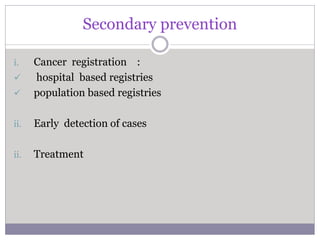
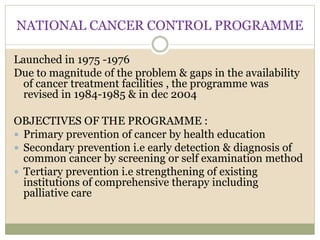
This document discusses cancer control and prevention. It covers risk factors for cancer, approaches to cancer control including primary and secondary prevention, cancer screening methods for breast, cervical and lung cancers, and prevention strategies. Key points include identifying environmental, genetic and lifestyle risk factors; defining primary prevention as preventing cancer occurrence and secondary prevention as early detection; describing screening tests and their limitations for different cancers; and highlighting the importance of controlling tobacco use, immunization, and public education in primary prevention.