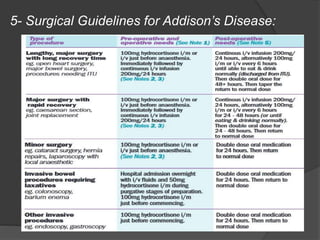
The document provides detailed answers to a series of medical questions related to surgical procedures and conditions. Key topics include laparoscopic inguinal hernia repair, Addison's disease and its management, hydatid cyst diagnosis and treatment, hyperthermic intraperitoneal chemotherapy (HIPEC), lateral scapular winging, and complications from surgery such as gossypiboma. It outlines anatomical structures, pathophysiology, diagnostic methods, treatment options, and preventive measures across various clinical scenarios.