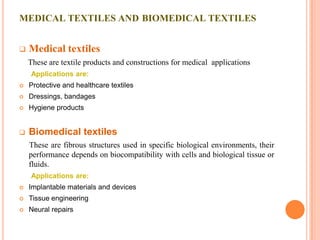
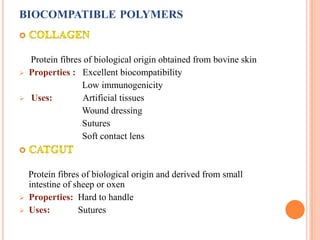
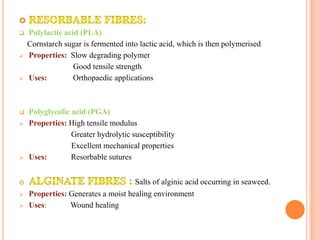
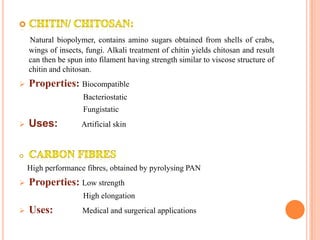
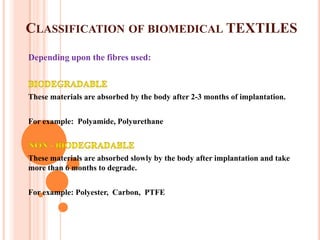
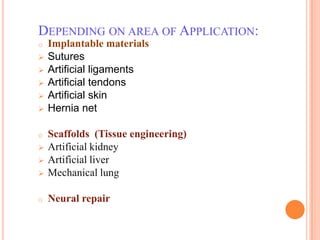
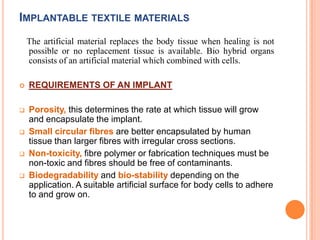
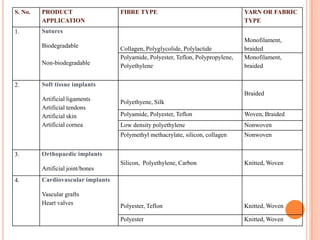
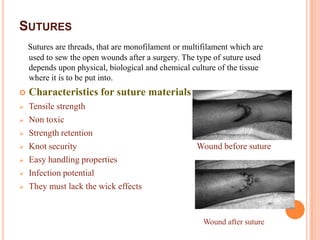
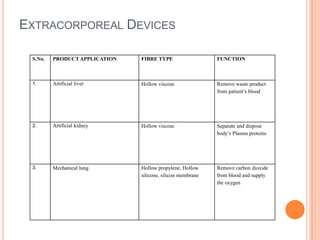
Biomedical textiles are textile products used for medical applications that come into contact with living tissue. They must be biocompatible and biostable. Medical textiles include protective clothing and wound dressings, while biomedical textiles are implantable materials used for tissue engineering and repairs. Biomedical textiles must be designed based on their intended function, biocompatibility, cost, and product approval standards. Common biocompatible polymers used include collagen, silk, PLA, PGA, and chitosan. Biomedical textiles can be classified based on their fibers and applications such as implants, scaffolds, or extracorporeal devices. Key requirements for implants include biocompatibility and appropriate porosity.