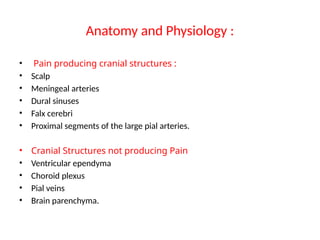
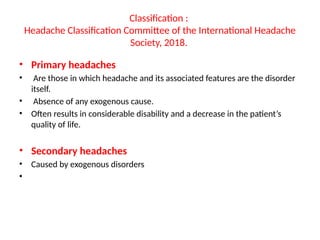
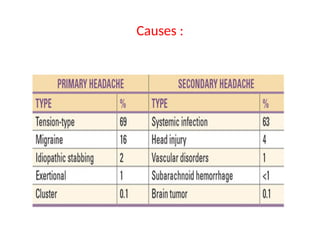
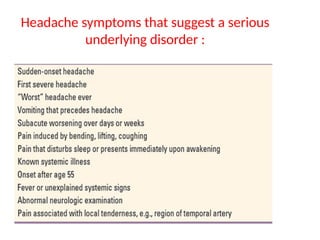
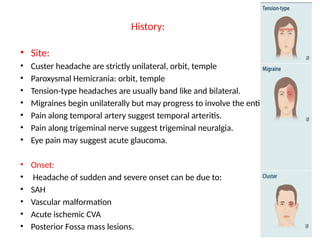
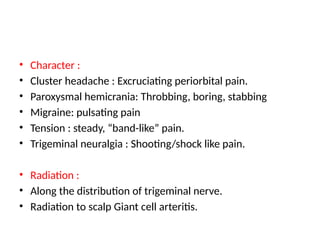
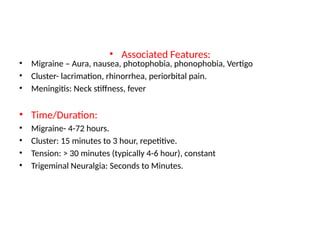
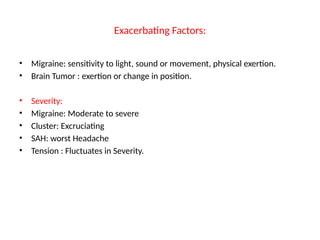
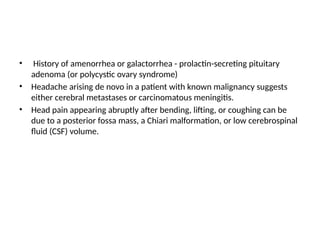
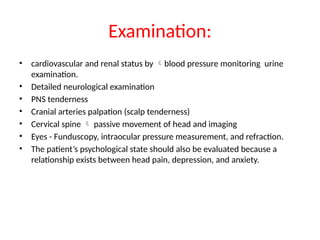
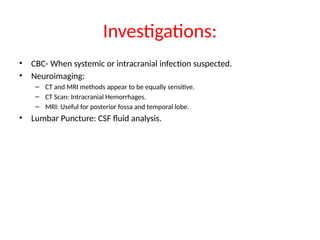
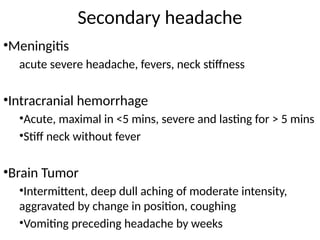
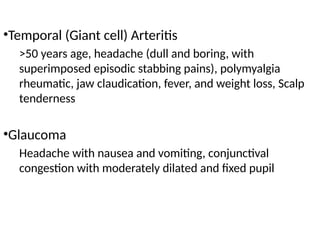
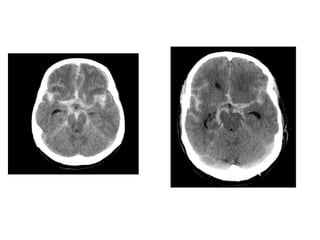
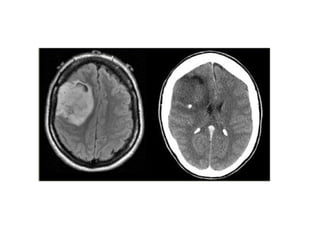
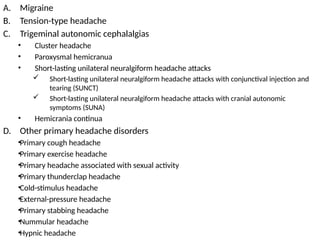
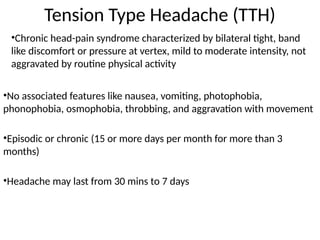
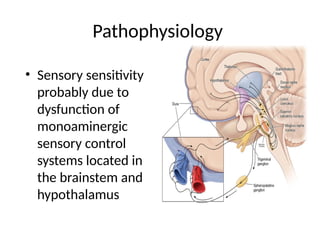
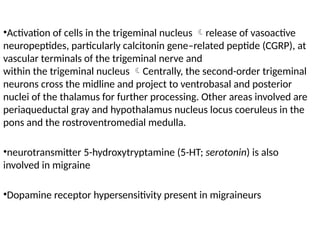
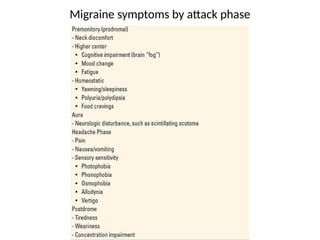
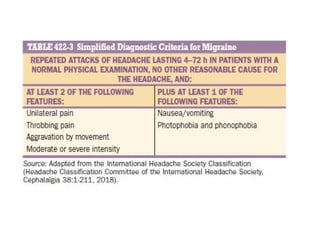
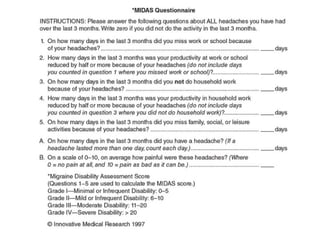
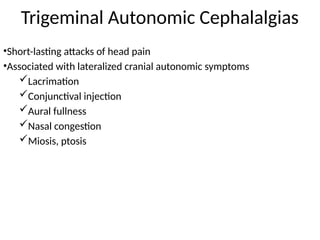
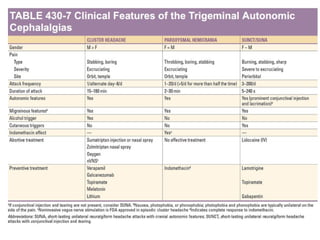
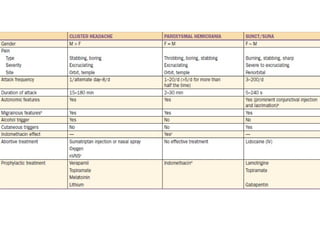
Headaches are a leading reason for medical visits and can be classified into primary headaches, which are the disorder itself, and secondary headaches, caused by other conditions. Symptoms, classifications, and pain characteristics vary greatly among different headache types, such as migraines, cluster headaches, and tension-type headaches, each requiring a specific treatment approach. Diagnostic processes often include thorough history taking, examinations, and imaging studies to determine appropriate management strategies.