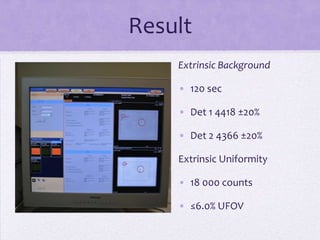
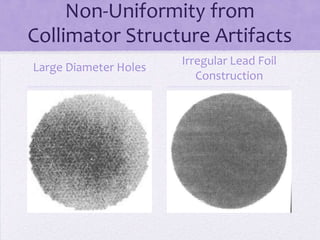
The document outlines the components and quality control (QC) procedures for gamma camera imaging in nuclear medicine, including the collimator, crystal, and photomultiplier tubes. It emphasizes the importance of routine QC tests to ensure imaging accuracy and safety, detailing specific checks such as visual inspections, background radiation assessments, and uniformity tests. Recommendations for daily and weekly QC tests are provided to maintain the integrity of imaging equipment.