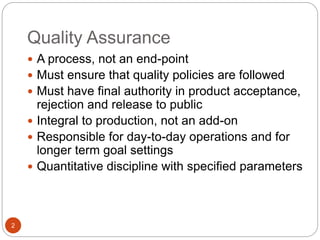
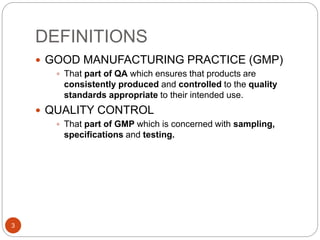
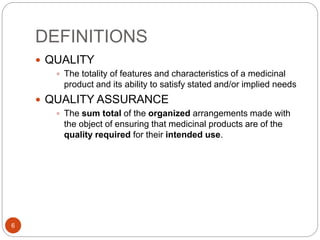
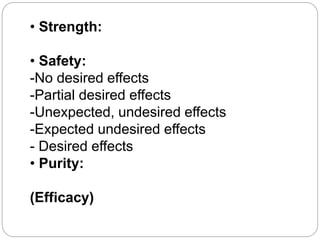
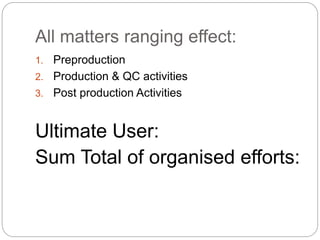
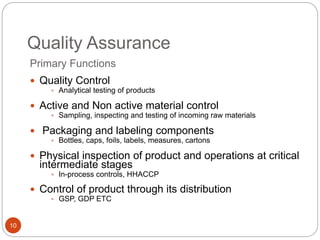
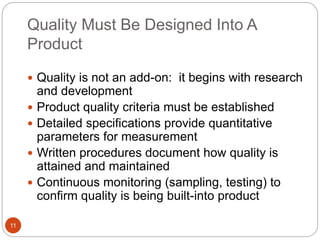
This document discusses quality control and quality assurance in the pharmaceutical industry. It defines key terms like quality assurance, quality control, good manufacturing practices, and outlines the primary functions and elements of quality assurance. Quality assurance aims to ensure pharmaceutical products are of the required quality for their intended use through organized efforts ranging from research and development to post-production activities. It involves monitoring manufacturing processes, facilities, equipment, personnel and documentation.