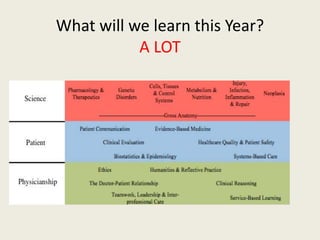
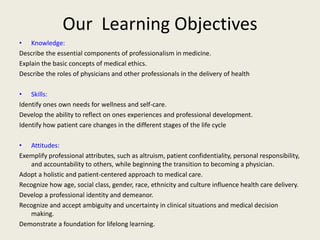
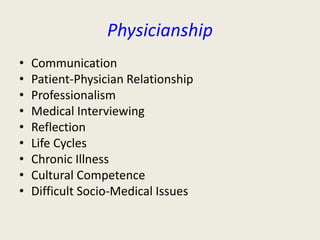
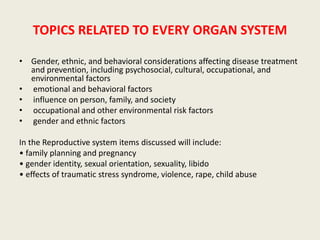
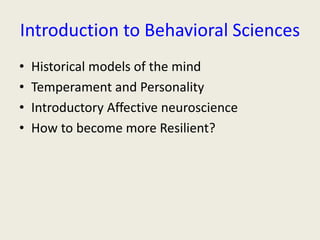
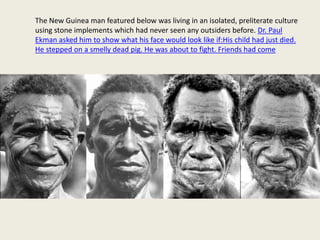
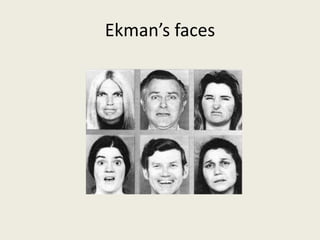
This document outlines the learning objectives and topics covered in an introductory clinical medicine course. The objectives are to develop knowledge of medical ethics and professionalism, clinical skills like self-care and reflecting on experiences, and attitudes like patient-centered care. Key topics include physicianship skills like communication and medical interviewing, the patient-physician relationship, professionalism, the life cycle, chronic illness, and cultural competence. Various teaching methods like lectures, role-playing, patient interviews, and video clips will be used.