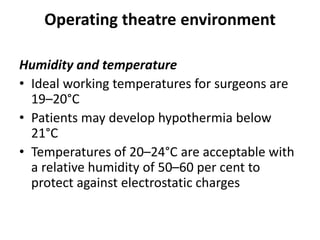
The WHO surgical safety checklist is used universally to improve patient safety and should be completed for every patient, including sign in, time out, and sign out. Risks are minimized through proper preoperative preparation, appropriate antibiotics and VTE prophylaxis, monitoring, positioning to prevent pressure injuries and hypothermia, and strict infection control. The operating theatre is optimized for lighting, ventilation, humidity and temperature. Additional equipment like diathermy and tourniquets require safe usage to prevent complications. Strict asepsis is followed through scrubbing, prepping, draping and limiting personnel movement to minimize infections.