning before and after the procedure. Troubleshooting tips are provided for issues that may arise during OPU like failure of suction or no oocytes retrieved. Assessing competency and areas for future research in OPU techniques are also discussed.