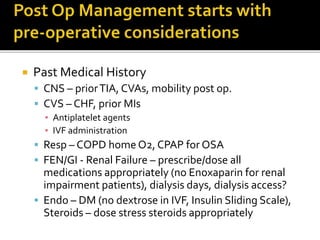
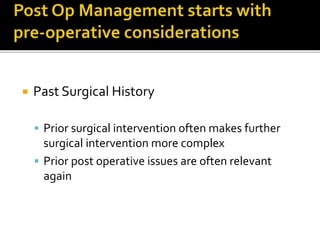
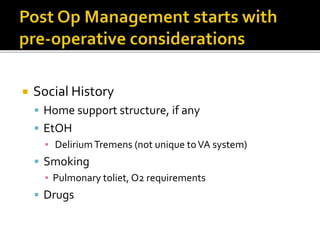
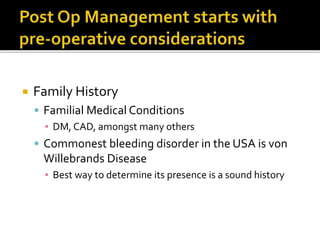
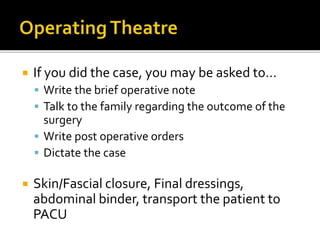
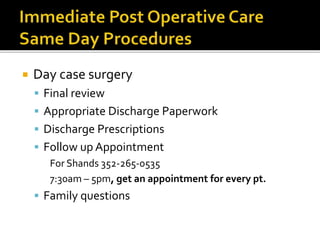
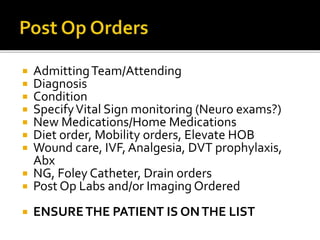
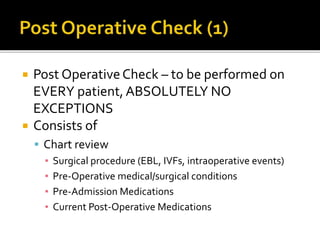
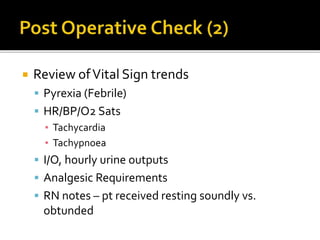
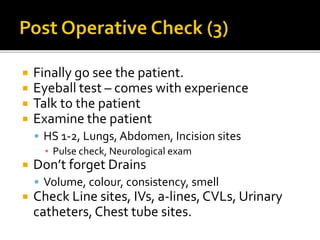
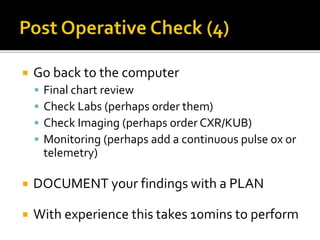
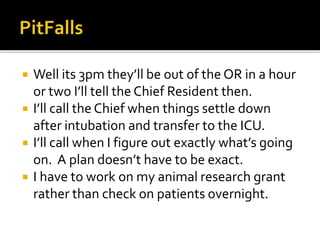
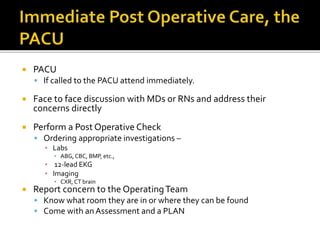
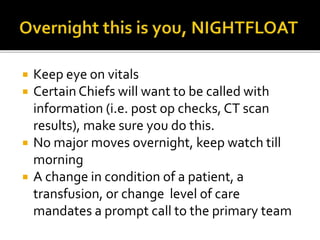
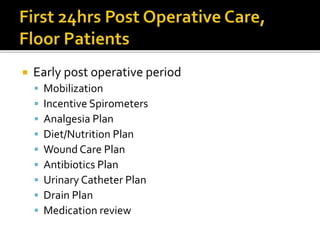
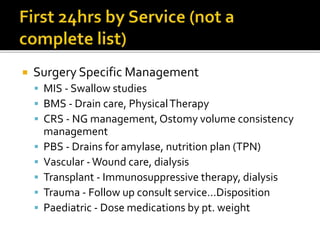
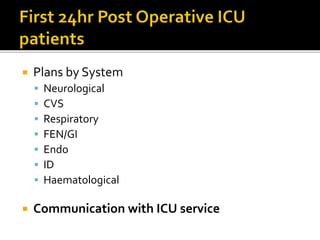
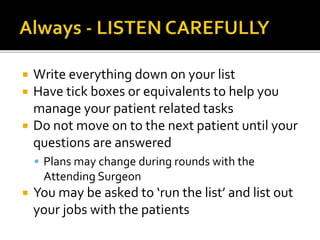
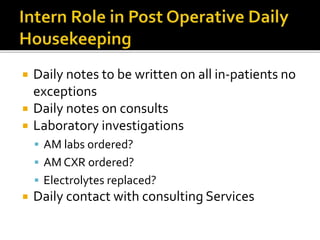
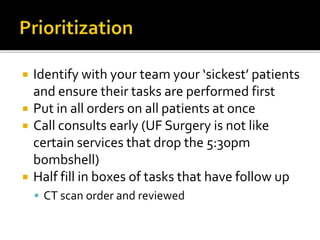
