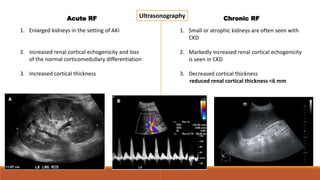
This document discusses renal failure and renal parenchymal disease. It defines acute renal failure as a rapid deterioration in renal function characterized by azotemia and a decline in GFR, which may or may not be accompanied by oliguria. Chronic renal failure is defined as kidney damage or decreased function for 3 or more months resulting in a GFR of less than 60 mL/min/1.17m2. The causes of acute and chronic renal failure are discussed under prerenal, intrarenal and postrenal categories. Imaging findings of various renal parenchymal diseases on ultrasound, CT and MRI are also summarized. Morphological criteria to categorize different renal abnormalities based on ultrasound findings are provided.