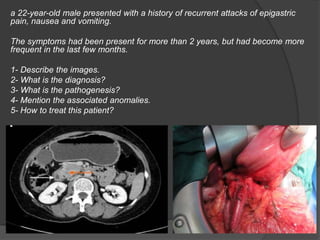
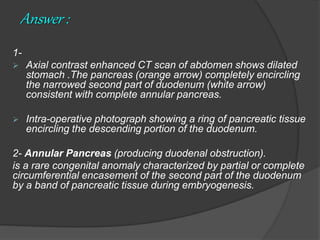
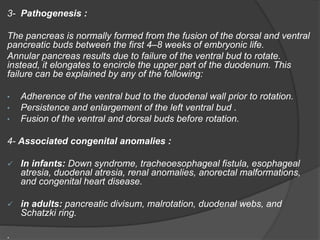
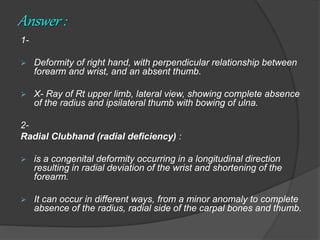
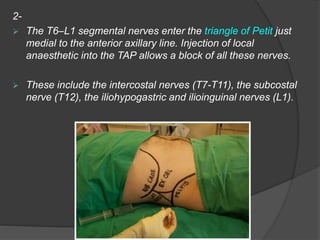
The document discusses various medical cases, including a young male with annular pancreas causing duodenal obstruction, a case of radial clubhand, indications for axillary lymph node dissection, bilateral peritonsillar abscess, and trichobezoar associated with psychiatric disorders. Each case covers imaging results, diagnoses, pathogenesis, associated anomalies, treatment options, and complications. It provides insights into rare congenital anomalies, surgical procedures, and management of specific medical conditions.