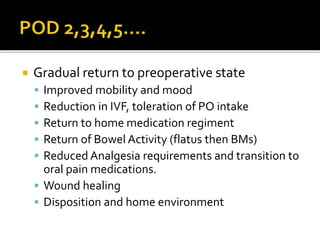
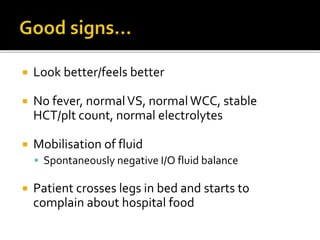
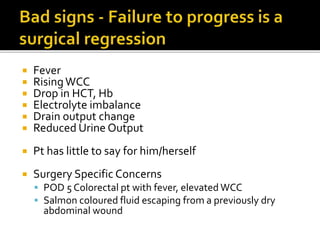
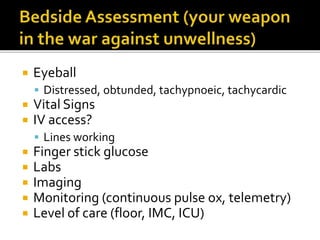
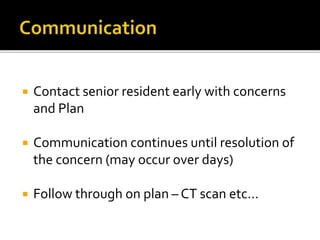
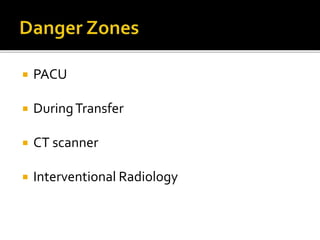
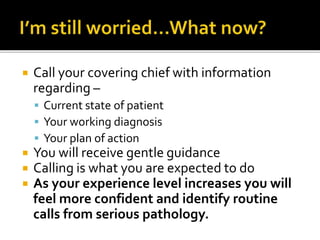
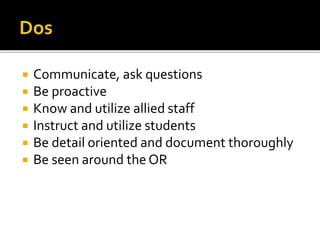
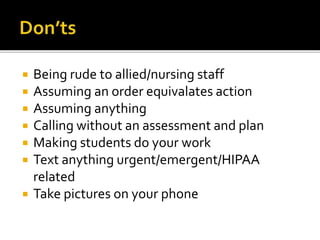
This document provides guidance on post-operative patient management for surgical residents. It discusses evaluating patients in the immediate post-operative period through discharge, including performing post-operative checks, monitoring for complications, communicating with consulting services, documenting care and managing specific post-op issues. Residents are advised to be diligent in their duties and communicate clearly with senior residents and attending surgeons.